All published articles of this journal are available on ScienceDirect.
Measuring Nurses' Uncertainty in Clinical Decision-making: An Integrative Review
Abstract
Background:
There are complexities and controversies regarding the concept of uncertainty in clinical decision-making, making this concept difficult to use.
Objective:
This study aimed to review the definitions and instruments related to uncertainty in clinical decision-making to help researchers select better tools when examining uncertainty in nursing practice.
Methods:
To retrieve the related studies, we searched seven electronic databases, including IranMedex, Scientific Information Database (SID), MagIran, PubMed, Science Direct, Google Scholar, and ProQuest. The COSMIN Consensus-based Standards for the Selection of Health Measurement Instruments (consensus-based standards for the selection of health measurement instruments) was used to determine better tools, and the PRISMA checklist was followed.
Results:
In most of the reviewed studies, the main characteristics of uncertainty were ambiguity, lack of confidence and control, complexity, being on the horns of a dilemma, unpredictability, and unexpectedness. Concerning the measurement tools, despite their acceptable validity, they were mostly measuring uncertainty tolerance.
Conclusion:
According to the results of the reviewed studies, the available tools were not specifically dedicated to measuring the uncertainty of nurses in clinical decision-making. A suitable tool can be helpful in measuring nurses' awareness about their degree of uncertainty in decision-making and nursing managers' awareness about nurses' uncertainty, thereby helping in planning to reduce the complications caused by nurses' uncertainty in clinical decision-making. Hence, it is necessary to develop suitable tools.
1. INTRODUCTION
There are several definitions for the concept of uncertainty in different disciplines. This concept has been studied and defined in the classical probability theory and has also been used in decision-making theories. According to decision-making theorists, uncertainty is defined as a situation where people cannot precisely predict the risk of events or expected outcomes [1], most often because of exposure to an ambiguous situation [2]. Uncertainty typically occurs in situations that might be associated with an unpleasant outcome, but the event's probability cannot be estimated [3].
The ability to detect and handle uncertainty is an essential skill for all healthcare providers [1]. An uncertain situation can keep nurses in doubt, delay their clinical decisions, postpone their interventions, and make them dissatisfied with their decisions. Embracing uncertainty, on the other hand, can be a learning opportunity. In this situation, nurses try to exercise their critical thinking and clinical reasoning skills to make effective clinical decisions [4].
In the process of patient care, clinical decision-making can be defined as the selection of the best clinical option [5]. Making a sound clinical decision involves processing information; using knowledge, critical thinking, and problem-solving skills; assessing evidence; and reflecting and using clinical judgment to select the best course of action to enhance the client’s health and reduce potential risks [6]. Nonetheless, the nurses’ uncertainty in their clinical decisions can result in emotional reactions, agitation, fear, burnout, frustration [7], and reduced job satisfaction and self-esteem [2]. Uncertainty in nursing practice may also directly affect patient care and influence the nurse’s decision to continue working in a particular unit [2]. Unresolved uncertainty and the resulting stress can potentially affect the quality of care and patient outcomes [4].
A precise definition of a concept is the prelude to finding a way to measure it. However, complexities and controversies regarding the concept of uncertainty in clinical decision-making make this concept difficult to conceptualize and operationalize [8]. In addition, measuring and reducing uncertainty plays an essential role in developing nurses' ability to make effective clinical decisions.
Given the consequences of uncertainty for patients and nurses, this study reviewed the definitions and instruments used to measure uncertainty in clinical decision-making to summarize the existing knowledge for future studies.
2. MATERIALS AND METHODS
To achieve the study aims and have a more comprehensive and accurate understanding of the concept, we conducted this integrated review study based on Broome’s method in three stages of the search process, critical evaluation of the research, and analysis and synthesis [9].
2.1. Search Process
At this stage, we searched for relevant studies in seven electronic databases, including IranMedex, Scientific Information Database (SID), MagIran, Science Direct, PubMed, Google Scholar, and ProQuest. Our search was restricted to papers published in English and Persian languages after 1990. The search terms were defined based on the research question and the inclusion criteria. We used a combination of keywords and Boolean operators to retrieve relevant studies from the database. The keywords were “nurse” AND “uncertainty” AND “decision-making” AND “instrument” OR “tool” OR “scale” OR “questionnaire”. We also used truncation () and wildcard (?) symbols to expand the search results. For example, we searched for “nurs” to include “nurse”, “nurses”, “nursing”, etc. and “decisio?” to include “decision” and “decisions”. We also applied filters, such as publication date, language, and type of publication to narrow down the search results. Our search strategy yielded a total of 137 published papers.
2.2. Critical Evaluation of the Research
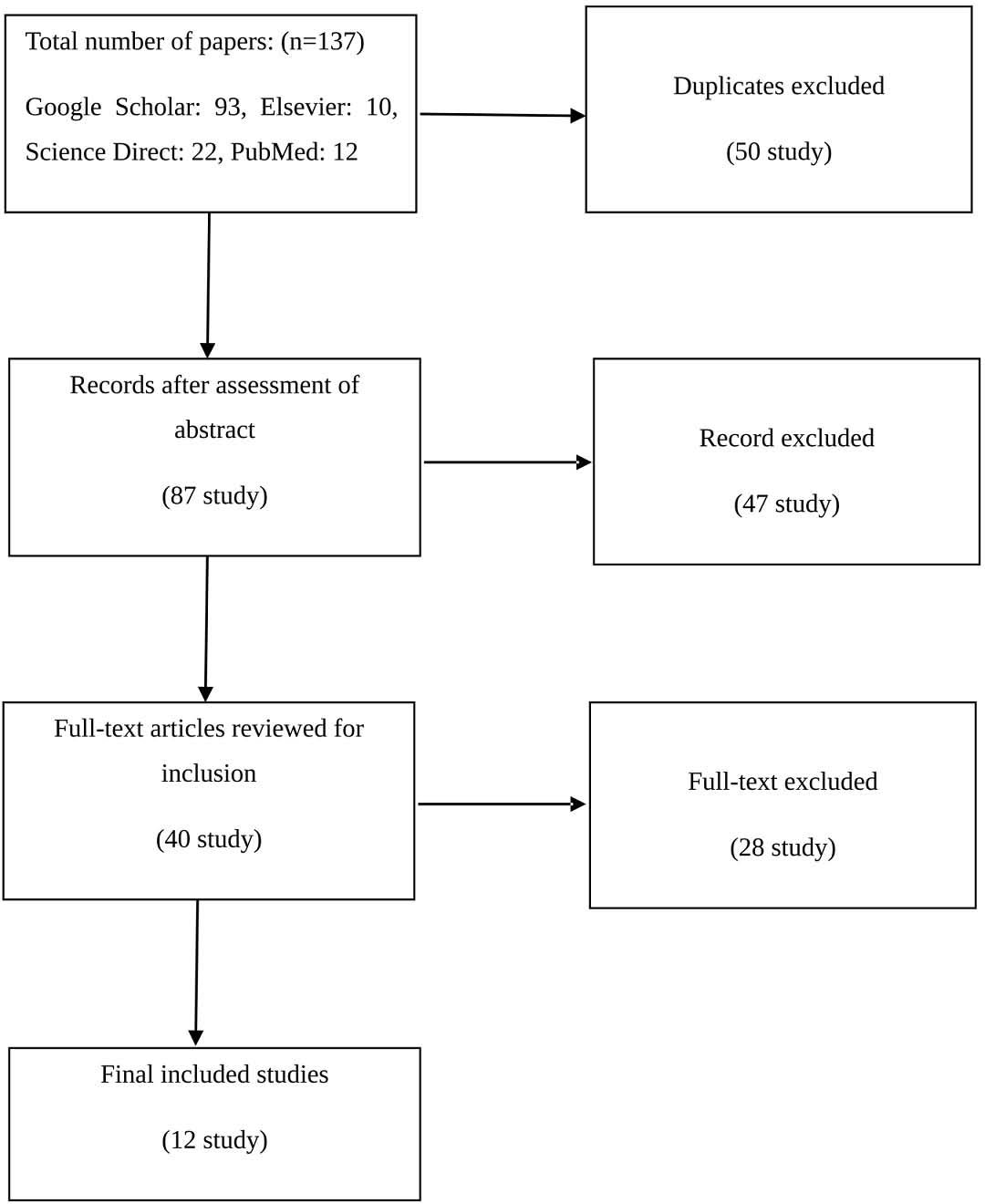
In this step, we screened the retrieved studies for inclusion criteria using a four-step process. First, we excluded 50 duplicates. Second, we screened the abstracts of 87 articles and excluded 47 articles that did not meet our criteria (Table 1). At this stage, we reviewed only the abstracts of the articles without considering the full texts. We identified 47 articles that did not meet the appropriate criteria at this stage of abstract review. For example, some of them focused on the uncertainty of patients or diseases, the degree of uncertainty in nursing students, etc. Third, we screened the full texts of the remaining articles (n=40) and included 12 articles with accessible full texts (Fig. 1). Fourth, we assessed the quality of the included articles using two quality criteria instruments: one for empirical sources and one for theoretical sources.
| References | Author | Year | Study Type |
|---|---|---|---|
| [1] | Cranley et al. | 2009 | Review |
| [2] | Orde | 2016 | Qualitative |
| [3] | Penrod | 2001 | Concept analysis |
| [4] | Cranley | 2009 | Qualitative |
| [7] | Vaismoradi et al. | 2011 | Qualitative |
| [8] | Makridakis et al. | 2019 | Review |
| [10] | Strout et al. | 2018 | Review |
| [11] | Buhr, Dugas | 2002 | Quantitative |
| [12] | Morse, Penrod | 1999 | Qualitative |
| [13] | Carleton, Norton | 2007 | Quantitative |
| [14] | Walker et al. | 2003 | Qualitative |
| [15] | El-Demerdash, Obied | 2017 | Quantitative |
| [16] | Thompson et al. | 2009 | Quantitative |
| [17] | Wurzbach | 1992 | Review |
| [18] | Lee | 2019 | Quantitative |
| [19] | Norton | 2005 | Quantitative |
| [20] | Ying et al. | 2020 | Quantitative |
| [21] | Vadivel et al. | 2022 | Quantitative |
| [22] | Schneider et al. | 2007 | Quantitative |
| [23] | Ghanavati | 2022 | Qualitative |
| [24] | Lipshitz | 1997 | Qualitative |
| [25] | Zahrayi et al. | 2019 | Review |
| [26] | Rowe | 1994 | Concept analysis |
| [27] | Freeston et al. | 1994 | Qualitative |
| [28] | Penrod | 2007 | Concept analysis |
| [29] | Politi | 2007 | Review |
| [30] | Hilton | 1994 | Qualitative |
| [31] | McCormick | 2002 | Concept analysis |
| [32] | Hall | 2002 | Review |
| [33] | Baumann | 1991 | Quantitative |
| [34] | Gerrity et al. | 1990 | Qualitative |
| [35] | Gosselin et al. | 2008 | Quantitative |
| [36] | Gerrity et al. | 1995 | Qualitative |
| [37] | Cioffi | 1998 | Qualitative |
| [38] | Alaszewski, Brown | 2007 | Review |
| [39] | Beresford | 1991 | Review |
| [40] | Engelhardt | 2017 | Qualitative |
| [41] | Franks | 2004 | Qualitative |
| [42] | Ghosh | 2004 | Review |
| [43] | Wakeham | 2015 | Review |
2.3. Analysis and Synthesis
At this stage, we analyzed and synthesized the data from the included articles using five steps: data display, data comparison, data reduction, drawing the conclusion, and verification [9]. We used tables and charts to display the data and compare the similarities and differences among the studies. We reduced the data by grouping them into themes and categories based on our research question. We concluded by summarizing the main findings and implications of the studies. We verified our conclusion by checking its validity and reliability with other sources.
3. RESULTS
Our search strategy yielded a total of 137 published papers. Out of 137 retrieved studies, 50 duplicates were excluded. Then, the abstracts of 87 articles were screened, which resulted in the exclusion of 47 articles (Table 1). Finally, we screened the full texts of the remaining articles (n=40) and included 12 articles with accessible full texts (Fig. 1).
The consensus-based standards for the selection of health measurement instruments (COSMIN) checklist was used to analyze the instruments [44]. In this checklist, out of 12 items, ten items assess the standards for good methodological quality and two items evaluate the general requirements of the articles. Nine of the first ten items examine internal consistency, reliability, measurement error, content validity, structural validity, hypotheses testing, cross-cultural validity, criterion validity, and responsiveness, and one item examines the standards of interpretability. Also, we assessed the general characteristics of the tools (Table 2).
Twelve articles were analyzed with the COSMIN checklist (Table 3). The PRISMA checklist was followed as well.
| References | Tool | Objective | Language | Methodology | Sample | Scope | Items | Response Options |
|---|---|---|---|---|---|---|---|---|
| [11] | Intolerance of Uncertainty Scale | To assess the psychometric properties of an English translation of the IUS to establish its reliability and validity, and further perspective of intolerance of uncertainty | English | Psychometric analysis self-report scales |
N= 341 test: 275 retest: 66 |
Undergraduate courses students | - Uncertainty leads to the inability to act (ten items) - Uncertainty is stressful and uncomfortable (twelve items) - Uncertain occurrences are negative and should be avoided (seven items) - Being uncertain is unjust (five items) |
Five-point Likert scale |
| [13] | Intolerance of Uncertainty Scale | To evaluate intolerance of uncertainty with a short version of the Intolerance of Uncertainty Scale (IUS-12) | English | Psychometric analysis self-report scale |
N= 1057 test: 254 retest: 803 |
Psychology and Kinesiology and Health Studies students | - Factor involves fear and anxiety based on future events (seven-item) - Factor describes uncertainty inhibiting action or experience (five-item) |
Five-point Likert scale |
| [15] | ICU Nurses’ Uncertainty | Assessing the relationship between patient safety culture and uncertainty among intensive care unit nurses |
Arabic | Complete the questionnaires |
N= 155 | ICU nurses | - Situations related to patients (10 items) - Situations related to nurses (18 items) - Situations related to the environment (8 items) - How do nurses feel when uncertain in these types of situations? (8 items) - What strategies do nurses use to address their uncertainty? (10 items) |
Three-point Likert scale |
| [19] | Intolerance of Uncertainty Scale (IUS) | To assess and compare the psychometric properties of the IUS among four racial groups: African American, Caucasian, Hispanic/Latino, and Southeast Asian | English | Psychometric analysis self-report scales |
N= 319 | Students from the University of Houston | - 27 items - A 5-factor solution emerged for African American, Caucasian, and Southeast Asian participants - A 6-factor structure was extracted for Hispanic participants |
Five-point Likert scale |
| [20] | Measuring Uncertainty Intolerance in Surgical Residents Using Standardized Assessments |
Using Physician Reaction to Uncertainty (PRU) and Physician Risk Attitude (PRA) scales to examine for UI in surgical residents |
English | Complete the survey | N= 126 | General surgery residents | - Anxiety because of uncertainty (five items) - Concern regarding bad outcomes (three items) - Reluctance to show uncertainty to patients (five items) - Reluctance to tell mistakes to physicians (two items) - Physician risk attitude (PRA) scale |
6-point Likert scale |
| [21] | Intolerance of Uncertainty Scale-12 (IU-12) | To validate the IU-12 among Iranian undergraduate students | Persian | Cross-sectional design psychometric analysis; complete the questionnaire |
N= 410 | Undergraduate students | IU-12 scale with two factors (prospective anxiety and inhibitory anxiety) |
5-point Likert scale |
| [22] | German version of the Physicians' Reactions to Uncertainty Scales |
To evaluate the validity of a translated and culturally adapted version of the 'Physicians' Reaction to Uncertainty scales' (PRU) | Germany | - Psychometric analysis - Complete the questionnaire |
N= 157 test: 93 retest: 64 |
Primary care physicians | - Anxiety due to uncertainty (five items) - Concern about bad outcomes (three items) - Reluctance to disclose uncertainty to patients (five items) - Reluctance to disclose mistakes to physicians (two items) |
Six-point Likert scale |
| [23] | Uncertainty Measurement Questionnaire (CUMQ) |
To examine the reliability and validity of a Persian questionnaire, which measures different determining physicians' aspects of uncertainty | Persian | Clinical Uncertainty Measurement Questionnaire (CUMQ) has been derived from a mixed-method study | N= 421 | Practicing physicians and clinical residents |
- Uncertainty caused by general determinants (5 items) - Uncertainty caused by individual determinants of the physician (4 items) - Uncertainty caused by dynamics of medical science (11 items) |
Five-point Likert scale |
| [27] | Intolerance of Uncertainty Scale | To examine reactions to ambiguous situations, uncertainty, and future occurrence |
French | Self-report scales | N= 326 test: 216 retest: 110 |
Introductory psychology students | - Uncertainty is unacceptable and should be avoided (9 items) - Uncertainty reflects badly on a person (9 items) - Frustration related to uncertainty (4 items) - Uncertainty causes stress (2 items) - Uncertainty prevents action (3 items) |
Five-point Likert scale |
| [34] | Physicians’ Reactions to Uncertainty (PRU) | Designing a dedicated tool to measure doctors' reaction to uncertainty | English | - Forming a conceptual model - Semi-structured interviews - Review of literature |
N= 700 | Physicians | Stress from Uncertainty subscale (13 items) - Reluctance to Disclose Uncertainty subscale (9 items) |
Six-point Likert scale |
| [35] | Intolerance of Uncertainty Inventory | To design a new instrument to evaluate intolerance of uncertainty, and evaluate its psychometric properties among the French-speaking population |
English | Psychometric analysis self-report scale |
N= 2212 Study 1: 498 Study 2: 703 Study 3: 703 Study 4: 308 |
Students in various disciplines in a university | The scale with 45 items - The first part includes three subscales - The second part includes six subscales |
Five-point Likert scale |
| [36] | Physicians’ Reactions to Uncertainty (PRU) | Revised structural models have greater conceptual clarity | English | - Forming a conceptual model - Responses to 22 items in the original scale and 5 new items |
N= 337 | Physicians | - Anxiety because of uncertainty (5 items) - Concern regarding bad outcomes (3 items) - Reluctance to show uncertainty to patients (5 items) - Reluctance to tell mistakes to physicians (2 items) |
Six-point Likert scale |
| References | Tool | Structural Validity | Internal Consistency | Cross-cultural Adaptation | Reliability | Error and Reliability | Criterion Validity | Hypothesis Testing for Construct Validity | Responsiveness |
|---|---|---|---|---|---|---|---|---|---|
| [11] | Intolerance of Uncertainty Scale | Adequate | Very good | Very good | Very good | Very good | Very good | Very good | Very good |
| [13] | Intolerance of Uncertainty Scale | Very good | Very good | Very good | Very good | Adequate | Very good | Very good | Very good |
| [15] | ICU Nurses’ Uncertainty | - | Doubtful | Adequate | Doubtful | Doubtful | Not mentioned | Unmentioned | Unmentioned |
| [19] | Intolerance of Uncertainty Scale (IUS) | Adequate | Very good | Adequate | Doubtful | Doubtful | Very good | Unmentioned | Unmentioned |
| [20] | Measuring Uncertainty Intolerance in Surgical Residents Using Standardized Assessments |
Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Unmentioned | Unmentioned |
| [21] | Intolerance of Uncertainty Scale-12 (IU-12) | Very good | Very good | Very good | Doubtful | Adequate | Inadequate | Very good | Very good |
| [22] | German version of the Physicians' Reactions to Uncertainty scales |
Adequate | Very good | Inadequate | Very good | Adequate | Very good | Unmentioned | Unmentioned |
| [23] | Uncertainty Measurement Questionnaire (CUMQ) |
Very good | Very good | Not mentioned | Very good | Very good | Very good | Very good | Very good |
| [27] | Intolerance of Uncertainty Scale | Adequate | Very good | Not mentioned | Very good | Adequate | Very good | Very good | Very good |
| [34] | Physicians’ Reactions to Uncertainty (PRU) | Adequate | Very good | Very good | Very good | Adequate | Very good | Very good | Very good |
| [35] | Intolerance of Uncertainty Inventory | Adequate | Very good | Adequate | Very good | Very good | Very good | Very good | Very good |
| [36] | Physicians’ Reactions to Uncertainty (PRU) | Very good | Very good | Very good | Very good | Very good | Very good | Very good | Very good |
Original and review articles with the following criteria were included in this study: a) providing at least one definition for uncertainty in nursing practice; b) explaining the development of an instrument for measuring uncertainty; c) describing the use of an instrument to measure uncertainty in the clinical decision-making of nurses or other medical professionals; and d) being conducted on people over the age of 18 with the full-text available in English or Persian languages.
We excluded all interventional and general studies that were not related to nursing. Furthermore, studies were excluded if they focused on uncertainty among patients, the experiences of nurses and nursing students, or the correlation between uncertainty and other concepts. A datasheet was prepared before data collection and the research team (JF, RF, ZV, and GHA) agreed on its items and structure. The extracted data included authors’ names, year of publication, objective(s), basic concepts, methodology (i.e., study design, data collection instrument, and data analysis), and the validity and reliability of the tools used in the study.
4. DISCUSSION
Uncertainty seems inevitable [43]. In most reviewed studies, the most essential characteristics of uncertainty were ambiguity [4, 30], lack of confidence and control [28], complexity [4, 26, 29], being on the horns of a dilemma [12], unpredictability, and unexpectedness [4]. Other characteristics were probability and uncertain outcomes [31]. In addition, the nurses' lack of knowledge played a vital role in uncertainty [4, 24, 31].
Morse and Penrod (1999; 2001) defined uncertainty as a dynamic state between enduring and suffering [12]. Uncertainty has cognitive [4, 31] and emotional [4, 30, 38] dimensions, is accompanied by emotional feelings [14], and is time-dependent [31]. According to Hilton (1994), this situation is accompanied by such feelings as stress and wondering [30]. However, it may sometimes be accompanied by positive feelings, such as hope and motivation for seeking information, mainly when uncertainty is at a moderate level [17]. On the other hand, uncertainty ranges from surety to vagueness [30].
Concerning the measurement tools, the majority of the instruments measured the degree of uncertainty tolerance [27, 42]. We found only one instrument for measuring uncertainty in nurses [15]. Uncertainty measuring instruments can be categorized into general and specific instruments.
4.1. Synthesis of Results
Despite the increasing number of studies on physicians’ clinical uncertainty, limited studies are available on nurses’ clinical uncertainty [3]. The IUS has been used in some Iranian and international studies on nurses [10, 18]. Zahrayi et al. performed a review study in Iran to determine the psychometric properties of the IUS. In this study, the intolerance of uncertainty was defined as an intrinsic feature caused by negative beliefs about uncertainty and its consequences, such as worry and the need for confidence and control. The authors emphasized that intolerance of uncertainty is an essential predictor of OCD, worry, anxiety, and eating disorders [25]. Nonetheless, no specific instrument is available for measuring uncertainty in nurses’ clinical decision-making.
A precise definition of uncertainty is necessary for designing an uncertainty measurement instrument. According to the literature, ambiguity [4, 30], lack of confidence and control [28], complexity [26, 29], and being on the horns of a dilemma [12] are the most critical characteristics of uncertainty. However, the unanswered question is whether these characteristics adequately measure nurses' uncertainty in clinical decision-making. A review study on nurses' uncertainty in decision-making reported that although nurses may face uncertainty in many situations, the probability of uncertainty increases when there is a need for interpretation or intervention in case of emergencies. The authors also emphasized that detecting and controlling an uncertain situation are essential skills for nurses to make effective clinical decisions [1]. Furthermore, this review concluded that an uncertain situation could result in cognitive, emotional, and behavioral reactions. However, nurses often use problem-solving skills to better understand the situation when facing uncertain situations. In addition to using their knowledge and experience, nurses also consult with experienced colleagues to deal with uncertain situations. Nevertheless, most studies on uncertainty have been conducted on physicians or patients, and there are few relevant studies on nurses. Therefore, further studies are needed to fill this gap [1].
In the process of patient care, clinical decision-making is the outcome of critical thinking, clinical reasoning, and clinical judgment [45]. Appropriate instruments are needed to assess and detect nurses' uncertainty, especially in the stage of clinical judgment. However, no specific instrument is available in this regard, and the existing instruments are general and do not measure all dimensions of uncertainty in nursing. Therefore, they are inappropriate for assessing uncertainty in clinical nursing practice [3].
The existing instruments measure situations that cause uncertainty, people’s feelings in dealing with uncertainty, and adaptive responses in an uncertain situation [15]. Cranley investigated the strategies used by ICU nurses in dealing with uncertainty. The study reported that coping with uncertainty includes three stages, namely, identifying uncertainty and its emotional and physiological responses (e.g., stress), management of the situation (e.g., receiving help from colleagues), and outcomes (e.g., learning and gaining experience from new situations). Cranley concluded that nurses use cognitive-behavioral, emotional, and behavioral strategies to adapt to an uncertain situation [4]. Given the acceptable reliability of the specific ICU nurses’ uncertainty measurement tool [15], this tool can be adapted and used to measure the nurses' responses to uncertainty. However, it is essential to design culture-specific instruments for measuring nurses' uncertainty in clinical decision-making. Furthermore, if researchers intend to consider the weight of clinical judgment in the degree of uncertainty of nurses when making clinical decisions, specific tools should be designed for this purpose. In this respect, qualitative methods, such as content analysis for finding the meanings of concepts and processes and reducing the challenges of facing contradictory theories, would be suitable [46]. Qualitative methods allow researchers to interpret the originality and truth of data objectively and scientifically. They also allow to reveal the hidden themes and patterns [47]. Investigating nurses’ lived experiences of uncertainty in clinical decision-making helps researchers discover the characteristics of uncertainty in clinical decision-making and design an instrument based on the discovered characteristics.
4.2. Uncertainty Attributes
Given that a person constantly understands and processes evidence at any given time, the state of uncertainty is dynamic [28]. 'Dynamic' refers to the interaction between antecedents over time [3]. Uncertainty is also a discomforting situation [28, 41] because it disrupts a person's daily life [28].
The experience of uncertainty is pervasive in human experience and is influenced by a sense of self-confidence and control; it can be very specific (event-focused) or more general, as well as non-normative and detrimental to human development [28]. The three attributes of uncertainty include probability, temporality, and perception, which may be explicit or implicit in uncertainty. All the attributes of uncertainty overlap, and they all affect each other [31]. Feelings of confidence and a sense of control are the main factors that determine the nature of the experience of uncertainty [28].
4.3. Uncertainty in Decision-making
In the health system, uncertainty in decision-making can include diagnostic, prognostic, treatment, interventional [16], technical, personal, and conceptual aspects [32, 39]. Regarding the uncertainty in intervention decisions, we can mention the uncertainty of nurses whether to request emergency care for their patients [37], and nurses' uncertainty is rooted in their uncertainty about their interpretation and choice of interventions [1]. In this regard, it has been observed that nurses may face uncertainty in decision-making during all clinical decision-making stages (review, use of intuition and intervention, etc.). However, it seems that most cases occur during the interpretation of findings [1]. Nurses make better decisions with structured information (e.g., diagnostic procedures) than with unstructured details [48]. Prognostic uncertainty can be due to the unpredictability of future events or the limited accuracy of probability estimation [40]. The source of technical uncertainty can be related to the information of the doctor or nurse and can also be associated with the rapid growth of health system knowledge. Individual uncertainty arises from the relationship between the patient and the physician or nurse. Conceptual uncertainty means not being aware of the patient's competitive needs for shared resources [32, 39].
According to the classification for nurses' uncertainty, micro-uncertainty refers to a person's degree of confidence in their decisions. Due to the different decisions of different people, macro-uncertainty is observed in the decisions made by individuals [33].
Nurses care for patients with different personal characteristics who respond differently to nursing interventions, and this can cause uncertainty in them. On this account, nurses face a significant challenge when using judgment and decision-making skills; whatever decision they make, they must use the available evidence to think about the uncertain future. Despite their uncertainty, they must decide what to do [16]. A correct understanding of nurses' uncertainty can lead to strategies that support nurses in their clinical decisions [1]. Therefore, it seems necessary to conduct specific studies on the concept of uncertainty in decision-making in nursing.
4.4. General Instruments
The Intolerance of Uncertainty Scale (IUS), developed by Freeston et al., is a self-report instrument designed to understand why people worry. In our review, all the participants in the included studies were undergraduate psychology students with an average age of 22 years [27].
Validity: The methodological quality of content validity and hypothesis testing was “very good”. The IUS showed acceptable convergent and divergent validity when used concurrently with the Worry Domain Questionnaire (WDQ) (r = 0.57) [49], Beck’s Anxiety Inventory (BAI) (r = 0.57) [50], Beck’s Depression Inventory (BDI) (r = 0.52) [51], Questionnaire on Generalized Anxiety Disorder-Modified (QGAD-M) [52], and Penn State Worry Questionnaire (PSWQ) (r = 0.63) [53]. Both construct validity and criterion validity were identified as “very good”. Moreover, the measure of sampling adequacy for the intercorrelation matrix was 0.80, indicating that factor analysis was appropriate.
Reliability: The IUS also showed acceptable reliability with an internal consistency of 0.91. Based on the IUS and the Worry Scale responses, people can be categorized into three groups: those who meet somatic criteria, those who meet both somatic and cognitive criteria, and those who meet neither cognitive nor somatic criteria [27].
The English version of the IUS, developed by Buhr et al., has four subscales. This scale reflects the idea that uncertainty is stressful and upsetting, uncertain situations are negative and should be avoided, being uncertain is unfair, and uncertainty results in failure to act [11]. The English version was tested and validated in a sample of students just admitted to various undergraduate programs.
Validity: This scale has four factors, and its scores have an acceptable correlation with the scores of PSWQ [53], Worry and Anxiety Questionnaire (WAQ) [54], BDI-II [55], and BAI [50]. The correlation coefficients showed that the English version of IUS is more correlated with worry criteria (r = 0.60) and less with anxiety and depression criteria, confirming its convergent and divergent validity.
Reliability: The English version of the IUS had acceptable internal consistency (Cronbach’s alpha = 0.94) and test-retest reliability (r = 0.74). This scale can differentiate between people who meet the criteria for generalized anxiety disorder (GAD), people who meet only the somatic criteria, and those who meet none of the GAD criteria. It has been shown that while people who meet the criteria for GAD have the highest scores in the English version of IUS, those who meet none of the criteria for GAD have the lowest scores [11].
Norton assessed the psychometric properties of IUS to ascertain if the structure of the instrument differs among four racial (cultural) non-clinical African-American, Caucasian, Spanish/Latin, and Southeast Asian groups. The participants were bachelor’s students of Houston University, and their mean age was 21.65 ±4.93 (MD) years [19].
Validity: The factor structure of each non-clinical group indicated a poor and unstable representation. The factor analysis has shown the five- or six-factor solutions. The IUS had a high correlation with the PSWQ and GADQ-IV [19].
Reliability: The overall internal consistency of the IUS was good (α=0.945). Moreover, the alpha coefficients of the African (α =0.951), Caucasian (α =0.942), Spanish (α =0.934), and Southeast Asian (α =0.954) participants were similar [19].
Carleton et al. developed a short version of IUS, known as IUS-12 [13]. They reduced the 27 items of the original IUS [27] to 12 items and tested the new scale on two academic groups. This version of IUS-12 has two subscales, including prospective anxiety and inhibitory anxiety.
Validity: The IUS-12 showed acceptable convergent validity when it was administered concurrently with BDI-II (r = 0.56) [55], BAI (r = 0.57) [50], PSWQ (r = 0.54) [53], and GADQ-IV (r = 0.61) [56].
Reliability: A significant association was observed between the scores obtained from IUS-27 and IUS-12 (r = 0.96), indicating the closeness of the results of these two scales; this confirms the validity of IUS-12. Furthermore, IUS-12 had a high internal consistency (α = 0.91), which was considered “acceptable”, and the highest inter-item correlations were low to moderate (between 0.27 and 0.65) [13].
Gosselin et al. (2008) also developed a self-report Intolerance of Uncertainty Inventory (IUI) to measure uncertainty intolerance. The initial instrument had 72 items, which were reduced to 45 items via factor analysis. The IUI has two parts. The first part includes three subscales: intolerance of uncertainty and uncertain situation, intolerance of unexpectedness, and difficulty waiting in an uncertain situation. The second part consists of six subscales: overestimation of the probability of an adverse event, control, reassurance-seeking, avoidance, worry, and doubt [35].
Validity: The content validity analysis was conducted by researchers and two experienced individuals. Fifteen university students also confirmed its comprehensibility. The convergent validity of the IUI was also confirmed through concurrent administration with the IUS [27], PSWQ [53], WAQ [54], and Padua Inventory [57].
Reliability: The instrument's stability and internal consistency were assessed and confirmed through test-retest (a five-week interval) and Cronbach's alpha coefficient. All scores of the IUI were correlated with the IUS (developed by Freeston) and had a moderate and high correlation with the scores resulting from the validated measures of GAD and obsessive-compulsive disorder (OCD). Besides, individuals who met the GAD criteria on the WAQ questionnaire scored higher on the IUI. Overall, study results supported the temporal stability of the IUI after a 5-week interval.
Vadivel et al. conducted a study on Iranian students to assess the psychometric properties of the Persian version of the IU-12; the age range was 18-24 in this study [21].
Validity: The values of the content validity index (CVI) and the content validity ratio (CVR) were over 0.7 and 0.78, respectively. In this study, the results of previous studies on the PSWQ and the Depression Anxiety Stress Scale (DASS-21) were assessed along with the Persian version to check the validity. Two subscales of the translated IUS-12 had direct relationships with worry (r=0.75), stress (r=0.61), anxiety (r=0.61), and depression (r=54) [21].
Reliability: The values of CR and Cronbach’s alpha were 0.86 and 0.89, respectively, and the internal consistency was good [21].
4.5. Specific Instruments in other Medical Professions
4.5.1. Physicians’ Reactions to Uncertainty (PRU)
Gerrity et al. designed a specific instrument to measure physicians' reactions to uncertainty. To this end, first, a conceptual model was developed to evaluate the effect of physicians' reactions to uncertainty on their decisions. This instrument consisted of 22 items in two subscales of reluctance to disclose uncertainty and stress from uncertainty.
Validity: Budner's Intolerance scale [58] did not correlate with the Stress from the Uncertainty scale (r = 0.08), but it had a high correlation with the Reluctance to Disclose Uncertainty subscale (r = 0.28; P < 0.0008).
Reliability: Cronbach's alpha values for the stress and disclosure subscales were 0.90 and 0.75, respectively [34].
This instrument was designed by Gerrity to measure physicians' reaction to uncertainty in the patient care process and their adaptive behaviors. This scale measures the emotional reactions of physicians to uncertainty during patient care and includes physicians' emotional reactions to concerns and physicians' behaviors to cope with emotions and concerns. The authors claimed that the revised structural model had greater conceptual clarity and better fit to the data compared to the original PRU model.
Validity: In hypothesis testing, it was found that uncertainty-induced anxiety and worry about bad outcomes were not fully correlated and represented distinct constructs.
Reliability: The stress subscales from uncertainty and anxiety about negative results had an acceptable correlation (r = 0.79). The Cronbach's alpha values of the subscales ranged from 0.72 to 0.86, indicating good internal consistency of the scale [36].
In a study assessing the surgical residents’ intolerance, PRU and Physician Risk Attitude (PRA) were used to analyze the residents’ intolerance. Statistical tests, mean, and standard deviation were also used. The scores of PRU and PRA were analyzed based on personality factors. The relationship between these instruments was analyzed; however, the validity and reliability of the instrument were not discussed. The questionnaires were given to the surgery residents only once [20].
Schneider conducted a study to analyze the psychometric properties for validation and cultural adaptation of the German version of the PRU among physicians [22].
Validity: To achieve the highest content validity, the German version of the PRU was translated and back-translated based on the cultural adaptation instructions. The draft of the translation was given to 15 general practitioners as a pilot study.
Reliability: The internal consistency of the instrument was evaluated using a retest (2-week interval) and Cronbach’s alpha.
4.5.2. Clinical Uncertainty Measurement Questionnaire (CUMQ)
Ghanavati conducted a qualitative study aiming to assess the reliability and validity of the Farsi questionnaire designed to measure different aspects determining intolerance from clinical physicians’ perspectives in Iran. This instrument consisted of 24 items, including the uncertainty resulting from general determining factors, the uncertainty resulting from physicians’ individual determining factors, the uncertainty resulting from patients’ individual determining factors, and the uncertainty resulting from the dynamics of medicine [23].
Validity: In the content analysis, the values of CVR and CVR ranged from 0.8 to 1. Convergent validity was also checked. The Fornell and Larcker criteria and cross-loading were analyzed to check the discriminant validity [23].
Reliability: The composite reliability and Cronbach’s alpha were higher than 0.7 in all dimensions [23].
4.5.3. Specific Tools for Nurses: ICU Nurses’ Uncertainty Questionnaire (INUQ)
The ICU Nurses’ Uncertainty Questionnaire (INUQ), developed by El-Demerdash et al., measures situations that cause uncertainty and adaptive reactions to deal with uncertainty among nurses [15].
Reliability: The reliability of this instrument was assessed using Cronbach’s alpha (0.88). Given the instrument's responsiveness, El-Demerdash reported a high correlation between the patients' safety culture and experience of uncertainty in ICU nurses [15].
The main limitation of our study was the inaccessibility of the full texts of several articles. We excluded all interventional and general studies that were not related to nursing. Furthermore, studies were excluded if they focused on uncertainty among patients, the experiences of nurses and nursing students, or the correlation between uncertainty and other concepts. It is recommended that more studies be conducted in this area.
5. IMPLICATIONS FOR NURSING
A suitable tool can be helpful in measuring nurses' awareness about their degree of uncertainty in decision-making and nursing managers' awareness about nurses' uncertainty, thereby helping in planning to reduce the complications caused by nurses' uncertainty in clinical decision-making.
CONCLUSION
Most studies have focused on the attributes of uncertainty in general or uncertainty in nurses' practice in a specific department, such as the ICU. Therefore, qualitative studies are necessary to extract the attributes of uncertainty in nurses' clinical decision-making. On the other hand, the available tools measure concepts and are not specifically dedicated to measuring uncertainty in nurses' clinical decision-making. Therefore, it is essential to develop suitable tools. Given the importance of providing quality and desirable care to patients, understanding how nurses experience uncertainty at different decision-making stages can help promote appropriate interventions, provide quality care to the patients, and reduce the complications caused by nurses' uncertainty in clinical decision-making.
LIST OF ABBREVIATIONS
| SID | = Scientific Information Database |
| COSMIN | = Consensus-based Standards for the Selection of Health Measurement Instruments |
| CUMQ | = Clinical Uncertainty Measurement Questionnaire |
| PRU | = Physicians’ Reactions to Uncertainty |
ETHICAL STATEMENT
Tabriz University of Medical Sciences (Ethics code: IR.TBZMED.REC.1399.148.). This article was derived from a thesis research project.
AVAILABILITY OF DATA AND MATERIAL
The data that support the findings of this study are available on request from the corresponding author [F. R].
FUNDING
This research was funded by the research deputy of Tabriz University of Medical Sciences (Ethics code: IR.TBZMED.REC.1399.148 and code of Phd thesis project: 64730).
ACKNOWLEDGEMENTS
Our sincere appreciation goes to the Research Deputy of Tabriz University of Medical Sciences for their financial support.
Supplementary material is available on the publisher’s website along with the published article.


