SYSTEMATIC REVIEW
The Effectiveness of Telenursing for Diabetes Self-management Education: A Scoping Review
Theresia Titin Marlina1, 2, Haryani Haryani1, 3, *, Widyawati Widyawati4, Dita Hanna Febriani2
Article Information
Identifiers and Pagination:
Year: 2023Volume: 17
E-location ID: e187443462307190
Publisher ID: e187443462307190
DOI: 10.2174/18744346-v17-230815-2023-38
Article History:
Received Date: 29/3/2023Revision Received Date: 22/05/2023
Acceptance Date: 31/05/2023
Electronic publication date: 29/08/2023
Collection year: 2023

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Diabetes mellitus (DM) is a chronic disease whose complications can cause a decline in quality of life and which requires long-term care. Diabetes Self Management Education (DSME) effectively helps control glycemic events and prevent DM complications. Telenursing has become a promising approach to educating patients with DM.
Objective:
This scoping review aimed to summarize the effectiveness of telenursing for DSME.
Methods:
The scoping review methodology guided by Arksey and O’Malley and Levac et al., and PRISMA-ScR guidelines were used. Comprehensive searches based on the concept of self-management education and technological media for education were conducted using databases, such as Cochrane, Science Direct, EBSCO, PubMed, and Portal Garuda. Articles were screened from 2013 to 2023, which were RCTs written in English or Bahasa Indonesia, including the adult population with T2DM, and whose one of the research outcomes has been diabetes self-management. Data were then extracted, synthesized, and concluded.
Results:
A total of 48,997 articles were screened at the title and abstract levels. We obtained 48,953 articles after removing the duplicates and finally acquired 1,327 articles appropriate to the criteria for full-text. We identified 12 articles and found telenursing for education by telephone or combined with other technological media, such as videos, to effectively improve diabetes self-management behavior in patients with T2DM.
Conclusion:
Telephone calls are one of the potential methods of telenursing for diabetes self-management education. Nurses can use telenursing as an effective and efficient educational media to improve glycemic control in patients with T2DM.
1. INTRODUCTION
Diabetes mellitus (DM) is a chronic metabolic disease that requires long-term treatment. The prevalence of DM is estimated to increase as the global population ages to 578 million in 2030 and 700 million in 2045. The World Health Organization (WHO) predicts that there will be an increase in people with T2DM in Indonesia from 8.4 million in 2000 to 21.3 million in 2030 [1]. The 2018 Basic Health Research (Riskesdas) reported the prevalence of DM in Indonesia to be 10.9% [1]. The data and information center of the Ministry of Health in the Republic of Indonesia reported that 6.2% (10.8 million) people suffered from DM in 2020. Indonesia is ranked 7th in the world, with 10.7 million people suffering from DM and ranks 3rd in Southeast Asia with a prevalence of 11.3% [2], rendering DM the third-largest cause of death in Indonesia (6.7%) [3]. DM is a chronic disease with an increasing prevalence, whose complications can lead to a decrease in the quality of life of patients [4, 5], require long-term care, have high treatment costs [6, 7], and affect psychological conditions [8]. Proper diabetes self-management can reduce these impacts.
Nurses play a role in providing health education to patients by utilizing technology, as it is an essential factor in improving current health services. The government policies for providing health services through information and communication technology in the pandemic era are crucial. This policy is the basis for implementing general health services and nursing services. In addition, high internet network users are also one aspect of the successful use of technology for health services. Based on the latest report of “We Are Social,” there is an increase of 17% or 25 million internet users in this country compared to the previous year. In 2020, there were 175.4 million internet users estimated in Indonesia. The results of a review reported that 35 studies (94.6%) used telenursing for patient care (educational strategies, monitoring systems, and care management), and two studies (5.4%) used educational methods [9].
Nurses can use telenursing as a medium of health education for patients. Education on diabetes self-management has increased knowledge, changed healthy living behavior, improved metabolic control [10-15], and significantly increased self-efficacy [16]. Health education with telenursing is a promising approach to increasing diabetes self-management. Several benefits of telenursing are effectiveness and efficiency, ease of information, high-quality care, fewer trips, no waiting queues, convenience, and simplicity [17, 18]. Furthermore, telenursing has many benefits that are effective in the current COVID-19 pandemic situation to controlling the spread of disease [19], improving health management [20], ensuring continuity of care, increasing patient and family participation in care, and saving time and money [21].
Several studies on diabetes self-management using technology, such as telenursing, have reported that it can improve the self-management behavior of patients with T2DM [18, 22-24]. A study has shown that telehealth significantly increased self-care scores among patients with T2DM [22]. The self-management education using booklets and telephones has also increased diabetes self-efficacy and self-management behavior in patients with T2DM [23]. In addition, using telephones could increase self-care scores for patients with T2DM [24].
The novelty of this review is that it describes changes in the self-care of patients with T2DM after being given health education by nurses. The focus of nursing services is the patient's behavior in response to their illness. Nurses must understand any changes in behavior during the patients’ illness. The authors of this review have focused on behavioral changes in diabetes self-management. Diabetic patients who have good diabetes self-management have been reported to achieve glycemic control. Many previous reviews have reported effects on clinical outcomes, such as HbA1C levels, cholesterol, blood sugar levels, and low-density lipoproteins [25-33]. These clinical outcomes have been reported to result from behavior change and the doctor's discretion; however, nursing care aims to change healthy living behavior.
There have been nine reviews found on the same topic in the last two years, with the latest review reported in 2021. The differences in the previous reviews have been observed in terms of population [25, 27-30], year of publication [25, 27-34], database [25, 27-34], and outcome [25, 27-33]. Similar publications have been found in the PubMed and Cochrane databases [25, 27-29, 33], as well as PubMed and Science Direct databases [30-32, 34].
The results of this review are helpful for nurses in providing nursing services to patients with T2DM by utilizing communication technology. The review, thus, summarizes the effectiveness of using telenursing for diabetes self-management education.
2. MATERIALS AND METHODS
2.1. Study Design
This scoping review followed the procedure of Arksey and O’Malley [35], and Levac [36]. The five steps of this procedure are as follows: 1) identify clear research objectives and search strategies, 2) identify suitable research papers, 3) select research papers, 4) extract and map data, and 5) summarize, analyze, and present the results in a report (Fig. 1).
2.2. Literature Search Strategy
The literature search was conducted extensively by searching several databases. An independent search has been conducted in EBSCO, Cochrane, Science Direct, PubMed, and the Portal Garuda databases for literature published from 2013 to 2021, including RCTs, articles in English or Indonesian involving the adult population with type 2 diabetes mellitus, and with one of the research outcomes as diabetes self-management.
The first step in determining keywords is to look for equivalent words with MeSH. The equivalent terms for telenursing are telehealth and digital health; NIDDM is used as an alternative term for type 2 diabetes mellitus, and self-care is used as an equivalent term for self-management. The researchers, therefore, searched the keywords “telenursing” OR telehealth OR digital health OR online OR telemedicine AND type 2 diabetes mellitus OR NIDDM, AND “self-management” OR self-care.
2.3. Identification and Selection of Relevant Articles
The study selection process followed the Preferred Reporting Items for Systematic Review and Meta-Analyses extension for scoping reviews [36]. The authors compared the results of five searches independently and removed duplicated articles. The Mendeley reference manager was used to list articles during the selection process. We selected twelve studies for review after passing them through a screening and eligibility process (Fig. 1). The articles were determined eligible for inclusion if they discussed all communication technology tools or media in English and Indonesian. All articles were RCTs and published between 2013 to 2023. All articles included diabetes self-management outcomes and adult patients with T2DM as subjects. The protocols, reviews, dissertations, and conferences were excluded.
2.4. Data Extraction
The data were extracted using a spreadsheet of Microsoft Excel and presented as a table. The table included the name of the author and year of publication, research objectives, methods, and respondents (Table 1). Telenursing description included the name of the author, technology media, measurement and intervention, outcomes, and results (Table 2).
3. RESULTS
A total of 48,997 articles were identified. After removing the duplicates, we obtained 48,953 articles. We screened 48,953 articles with reference to their titles, abstracts, English language, adult ages, and the years of publication from 2013 to 2023. We selected 1,327 articles appropriate to the criteria for full-text and excluded the articles involving patients with type 1 diabetes mellitus, non-telenursing or telehealth intervention, no self-management outcomes, protocol study, systematic review, editorial, thesis, and conference. Finally, we selected 12 articles for this scoping review (Fig. 1).
3.1. Study Characteristics
There were three articles with less than 100 respondents [37-39] and nine with more than 100 respondents [22, 23, 40-46]. In the reviewed articles, the mean age ranged from 51.8 ± 10.7 to 62.9 ± 10.3 years, and the mean duration of diabetes diagnosis was from 8.09 ± 6.95 to 11.33 ± 5.66 years (Table 1).
Seven studies used the Summary of Diabetes Self-Care Activities questionnaire (SDSCA) [38, 39, 41-45], and two studies used the Diabetes Self-Management Questionaire (DSMQ) [23, 37]. One study used the American Association of Diabetes Educators 7 Self-Care Behaviors (AADE7) [46], one study used the Diabetes Self-care Questionnaire (DSQ) (22), and the Self Care Inventory (SCI) instrument [40]. The researcher used the SDSCA instrument to measure diabetes self-management, consisting of diet, physical activity, medication, blood sugar monitoring, foot care, and smoking [38, 39, 41-45, 47].
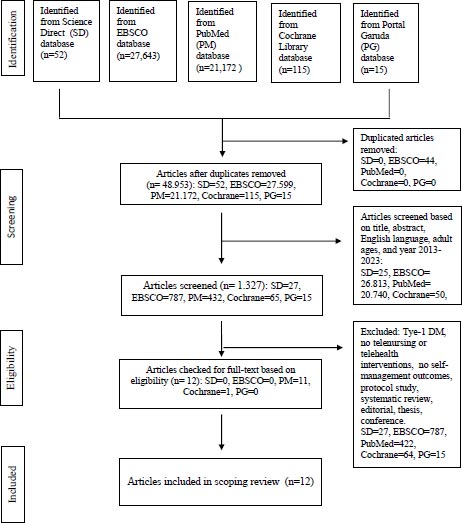 |
Fig. (1). Prisma flowchart for scoping review [36]. |
3.2. Telenursing Description
3.2.1. Theme 1: Mode of Telenursing
In the reviewed articles, information technology communication media as a mode of telenursing used for DSME was a single or combination of communication technology. Five articles comprised communication by telephone only [23, 37, 44-47]. One article used a combination of telephone or text messages, short video clips, and automatic health reminders [39], while others employed a combination of telephone and short message service [40], diabetes self-care software [43], a combination of telephone and voice mail message [41], a combination of telephone and movie clips [22], a combination of telephone, lectures, group discussion, film presentation, and booklet [37], and a combination of application and course [41] (Table 2).
3.2.2. Theme 2: The Duration of Telenursing Intervention
The duration of telenursing intervention was different for each article. In four articles, telenursing was used for 3 months [37, 38, 40, 44], for 6 months in four articles [22, 23, 39, 42], and for 12 months in four articles [41, 43, 45, 46]. The time measurement outcomes varied from one study to another. All articles measured the outcome at baseline, ten articles in a range of 3-6 months from baseline [22, 23, 37-41, 44, 45, 48], and four articles at 6-12 months after baseline [41, 43, 45, 46] (Table 2).
3.2.3. Theme 3: Effectiveness of Telenursing
Most studies reported phone usage as the most effective for telenursing [22, 23, 37-39, 41, 44-46, 48]. The telephone call alone may effectively improve diabetes self-management behavior if it is conducted frequently, once a month for six months or twice a month for three months, followed by once a month for nine months [46]. Two studies reported in detail the significance of each self-management domain, self-management behavior of carbohydrate spacing (p=0.04), glucose monitoring (p=0.001), foot care (p=0.02) [39], glucose management (p<0.001), dietary control (p=0.015), and physical activity (p<0.001) [49]. Meanwhile, other studies did not report the significance of each self-management domain [22, 23, 38, 40, 42-45] (Tables 3 and 4). There were five articles found with a p-value from 0,001 to 0,035 [22, 23, 37-39], two articles with an effect size of 0,61 and 0,606 [22, 40], and two articles did not report a p-value [41, 43] (Table 2).
Another study modified telephone calls with other methods to conduct diabetes self-management behavior effectively. These methods included training, daily health sessions with short video clips, automatic health session reminders, telephone calls for six months [39], telephone calls and group discussions, booklets, and movies for three months [22]. The combination of telephone with training, daily health sessions with short video clips, and automatic health session reminders
| Author(s) | Objectives | Methods | Respondents |
|---|---|---|---|
| Greenwood et al., 2015 | To determine the effectiveness of monitoring intervention with telehealth on fasting blood sugar in 2 DM adults without insulin. | RCT | Intervention group: 45, Control group: 45. Mean age: 58 ± 11 years, with a mean duration of diabetes 8,2 ± 5,4 years. |
| Azami et al., 2018 | The evaluation of the effect of diabetes self-management education by nurses on HbA1c. | RCT | Intervention group: 71, Control group: 71. Mean age: 54,2 ± 11,8 years, with mean duration of diabetes 8,9 ± 7,4 years. |
| Forjuoh et al., 2014 | The effectiveness of two different diabetes self-care interventions on glycemic control. | RCT | Intervention group 1 (CDSMP): 101; Intervention group 2 (PDA): 81 Intervention group 3 (combination CDSMP and PDA): 99; Control group: 95 Mean age: 57,6 ± 10,9 years, with the mean duration of diabetes being not clear. |
| Kim and Utz, 2019 | To evaluate the effects of a social media-based “health literacy sensitive” diabetes management intervention on self-care behaviors and glucose control compared with telephone-based diabetes management interventions and regular care, and identify how health literacy affects the effectiveness of diabetes management interventions. | RCT | Intervenstion group 1 (SM-HL): 51; Intervension group 2 (TEL-HL): 52; Control group: 52 Age, median (IQR): Intervention group 1 = 46,00 (15,50) years Intervention group 2 = 52,00 (17,00) years Control group = 56,00 (10,00) years Duration of diabetes, median (IQR): Intervention group 1 = 27,5 (85,80) years Intervention group 2 = 24 (113,00) years Control group = 11,5 (33,00) years |
| Maslakpak et al., 2017 | To study and compare the effectiveness of family-oriented education delivered through two face-to-face methods and telephone-based methods on self-care behavior. | RCT | Face-to-face family-oriented education group: 30; Telephone-based family-oriented education group: 30; Control group: 30. Mean age: Intervention group 1 = 49,9 ± 4,98 years Intervention group 2 = 49,46 ± 4,76 years Control group = 50,6 ± 3,74 years Mean duration of diabetes: Intervention group 1 = 10,33 ± 6,89 years Intervention group 2 = 9,26 ± 5,47 years Control group = 11,33 ± 5,66 years |
| Chan et al., 2014 | To investigate whether frequent contact via telephone program-based peer support (Peer Support, Empowerment, and Information Technology Connected Remote Communication [PEARL]) would increase cardiometabolic risk and health outcomes by improving psychological well-being and self-care in patients receiving care. An integrated program was implemented with a web-based multi-component quality improvement program (JADE [Joint Asia Diabetes Evaluation]) | RCT | The JADE and PEARL group: 312, JADE group: 316. Mean age: 54.7 ± 9.3 years, with mean duration of diabetes 9,4 ± 7,7 years. |
| Sherifali et al., 2019 | To describe the effect of diabetes health coaching on clinical outcomes and self-care behaviors in community-based adults living with T2DM. | RCT | Intervention group: 182. Control group: 182.. Mean age: 57,9 ± 11,79 years, with mean duration of diabetes 8,69 ± 8,54 years. |
| Peimani et al., 2016 | To assess the effectiveness of mobile SMS intervention on the education of basic self-care skills in patients with T2DM. | RCT | Intervention group: 50; Control group: 50 Mean age: Intervention group 1 = 49,78 ± 9,76 years Intervention group 2 = 53,26 ± 10,49 years Control group = 54,56 ± 9,88 years Mean duration of diabetes: Intervention group 1 = 8,09 ± 6,95 years Intervention group 2 = 8,9 ± 6,63 years Control group = 9,98 ± 7,51 years. |
| Nasab et al., 2017 | To investigate the effect of self-management education with telephone follow-up on diabetic patients of rural areas of Fars province in Lamerd city, Iran. | RCT | Intervention group: 32; Control group: 32. Median age: 52 years Median duration of diabetes: 6 years |
| Fernandes et al., 2016 | To evaluate the effectiveness of the telephone intervention for promoting self-care related to physical activity and following a diet plan in users with diabetes, compared to conventional monitoring of users over six months. | RCT | Intervention group: 104; Control group: n=106. Mean age: Intervention group = 62,9 ± 10,2 years Control group = 62,9 ± 10,3 years Mean duration of diabetes: not clear |
| Agarwal et al., 2019 | To conduct a pragmatic randomized controlled trial of the BlueStar mobile app on T2DM patients with poorly controlled blood sugar to determine if the use of the app would lead to improved HbA1c levels compared to controls in real-life clinical contexts. | RCT | Intervention group: 57; Control group: 63. Mean age: Intervention group = 51,5 ± 10,6 years Control group = 52,1 ± 10,7 years Total = 51,8 ± 10,7 years Time since diabetes diagnosis >5 years, n (%) Intervention group = 41 (37,3%) Control group = 47 (41,6%) Total = 88 (40%) |
| Bluml et al., 2019 | To determine whether augmenting DSME with support for an economically vulnerable population might better meet patient needs and reduce morbidity and premature mortality. | RCT | Intervention group: 22; Control group: 225. Mean age: Intervention group = 54,6 ± 10,00 years Control group = 54,2 ± 11,2 years Total = 54,4 ± 10,6 years Mean duration of diabetes: not clear |
| Author(s) | Technology Media | Measurement and Intervention | Outcome | Result |
|---|---|---|---|---|
| Greenwood et al., 2015 | Telephone, short video clips, messages, automatic health reminders | T0: Baseline T1: 3 months T2: 6 months Control group: The participants obtained education using booklets. This group continued receiving nurse care and reminders for HbA1C and health checks sent by post mail. Intervention group: The participants received a training session and expected feedback with communication by message or telephone. They received 84 sequential daily health sessions as a text document in the style of a PowerPoint slide or via short video clips. The participants received an automated health reminder every week to evaluate blood glucose. |
Primary outcome: HbA1C Secondary outcomes: Self-management, self-efficacy, and knowledge. |
Primary outcome: There were no significant differences in mean HbA1C between intervention and control groups at 3 and 6 months, with p=.53 and p=.55, respectively. Secondary outcomes: There was a significant difference between the control group and the intervention group in terms of carbohydrate management (p=.04), glucose monitoring (p=.001), and foot care (p=.02), respectively. There were no significant differences between the intervention and control groups in terms of knowledge (p=.55), self-efficacy (p=.70), and medication (p=.34), respectively. |
| Azami et al., 2018 | Telephone and movie clips | T0: Baseline T1: 3 months T2: 6 months Control group: The participants received individual-based education at three monthly intervals for 20-30 minutes. Health education with face-to-face consultations and pamphlets was used to give the usual diabetes care education. Intervention group: The participants received nurse-led DMSE, a detailed information booklet, viewed movie clips, attended four weekly group-based educational sessions, and followed up with weekly telephone calls. |
Primary outcome: HbA1C Secondary outcomes: Blood pressure, self-efficacy, self-management behaviors, body weight, quality of life, social support, and depression. |
Primary outcome: There was a significant difference between control and intervention groups in the HbA1C level, with p<.001. Secondary outcomes: There were significant differences between control and intervention groups in the systolic and diastolic blood pressure (p<.001), and diabetes self-management behavior (p=0,001), body weight (p<.001), self-efficacy, and social support (p<.001). There were no significant differences between control and intervention groups in terms of depression (p=.055). |
| Forjuoh et al., 2014 | A diabetes self-care software | T0: Baseline T1: 12 months Chronic Disease Self-Management Program (CDSMP) group: The participants were invited to attend a 6-week, classroom-based program for diabetes self-management. Personal Digital Assistant (PDA) group: The participants were taught to use a diabetes self-care software. Combination CDSMP and PDA group: The participants were given both the interventions. Usual Care (control) group: The participants received usual clinical diabetes care. |
Primary outcome: HbA1c Secondary outcome: BMI, blood pressure, and self-management behaviors. |
Primary outcome: There was no significant difference between CDSMP, PDA, and combination CDSMP and PDA groups in HbA1C (p=.771). Secondary outcome: There were no differences between the control and intervention groups in BMI, blood pressure, and self-management behaviors (statistical results were not reported). |
| Kim and Utz, 2019 | Telephone (smartphone and traditional phone) | T0: Baseline T1: 9 weeks T2: 3 months SM-HL/social media-based, health literacy group: The participants received education with smartphone-based technology for social media TEL-HL/telephone-based, health literacy group: The participants received diabetes education with traditional phone calls Usual care group: The participants received conventional education with brochure. |
Patient activation level, diabetes self-care behaviors, and HbA1C. | There were no significant differences between SM-HL, TEL-HL, and usual care groups in patient activation and HbA1C (p=.139). There was a significant difference between the SM-HL and TEL-HL groups in self-care behavior (p=.035). TE-HL group had a significantly higher score for self-care behavior than the usual care group (adjusted difference: 0.48; 95% CI: 0.11–0.86; observed power = 0.64). There was no difference between the SM-HL group and the usual care group in self-care behaviors (adjusted difference: 0.15; 95% CI: –0.26–0.56). |
| Maslakpak et al., 2017 | Telephone | T0: Baseline T1: 3 months Face-to-face family-oriented education group: The participants received education face-to-face twice a week in the first month and once a week in the second and third months. Telephone-based family-oriented education group: The participants received telephone-based family-oriented education twice a week in the first and second months and once a week in the third month. Control group: The participants received the paper-based educational materials of the teaching sessions. |
Self-care, HbA1C, cholesterol, and triglyceride. | There were significant differences in the mean and standard deviation of self-care scores for both the intervention and control groups with 100.82 ± 14.56, 92.93 ± 11.09, and 49.46 ± 16.35 (p=.0001), respectively. There was a significant improvement in the mean triglycerides 132.7±55.32mg/dl in the face-to-face group and 118.7±54.81mg/dl in the telephone group vs. 166.63±53.94mg/dl in the control group. The cholesterol values were 154.53±39.4 mg/dl in the face-to-face group and 148.53±49.4 mg/dl in the telephone group vs. 180.23±49.9 mg/dl in the control group. There was no significant decrease in HbA1C in face-to-face and telephone groups. |
| Chan et al., 2014 | Telephone | T0: Baseline T1: 3-4 months T2: 12 months JADE [Joint Asia Diabetes Evaluation]: The participants received their reports with the JADE portal 4 to 6 weeks later during a 2-hour nurse-led group empowerment class. The participants were followed up in their usual clinics every 3 to 4 months for HbA1c measurement and recording BP and body weight. JADE + PEARL: The participants received JADE Program and PEARL (Peer Support, Empowerment, and Remote Communication Linked by Information Technology). This program is a trained peer supporter who supports the participant via telephone, i.e., peer support calls twice a week for three months, every week for three months later, and every two months for 6 months later. |
Primary outcome: HbA1C Secondary outcomes: Psychological-behavioral parameters, and self-management. |
Primary and secondary outcomes: There were no significant differences between the JADE and JADE+PEARL groups in HbA1c (p=.97), self-management (p=.74), and psychological-behavioral parameters (p=.96). |
| Sherifali et al., 2019 | Telephone | T0: Baseline T1: 6 months T2: 12 months Control group: The participants received usual diabetes education. Intervention group: The participants received diabetes health coaching via telephone every week in the first six months and every month in the last six months and also received usual diabetes education. |
HbA1C, BMI, diabetes self-care activities, and health-related quality of life. | The study results included a mean BMI of 35.03 kg/m2, a weight of 97.14kg, and a mean HbA1C level of 8.98. The participants reported the disease-related quality of life to range from -3 to +1, diabetes-dependent quality of life with a mean score of -1.16, and mean weighted impact ADDQoL of -1.47. The participants reported following a general and special diet for 4.76 and 4.97 days, exercising an average of 4.25 times, and checking their blood glucose levels an average of 5.35 days in the past seven days. This study did not report statistical results. |
| Peimani et al., 2016 | Telephone and SMS | T0: Baseline T1: 3 months Control group: The participants received the usual care. Tailored SMS group: The participants received phone calls every week and were asked about receiving their messages regularly. Each person received 75% custom messages and 25% randomly selected messages. Nontailored SMS group: In this group, random messages were sent to everyone regardless of obstacles. In both the groups, an average of 7 messages were sent per week for three months. |
HbA1c, BMI, fasting blood sugar (FBS), lipid profile, SCI, DMSES, and DSCB-OA. | There was a significant difference between the tailored, non-tailored SMS groups, and the control group in mean BMI (p=.001), FBS (p<.001), and DSCB-OA (p<.001). There were no significant differences between the tailored, non-tailored SMS groups, and the control group in HbA1c (p=.190), triglyceride (p=.085), SCI (p=.89), and DMSES (=.091). |
| Nasab et al., 2017 | Telephone, lectures, group discussion, film presentation, and booklet | T0: Baseline T1: 3 months Control group: The participants received conventional care and usual education. Intervention group: The participants received four educational sessions, with each lasting 90 minutes. Educational methods included a combination of lectures, group discussions, film presentations, and booklets. The participants were followed up 12 times by telephone every week for three months. |
DSMQ, FBS, and LDL. | There was a significant difference between the intervention and control groups in DSMQ (p=.001) and FBS (p=.047). There were no significant differences between the intervention and control groups at pre-intervention and post-intervention in BMI (p=.730) and LDL (p=.674). |
| Fernandes et al., 2016 | Telephone | T0: Baseline T1: 3 months T2: 6 months Control group: The participants received education with a booklet. Experiment group: The participants received a telephone call every month for six months. |
Self-care activities | There was a significant difference found between the experimental and control groups in self-care (p=.000). |
| Agarwal et al., 2019 | Application of diabetes | T1: 3 months T2: 6 months Immediate treatment group (ITG): The participants received virtual coaching with the blue star application for six months. Wait-list control (WLC) group: The participants received usual care for the first three months and virtual coaching with the blue star application for three months later. |
Primary outcome: HbA1c levels. Secondary outcomes: Self-management, the experience of care, and self-reported health utilization. |
Primary outcome: There were significant differences between ITG and WLC groups in HbA1C (p=.19). Secondary outcomes: There was no significant difference between ITG and WLC groups in diabetes self-care behaviors, self-efficacy, quality of life, and healthcare utilization behaviors. This study did not report p-value. |
| Bluml et al., 2019 | Telephone | T0: Baseline T1:12 months Control group: The participants received usual care education face-to-face. Intervention group: The participants received regular phone calls from NCFH health navigators every two weeks for 3 months and every month for 12 months later. |
HbA1c levels, BMI, low-density lipoprotein cholesterol, triglycerides, depression status, and self-care. | There was no significant difference found between the control group and intervention group in HbA1c (p=.207), BMI (p=.517), HDL (p=.077), LDL (p=.098), triglycerides (p=.741), systolic (p=.211) and diastolic blood pressure (p=.987), healthy eating (p=.260), monitoring (p=.277), taking medication (p=.065), problem-solving (p=.366), reducing risk (p=.266), and healthy coping (p=.175). There were significant differences observed between the control group and intervention group in depression status (p=.031), cholesterol level (p=.001), and being active (p=.012). |
| Author(s) & Date of Publication | Measurement | Duration | Technology Media | Instrument | Result |
| Greenwood, Blozis, Young, Nesbitt, Quinn, June 21, 2015 [39] | Baseline. T1: 3 months. T2: 6 months. |
6 months. | Telephone, short video clips, message, automatic health reminder. | SDSCA | There was an increase in both groups, but the intervention group increased more for DM self-management on the aspect of carbohydrate spacing (p=0.04), glucose monitoring (0.001), and foot care (0.02) (there is a significant difference), no differences in aspects of physical activity, smoking, and medication. |
| Azami, Soh, Sazlina, et al, July 8, 2018 [22] | Baseline, T1: 3 months. T2: 6 months. |
6 months. | Telephone and movie clips. | DSMQ | Diabetes self-management behavior was significantly different between post-intervention groups (p=0,001). Self-management behavior intervention groups showed greater improvement compared with the control groups. |
| Forjuoh, Bolin, Huber, et al, January 23, 2013 [43] | Baseline, T1: 12 months. |
12 months. | A diabetes self-care software. | SDSCA | There is no difference in self-care in all groups. |
| Kim, Utz, September 24, 2019 [44] | Baseline, T1: 9 weeks. T2: 3 months. |
3 months. | Telephone (smartphone and traditional phone). | SDSCA | The self-care behavior score in the Telephone Health Literacy group was a significantly higher score than the control group at follow-up (adjusted difference 0.48; 95% CI 0.11–0.86; observed power = 0.64). The self-care behaviors between the SM-HL group and the usual care control group are not different (adjusted difference 0.15; 95% CI –0.26–0.56). A Self-care behavior at week nine of the intervention group showed a significant difference.[F (2, 137) = 3.45, p = 0.035]. |
| Maslakpak, Razmara, Niazkhani, November 22, 2017 [38] | Baseline, T1: 3 months. . |
3 months. | Telephone | SDSCA | There were significant differences in mean and standard deviation of overall self-care scores among group 1 (100.82 ± 14.56), group 2 (92.93 ± 11.09), and group 3 (49.46 ± 16.35) (P = 0.0001). The face-to-face group showed a significantly higher overall score than the group (P = 0.011). |
| Chan, Sui, Oldenburg, et al, April 28, 2014 [45] | Baseline, T1: 3-4 months. T2: 12 months. |
12 months | Telephone | SDSCA | SDSCA scores on the JADE and JADE + PEARL groups are no significant difference with p = 0.74. |
| Sherifali, Brozic, Agema, et al, October 17, 2018 [41] | Baseline, T1:6 months. T2: 12 months. |
12 months | Telephone and mail message. | SDSCA | The participants reported following a general and special diet for 4.76 and 4.97 days. Furthermore, participants reported exercising an average of 4.25 times in the past seven days and checking their blood glucose levels an average of 5.35 days in the past seven days. |
| Peimani, Rambod, Omidvar, et al, December 2, 2015 [40] | Baseline, T1: 3 months. |
3 months | Telephone and SMS | SCI | The mean SCI-R score significantly increased in the tailored and non-tailored SMS groups (P < 0.001), while it significantly decreased in the control group (P < 0.001). |
| Nasab, Ghavam, Yazdanpanah, Jahangir, Shokrpour, July/Sep 2017 [37] | Baseline, T1: 3 months. |
3 months | Telephone, lectures, group discussion, film presentation and booklet | DSMQ | There was a significant difference between the intervention and control groups in the sum scale DSMQ (p=0,001). |
| Fernandes, Reis, Torres, August 29, 2016 [21] | Baseline, T1: 3 months. T2: 6 months. |
6 months | Telephone. | DSQ. | The mean effect on self-care in the EG is statistically different from the mean in the CG (p=0.000), considering the period between T0 and T6. |
| Agarwal, Mukerji, Desveaux, et al, January 10, 2019 [42] | T1: 3 months. T2: 6 months. |
6 months | Application of diabetes and course | SDSCA | There was no difference in patient-reported diabetes self-care behaviors. |
| Bluml, Kolb, Lipman, February 13, 2019 [46] | Baseline, T1:12 months. |
12 months. | Telephone | AADE7. | The telephone frequency and the success of achieving the target have a positive relationship. |
| Author & Year | Time of Measurement | Diabetes Self Care Management | P-value | ||
| Intervention Group 1 | Intervention Group 2 | Control Group | |||
| Greenwood, Blozis, Young, Nesbitt, Quinn, June 21, 2015 [39] | General diet: Baseline T1: 3 months |
3.7 (2.4, 5.0) 4.7 (2.0, 7.0) |
None | 3.7 (3.2, 4.3) 4.9 (3.7, 6.1) |
0,95 0,84 |
| Specific diet: Baseline T1: 3 months |
3.5 (2.3, 4.7) 4.6 (1.7, 7.0) |
2.9 (2.4, 3.4) 4.2 (3.0, 5.3) |
0,09 0,68 |
||
| Carbohydrate spacing Baseline T1: 3 months |
2.7 (1.0, 4.6) 4.7 (3.4, 7.0) |
3.0 (2.3, 3.8) 3.9 (2.4, 5.4) |
0,65 0,04 |
||
| Exercise Baseline T1: 3 months |
2.7 (1.1, 4.3) 3.7 (0.60, 6.8) |
2.4 (1.7, 3.1) 2.6 (1.3, 3.9) |
0,58 0,07 |
||
| Medication Baseline T1: 3 months |
6.2 (4.9, 7.0) 6.3 (5.2, 7.0) |
6.5 (6.0, 7.0) 6.4 (5.4, 7.3) |
0,35 0,34 |
||
| Monitoring glucose Baseline T1: 3 months |
3.0 (1.1, 4.8) 5.1 (2.6, 7.0) |
3.6 (2.8, 4.4) 3.7 (2.1, 5.3) |
0,25 0,001 |
||
| Foot care: Baseline T1: 3 months |
2.5 (0.9, 4.2) 5.0 (1.7, 7.0) |
2.5 (1.8, 3.2) 3.8 (2.5, 5.2) |
0,97 0,02 |
||
| Azami, Soh, Sazlina, et al, July 8, 2018 [22] | Baseline, T1: 3 months. T2: 6 months. |
3.56 (1.22) 4.67 (1) 5.41 (1.15) |
None | 3.71 (1.40) 3.67 (1.37) 3.73 (1.40) |
0,001 ES=0,61 |
| Forjuoh, Bolin, Huber, et al, January 23, 2013 [43] | Baseline, T1: 12 months. |
Not clear | None | Not clear | No significant differences were observed. |
| Kim, Utz, September 24, 2019 [44] | Baseline, T1: 9 weeks. T2: 12 weeks |
SM-HL= 3.66 (1.15), TEL-HL=3.50 (1.38) SM-HL= 4.62 (0.96), TEL-HL=5.04 (0.79) HbA1C levels measurement |
None | 3.46 (1.09) 4.54 (1.05) HbA1C levels measurement |
0,476 0,035 |
| Maslakpak, Razmara, Niazkhani, November 22, 2017 [38] | Baseline, T1: 3 months. |
Face to face=49.36 ± 15.74 Face to face=100.82 ± 14.56 |
Phone based=56.13 ± 17.64 Phone based=92.93 ± 11.09 |
58.83 ± 18.95 49.46 ± 16.35 |
0,007 0,001 |
| Chan, Sui, Oldenburg, et al, April 28, 2014 [45] | Baseline, T1: 3-4 months. T2: 12 months. |
JADE+PEARL=48.7 (17.6) Not clear JADE+PEARL=4.09 (2.11 to 6.07) |
None | JADE=48.6 (17.5) Not clear JADE=4.56 (2.62 to 6.50) |
0,74 |
| Sherifali, Brozic, Agema, et al, October 17, 2018 [41] | Baseline: General diet Specific diet Exercise Blood-glucose testing Foot care |
All participant: 4.76 (2.76) 4.97 (1.57) 4.25 (2.61) 5.35 (2.34) 2.92 (1.85) |
None | The Diabetes Health Coaching be able to improve diabetes self care behavior | |
| Peimani, Rambod, Omidvar, et al, December 2, 2015 [40] | Baseline, T1: 3 months. |
Tailored SMS group= 55.41 ± 10.54 Tailored SMS group= 65.37 ± 10.26 |
Non-tailored SMS group= 55.43 ± 10.67 Non-tailored SMS group= 65.79 ± 9.99 |
54.57 ± 9.13 49.98 ± 11.25 |
0,001 0,001 ES= 0,606 |
| Nasab, Ghavam, Yazdanpanah, Jahangir, Shokrpour, July/Sep 2017 [37] |
Glucose management: Baseline, T1: 3 months. |
5.2 (1.04) 7.07 (1.53) |
None | 5.24 (1.39) 5.15 (1.32) |
0,000 |
| Dietary control: Baseline, T1: 3 months |
5.3 (2.04) 6.78 (1.41) |
None | 5.75 (1.57) 5.92 (1.28) |
0,015 | |
| Physical activity : Baseline, T1: 3 months |
6.9 (3.03) 8.1481 (1.68) |
None | 7.03 (2.67) 5.8148 (2.57) |
0,000 | |
| Health care use : Baseline, T1: 3 months |
7.5 (2.34) 7.4 (2.06) |
None | 6.7 (2.36) 6.66 (2.16) |
0,161 | |
| Sum scale : Baseline, T1: 3 months |
5.63 (1.77) 7.29 (1.13) |
None | 5.85 (1.4) 5.78 (1.2) |
0,000 | |
| Fernandes, Reis, Torres, August 29, 2016 [21] | Baseline, T1: 3 months. T2: 6 months. |
3.52±0.71 5.20±0.94 5.53±0.80 |
None | 3.55±0.76 4.34±1.10 4.10±1.18 |
0,000 |
| Agarwal, Mukerji, Desveaux, et al, January 10, 2019 [42] | T1: 3 months. T2: 6 months. |
Not clear | None | Not clear | 0,32 |
| Bluml, Kolb, Lipman, February 13, 2019 [46] | Baseline: Healthy Eating Being Active Monitoring Taking Medications Problem Solving Reducing Risk Healthy Coping |
168 (76.0)% 126 57.0 111 50.2 91 41.2 58 26.2 89 40.3 34 15.4 |
None | 159 71.6 111 50.0 116 52.3 106 47.7 43 19.4 80 36.0 28 12.6 |
0,293 0,139 0,670 0,164 0,085 0,359 0,400 |
| T1:12 months: Healthy Eating Being Active Monitoring Taking Medications Problem Solving Reducing Risk Healthy Coping |
78 46.4 55 43.7 50 45.0 48 52.7 34 58.4 51 57.3 18 52.9 |
64 40.3 31 27.9 44 37.9 42 39.6 29 67.4 39 48.8 10 35.7 |
0,260 0,012 0,277 0,065 0,366 0,266 0,175 |
||
showed significant diabetes self-management behavior in the post-intervention groups. In the intervention group, diabetes self-management was found to be increased with respect to carbohydrate spacing (p=.04), glucose monitoring (p=.001), and foot care (p=.02) [39]. While the combination of telephone with group discussions, booklets, and movies showed diabetes self-management behavior to be significantly different between the groups (p=.001), diabetes self-management behavior in the intervention group has been found to be greater than in the control group [22].
Telephone voice messaging effectively changed behavior toward glycemic control for twelve months [41]. Sending short messages according to patients’ needs or randomly following by telephone calls for three months had a significant effect on increasing the self-care inventory (SCI) score, with p <.001 [40].
4. DISCUSSION
All articles reviewed have been summarized based on the telenursing intervention's mode, duration, and effectiveness. The discussion of the three themes from the 12 articles analyzed in this study is provided below.
4.1. Theme 1: Mode of Telenursing
Technology media of telenursing are telephone, video clips or movies, automatic reminders, voice mail messages, and SMS. Via the telephone media, there is a two-way interaction between nurses and patients, so they feel comfortable, easy, simple, and inexpensively [46] and immediately get information about health problems [9, 50] anytime and anywhere [51]. Video movies, voice mail messages, and SMS provide no direct interactions between the patient and the nurse.
4.2. Theme 2: The Duration of Telenursing Intervention
The duration of telephone intervention for improving diabetes self-management behaviors is at least six months, and the minimum frequency of calls is once a week. Nurses make regular phone calls, resulting in intense communication with patients. Patients also feel motivated to change their behavior for the better. Information and motivation increase knowledge and confidence in managing the disease [52].
The 3-months duration of telenursing intervention through telephone and seven short messages is effective for improving diabetes self-management behavior [40]. The telenursing for improving diabetes self-management behavior is carried out through telephone, group discussions, film presentations, and booklets [37]. 6 and 12 months telenursing durations involving telephone calls alone have also been reported as effective [22, 46]. The author suspects that the time required is related to the methods and media used. The provision of education is effective when using several telecommunication media [37, 40].
4.3. Theme 3: Effectiveness of Telenursing
Telephone telenursing has been found to be effective and efficient and it can be carried out anywhere and anytime as needed. Therefore, health services need to utilize communication technology. The benefits obtained by using telenursing include faster and easier access to information [53, 54], monitoring of the patient's health condition by nurses [55], and increased patient self-care ability [56]. Another benefit is meeting physical and psychological needs, reducing physical contact during a pandemic, and replacing face-to-face consultations directly during the COVID-19 outbreak [57].
The use of a telephone as a medium for diabetes self-management education significantly increases the self-care score for type 2 diabetes mellitus [58] and diabetes self-management, as well as increases self-efficacy [22, 50] and healthy lifestyle [22].
This scoping review has focused on the diabetes self-management behavior of T2DM patients, which is the basis for nurses in providing health education. Diabetes self-management education is thus deemed essential. However, 8 articles did not describe the p-value of each self-management domain, 10 did not mention the size effect, and 2 articles did not mention the p-value. This limitation of the reviewed articles can as well be considered a limitation of this scoping review. In addition, another limitation of the review process was that a risk assessment of bias had not been conducted for each study.
Post-pandemic sustainable telenursing can be conducted by adhering to government or institutional policies, building and maintaining infrastructure [59], financing, maintaining patient and service provider safety, and supporting management [60].
5. PRACTICE IMPLICATIONS
Telephone calls are one of the potential methods of telenursing for diabetes self-management education, which can be practiced with an intervention time of at least three months.
CONCLUSION
The results of this review have found telephone calls as one of the potential methods of telenursing, with a minimum intervention time of three months. Modifications in other methods, such as video movies, voice mail messages, and SMS, can be made according to the needs and characteristics of the respondents. Telenursing must be maintained, especially considering the situation of the COVID-19 pandemic, as it makes health services easy, cheap, and fast.
LIST OF ABBREVIATIONS
| SMS | = Short Message Service |
| COVID-19 | = Coronavirus Disease of 2019 |
| ITG | = Immediate Treatment Group |
| T2DM | = Type 2 Diabetes Mellitus |
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
The name of the funding institution is the Research Directorate of Gadjah Mada University which financially supportsresearch with the 2022 Final Year Assignment Recognition Grant Program, with number 1525/UN1/DITLIT/Dit-Lit/PT.01. 05/2022.
ACKNOWLEDGEMENTS
The authors thank Gadjah Mada University for the 2022 Final Project Recognition Grant Program.
REFERENCES
| [1] | Soelistijo SA. Buku Pengelolaan Dan Pencegahan Diabetes Melitus Tipe 2 Dewasa di Indonesia. Perkeni 2019; p. 133. |
| [2] | Tetap P. Cegah, dan Atasi Diabetes Melitus 2020. pusat data dan informasi kementrian kesehatan RI 2020; 01-10. Available from: https://pusdatin.kemkes.go.id/resources/download/pusdatin/infodatin/Infodatin-2020-Diabetes-Melitus.pdf |
| [3] | Kemkes RI. Cegah Dan Atasi Diabetes Mellitus. Kemenkes: pusat data dan informasi kementrian kesehatan RI 2020. |
| [4] | Jing X, Chen J, Dong Y, et al. Related factors of quality of life of type 2 diabetes patients: A systematic review and meta-analysis. Health Qual Life Outcomes 2018; 16(1): 189. |
| [5] | de la Cruz JPS, Morales DLG, González-Castro TB, et al. Quality of life of Latin-American individuals with type 2 diabetes mellitus: A systematic review. Prim Care Diabetes 2020; 14(4): 317-34. |
| [6] | Riddle MC, Herman WH. The cost of diabetes cared an elephant in the room. Diabetes Care 2018; 41(5): 929-32. |
| [7] | Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low- and middle-income countries: A systematic review. BMJ Glob Health 2019; 4(1): e001258. |
| [8] | Ph L, Sari IP, Hermanto H. Gambaran tingkat stres pasien diabetes mellitus. Indones J Perawat 2018; 2(1): 41-50. |
| [9] | Souza-Junior VD, Mendes IAC, Mazzo A, Godoy S. Application of telenursing in nursing practice: An integrative literature review. Appl Nurs Res 2016; 29: 254-60. |
| [10] | Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns 2016; 99(6): 926-43. |
| [11] | Fan L, Sidani S. Effectiveness of diabetes self-management education intervention Elements: A meta-analysis. Can J Diabetes 2009; 33(1): 18-26. [Internet]. |
| [12] | Zheng F, Liu S, Liu Y, Deng L. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: A randomized controlled trial. J Diabetes Res 2019; 2019: 1-7. |
| [13] | Mikhael EM, Hassali MA, Hussain SA. Effectiveness of diabetes self-management educational programs for type 2 diabetes mellitus patients in middle east countries: A systematic review. Diabetes. Diabetes Metab Syndr Obes 2020; 13: 117-38. |
| [14] | Pamungkas RA, Limansyah D, Sudarman S, Siokal B. Self management program among type 2 diabetes mellitus patients: A literature review. Belitung Nurs J 2016; 2(3): 34-9. |
| [15] | Hildebrand JA, Billimek J, Lee JA, et al. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: A systematic review and meta-analysis. Patient Educ Couns 2020; 103(2): 266-75. |
| [16] | Hailu FB, Moen A, Hjortdahl P. Diabetes self-management education (DSME) – Effect on knowledge, self-care behavior, and self-efficacy among type 2 diabetes patients in Ethiopia: A controlled clinical trial. Diabetes Metab Syndr Obes 2019; 12: 2489-99. |
| [17] | Boro MFV, Hariyati TS. Implementasi telenursing dalam praktik keperawatan: Studi literature. Carolus J Nurs 2020; 2(2): 161-9. |
| [18] | Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: A systematic review.. Patient Educ Couns 2018; 101(8): 1310-21. |
| [19] | Firouzkouhi M, Abdollahimohammad A, Arulappan J, Nouraei T, Farzi J. Challenges and opportunities of using telenursing during COVID-19 pandemic: An integrative review. Front health inform 2021; 10(1): 98. |
| [20] | Petrelli F, Cangelosi G, Scuri S, et al. Diabetes and technology: A pilot study on the management of patients with insulin pumps during the COVID-19 pandemic. Diabetes Res Clin Pract 2020; 169(108481): 108481. |
| [21] | Diğin F, Kizilcik OZ. Telehealth and telenursing in COVID-19 pandemic. Turk Klin J 2021; 13(4): 987-93. |
| [22] | Fernandes BSM, Reis IA, Torres HC. Evaluation of the telephone intervention in the promotion of diabetes self-care: A randomized clinical trial. Rev Lat Am Enfermagem 2016; 24(0): e2719. |
| [23] | Azami G, Soh KL, Sazlina SG, et al. Effect of a nurse-led diabetes self-management education program on glycosylated hemoglobin among adults with type 2 diabetes. J Diabetes Res 2018; 2018: 1-12. |
| [24] | Aytekin Kanadli K, Ovayolu N, Ovayolu Ö. Does telephone follow-up and education affect self-care and metabolic control in diabetic patients? Holist Nurs Pract 2016; 30(2): 70-7. |
| [25] | Bağriaçik E, Bayraktar N. Effectiveness of training in disease management for patients with type 2 diabetes mellitus: A systematic review. Endocrinol Diabetes Nutr 2022; 69(5): 362-78. |
| [26] | Cunningham AT, Crittendon DR, White N, Mills GD, Diaz V, LaNoue MD. The effect of diabetes self-management education on HbA1c and quality of life in African-Americans: A systematic review and meta-analysis. BMC Health Serv Res 2018; 18(1): 367. |
| [27] | Nkhoma DE, Soko CJ, Bowrin P, et al. Digital interventions self-management education for type 1 and 2 diabetes: A systematic review and meta-analysis. Comput Methods Programs Biomed 2021; 210(172): 106370. |
| [28] | Eberle C, Stichling S. Effect of telemetric interventions on glycated hemoglobin A1c and management of type 2 diabetes mellitus: Systematic meta-review. J Med Internet Res 2021; 23(2): e23252. |
| [29] | Niu XD, Chi JT, Guo JB, et al. Effects of nurse-led web-based interventions on people with type 2 diabetes mellitus: A systematic review and meta-analysis. J Telemed Telecare 2021; 27(5): 269-79. |
| [30] | Robson N, Hosseinzadeh H. Impact of telehealth care among adults living with type 2 diabetes in primary care: A systematic review and meta-analysis of randomised controlled trials. Int J Environ Res Public Health 2021; 18(22): 12171. |
| [31] | El-Gayar O, Ofori M, Nawar N. On the efficacy of behavior change techniques in mHealth for self-management of diabetes: A meta-analysis. J Biomed Inform 2021; 119(June): 103839. |
| [32] | Anderson A, O’Connell SS, Thomas C, Chimmanamada R. Telehealth interventions to improve diabetes management among black and hispanic patients: A systematic review and meta-analysis. J Racial Ethn Health Disparities 2022; 9(6): 2375-86. |
| [33] | Masepia BD, Isworo A. Telemedicine for the self-management of type 2 diabetes: A literature review. J keperawatan Soedirman 2021; 16(1): 37-42. |
| [34] | Agastiya IMC, Kurianto E, Akalili H, Wicaksana AL. The impact of telehealth on self-management of patients with type 2 diabetes: A systematic review on interventional studies. Diabetes Metab Syndr 2022; 16(5): 102485. |
| [35] | Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology. Implement Sci 2010; 5(1): 69. |
| [36] | Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 2018; 169(7): 467-73. |
| [37] | Namjoo Nasab M, Ghavam A, Yazdanpanah A, Jahangir F, Shokrpour N. Effects of self-management education through telephone follow-up in diabetic patients. Health Care Manag 2017; 36(3): 273-81. |
| [38] | Hemmati Maslakpak M, Razmara S, Niazkhani Z. Effects of face-to-face and telephone-based family-oriented education on self-care behavior and patient outcomes in type 2 diabetes: A randomized controlled trial. J Diabetes Res 2017; 2017: 1-10. |
| [39] | Greenwood DA, Blozis SA, Young HM, Nesbitt TS, Quinn CC. Overcoming clinical inertia: A randomized clinical trial of a telehealth remote monitoring intervention using paired glucose testing in adults with type 2 diabetes. J Med Internet Res 2015; 17(7): e178. |
| [40] | Peimani M, Rambod C, Omidvar M, et al. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: A feasibility study. Prim Care Diabetes 2016; 10(4): 251-8. |
| [41] | Sherifali D, Brozic A, Agema P, et al. The diabetes health coaching randomized controlled trial: Rationale, design and baseline characteristics of adults living with type 2 diabetes. Can J Diabetes 2019; 43(7): 477-82. |
| [42] | Agarwal P, Mukerji G, Desveaux L, et al. Mobile app for improved self-management of type 2 diabetes: Multicenter pragmatic randomized controlled trial. JMIR Mhealth Uhealth 2019; 7(1): e10321. |
| [43] | Forjuoh SN, Bolin JN, Huber JC Jr, et al. Behavioral and technological interventions targeting glycemic control in a racially/ethnically diverse population: A randomized controlled trial. BMC Public Health 2014; 14(1): 71. |
| [44] | Kim SH, Utz S. Effectiveness of a social media–based, health literacy-sensitive diabetes self-management intervention: A randomized controlled trial. J Nurs Scholarsh 2019; 51(6): 661-9. |
| [45] | Chan JCN, Sui Y, Oldenburg B, et al. Effects of telephone-based peer support in patients with type 2 diabetes mellitus receiving integrated care: A randomized clinical trial. JAMA Intern Med 2014; 174(6): 972-81. |
| [46] | Bluml BM, Kolb LE, Lipman R. Evaluating the impact of year-long, augmented diabetes self-management support. Popul Health Manag 2019; 22(6): 522-8. |
| [47] | Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000; 23(7): 943-50. |
| [48] | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009; 339(jul21 1): b2535. |
| [49] | Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol 2005; 8(1): 19-32. |
| [50] | Adiputra AB. Aplikasi media telenursing pada tata laksana diabetes mellitus: Sebuah scoping review. J Islam Nurs 2019; 4(1): 83-9. |
| [51] | Liu L, Ogwu SM. A meta-analysis of mobile health and risk reduction in patients with diabetes mellitus: Challenge and opportunity. J Mob Technol Med 2012; 1(3): 17-24. |
| [52] | Malini H, Yeni F, Pratiwi CA, Lenggogeni DP. Associated factors of self-management in type 2 diabetes mellitus at community health center. J keperawatan Soedirman 2020; 15(2): 24-30. |
| [53] | Padila P, Lina LF, Febriawati H, Agustina B, Yanuarti R. Home visit berbasis sistem informasi manajemen telenursing. Jurnal Keperawatan Silampari 2018; 2(1): 217-35. |
| [54] | Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: A systematic review. Patient Educ Couns 2018; 101(8): 1310-21. |
| [55] | Wynchank S, Sabbah N. eHealth and telenursing. In: The e-Medicine, E-Health, M-Health, Telemedicine, And Telehealth handbook. London New York: CRC Press Taylor & Francis Group Boca Raton 2016; pp. 119-44. |
| [56] | Pratama WW, Nurhest POY, Sulistiowati MD. The effect of telenursing on self-care of patients with chronic diseases. Community Publ Nurs 2019; 7(2): 87-94. |
| [57] | Raafi VA, Saryono S, Sari Y. Implementasi telehealth pada pasien diabetes melitus saat pandemi Covid-19: Tinjauan sistematis. NURSCOPE J Penelit dan Pemikir Ilm Keperawatan 2021; 7(1): 45-52. |
| [58] | Sarayani A, Mashayekhi M, Nosrati M, et al. Efficacy of a telephone-based intervention among patients with type-2 diabetes; a randomized controlled trial in pharmacy practice. Int J Clin Pharm 2018; 40(2): 345-53. |
| [59] | Johnson KA, Parkinson C, Johnson MM, Hamburger ML. Using telemedicine interventions during COVID-19 to expand care post COVID-19. Am J Manag Care 2023; 29(1): e31-5. |
| [60] | Ashley C, Williams A, Dennis S, McInnes S, Zwar NA, Morgan M. Telehealth's future in Australian primary health care: A qualitative study exploring lessons learnt from the COVID-19 pandemic. BJGP Open 2023; 7(2): BJGPO-0117. |










