All published articles of this journal are available on ScienceDirect.
Simulation in Basic Nursing Student Education: Uses and Barriers
Abstract
Introduction:
In nursing, simulation has demonstrated its educational value as an active form of teaching. However, its integration into educational programmes and faculty practices remains limited.
Objectives:
The purpose of this research was to explore the place of simulation in teaching activities for the basic education of undergraduate nursing students and identify barriers to its implementation.
Methods:
An online questionnaire survey was used for teachers in the Higher Institutes of Nursing and Technical Health Professions. A total of 90 teachers responded. The data collected were analysed using descriptive statistics.
Results:
Simulation was present in the practices of 63.3% of teachers. The most used types were procedural simulation (36.4%), role-playing (31.5%), standardised patients (14.4%), and hybrid simulation (9.1%). The areas of use were technical skills (24.2%), knowledge acquisition (19.2%), communication (20.8%), emergency management (10.8%), team management (10%), and error management (10%). A range of barriers to the implementation of the simulation was revealed, such as a lack of organisational resources and teacher training.
Conclusion:
This study provided insight into the use of simulation in nursing student education and highlighted the challenges to its use. Faculty recommendations support the formal integration of simulation into nursing education programmes.
1. INTRODUCTION
The adoption of simulation in health care has increased over the past few decades [1-3]. The evolution of its different forms has allowed it to become an active and sharp pedagogy [4-6]. However, some obstacles limit its integration into teachers’ practices.
In nursing, simulation has demonstrated its potential [7-9]. It is a ubiquitous teaching strategy in various training programmes: nursing, obstetrics, emergency, anaesthesia, neonatal care, and mental health [9]. It is a powerful lever for improving the quality of care and enhancing patient safety [10]. The wide range of simulation types and their rich applications allow teachers to combine them with traditional teaching methods to bridge the gap between theory and clinical placements [11, 12].
Simulation perfectly meets the learning needs of nursing students; it allows the development of technical and non-technical skills [13-15]. Many studies have documented the mobilisation of simulation to reinforce theoretical knowledge, stimulate critical thinking, promote reflective attitudes [16, 17], and improve clinical performance [18]. Similarly, simulation has a place in improving communication skills and teamwork [19]. It provides a safe context for students to apply and implement the knowledge gained in the classroom.
Although the investment in simulation has increased considerably, obstacles exist to the deployment of this formative strategy. The implementation of these tools requires significant budgetary, structural, and logistical investments. Simulation-based teaching also requires innovative professional and organisational skills. This encourages a commitment from the institutional authorities to facilitate its integration into the training of nurses.
2. LITERATURE REVIEW
2.1. Uses and Practices of Simulation in Nursing
The healthcare environment is constantly evolving due to significant epidemiological changes and technological and scientific advances [20]. This context calls for a competent professional capable of managing these changes. The use of simulation has become a much greater necessity in nursing education to keep up [21].
Increasingly, studies have confirmed the value of simulation in nursing education [17, 22, 23]. This teaching technique accelerates learning and gives students the necessary skills to prepare them for clinical settings. The simulation context allows reproducing scenarios as close to reality as possible, providing a framework with the freedom to make mistakes [4]. The learner applies what they have learned in a safe environment, and the debriefing they receive allows them to identify errors and adjust their learning.
The many simulation techniques can be included in cognitive, emotional, and psychomotor learning styles. Low-fidelity or partial task forms allow repetitive technical training until the gesture is mastered [10]. The more advanced versions offer a framework that combines several contextual factors to reproduce scenarios that become more difficult as they progress by actively involving the student in their resolution. Simulation thus contributes positively to the development of clinical reasoning.
Simulation has also emerged as a valuable tool for improving soft skills. Its beneficial effects on team management, communication, and even crisis management have been supported by several studies [14, 15, 19]. However, given the wide range of accessible simulation tools, it is crucial to be aware of the pedagogical intentions and practices that accompany them.
2.2. Obstacles to the Practice of Simulation
The value of simulation in the training of nursing students is indisputable. Teachers report that these resources help them to maximise their efforts [15]. However, the effective and efficient use of simulation techniques is hampered by several factors. Many studies have examined these barriers [13-24, 26]. One of the studies identified seven categories: time, training, perception of ownership of tools in the course, equipment and space planning, funding, and personnel and student engagement and involvement in simulations [27].
Simulation in its advanced forms has seized the opportunity offered by technological progress. New tools have become highly sophisticated, including high-fidelity interactive manikins and virtual reality, significant gains for simulation. However, this evolution is not always equal to the performance of practitioners. Teachers are left to their own devices to use these sophisticated instruments [26, 27], and their application often destabilises them, hence the need for support for the safe and effective use of these technologies is required [28, 29].
Seen from another angle, the integration of these advanced tools into teaching practices requires considerable knowledge. According to several studies, this implementation translates into new pedagogical requirements to achieve a convincing articulation between knowledge and methods [27]. Therefore, its success can only be ensured by careful educational restructuring in accordance with standardised norms of good practice [5].
In addition to these specific challenges, managing simulation use in training is hampered by a lack of financial resources, a lack of facilities and equipment, and a shortage of expert personnel in the field [27, 26].
2.3. Background
The use of simulation as a teaching technique to train health professionals has developed considerably. Many countries in Europe and North America, as well as Australia, support its use as a supplement to traditional teaching and learning techniques [30] or even its formal integration into training programmes [2].
In North America, simulation reflects excellence in training and is integrated into basic and continuing education programmes. This success is supported by the field of research, which has evolved considerably. Research is interested in the study of simulation in all its aspects, including its objects and tools [10]. Studies have shown that under certain circumstances, such as the availability of sufficient experienced instructors, simulation can replace up to 50% of nursing placements [20]. These results were sustained during the unprecedented COVID-19 crisis when the simulation was widely used and able to substitute hours of internships [31].
Following the example of other countries, Morocco is part of this vast project of pedagogical development of simulation. For years, efforts have been made in this direction, through multiple partnerships with organisations to promote the use of simulation. We highlight the contribution of some non-governmental organisations and the Moroccan Society of Medical Simulation to the generalisation of simulation laboratories at the level of Higher Institutes of Nursing and Health Technicians (Ministry of Health, 2022). The training field has seen a growing interest, especially through the creation of specialised masters and university degrees for the training of trainers in simulation pedagogy.
In addition to these initiatives, the national research field is experiencing growing interest in simulation. Different publications have aimed to examine the various uses of simulation to improve the performance and capacities of health actors [32-34], its characteristics as a learning strategy [35, 36], and the perceived usefulness of learning through simulation [37].
These advances support and accompany the reforms organising the training of nurses and health technicians in Morocco. The new training architecture is part of the bachelor–master–doctorate system (LMD), with the creation of the Higher Institutes of Nursing and Health Technicians non-university higher education institutions. This strategic redesign aimed to enhance the quality of health professional training and improve the quality of care. However, despite the increased success of simulation, its use by teachers in the training of nursing students in our context remains less explored.
Our study aimed to address two objectives: (1) to explore the use of simulation in nursing education and (2) to describe the different difficulties and obstacles encountered by teachers in the implementation of simulation.
3. MATERIALS AND METHODS
3.1. Design
To meet the objectives, a descriptive study with a quantitative design was chosen. The target population was permanent teachers at the level of the Higher Institutes of Nursing and Health Technology.
3.2. Study Environment
This study was conducted in the Higher Institutes of professional nurses and health technics (ISPITS), located in different regions in Morocco. These institutes are among the establishments of higher education that are not part of the universities, and which are under the supervision of the government authority of health. The main missions of ISPITS in the new LMD architecture are: basic training (bachelor's degree, master's degree, doctorate), continuing education, and scientific research, with a view to the development of professions related to nursing sciences and health techniques.
3.3. Data Collection
Our choice for the study was a quantitative survey using a questionnaire. We chose this tool to cover a maximum of the target population and collect precise and easily quantifiable information. This instrument has been structured on the basis of the recommendations of the guide to good simulation practices and the mission report “State of the art (national and international) in terms of simulation practices in the field of health”, published by the Haute Autorité de Santé [38].
The questionnaire was composed of 25 items organized in three parts. The first part dealt with the general and professional characteristics of participants: gender and age, level of education, and seniority in teaching. The second part questioned the pedagogical aspects mobilised by the teachers within the framework of simulation use, including use or not of simulation, beneficiaries of simulation, semesters in which simulation was offered, methods of simulation used, the average duration of the sessions, fields of use, and supports. The last part examined the difficulties and needs related to the use of simulation. The questions were asked in closed, open and multiple-choice formats.
Before the final administration of the questionnaire, a pre-test was conducted with eight tenured teachers to check for clarity and understanding of the questions. Adjustments were deemed necessary. The questionnaire was conducted via Google Forms® software and sent by email to the teachers and coordinators of the institutes. The data collection lasted for four months between May and August 2022.
3.4. Data Analysis
The collected data were automatically transferred from Google Forms® to a table in Microsoft Excel. The data processing was based on the description of the frequencies and percentages of the different categories covered by the questionnaire items. They were presented as tables and figures.
4. RESULTS
4.1. Demographic Characteristics of Participants
Ninety faculty members responded to our study. Characteristics collected from the participants included age, gender, education level, and years of experience in nursing education (Table 1).
| Age Range | N (%) |
|---|---|
| 20–30 years | 4 (4.4%) |
| 30–40 years | 57 (63.3%) |
| 40–50 years | 23 (25.6%) |
| ≥50 years | 6 (6.7%) |
| Gender | |
| Female | 70 (77.8%) |
| Male | 20 (22.2%) |
| Level of Study | |
| The first cycle of paramedical studies | 8 (8.9%) |
| The second cycle of paramedical studies | 35 (38.9%) |
| Master in Nursing and Health Technology Education | 35 (38.9%) |
| Doctorate | 12 (13.3%) |
| Teaching Experience | |
| <5 years | 29 (32.2%) |
| 5–10 years | 30 (33.3%) |
| 10–20 years | 25 (27.8%) |
| ≥20 years | 6 (6.7%) |
| Use of Simulation as a Teaching Tool | N (%) |
|---|---|
| No | 33 (36.7%) |
| Yes | 57 (63.3%) |
| Use of Simulation by Training Option | N (%) |
| Nurse in anaesthesia and intensive care | 2 (3.5%) |
| Mental health nurse | 7 (12.3%) |
| Emergency and critical care nurse | 1 (1.8%) |
| Multi-skilled nurse | 32 (56.1%) |
| Physical therapies/physiotherapy | 2 (3.5%) |
| Radiology technician | 4 (7.0%) |
| Midwife | 19 (33.3%) |
The most represented age group was 30–40 years (63.3%), with a predominance of women (77.8%) and only 22.2% men. The training of the teachers ranged from basic training in the first cycle of paramedical studies (8.9%) to the doctoral cycle (13.3%), with a predominance of pedagogical training in nursing (77.8% of the participants had training in pedagogy). Their teaching education was also variable, that was 38.9% studied in the second cycle of paramedical studies, and 38.9% had a master’s degree in nursing and health technology pedagogy. The teaching experience of the participants varied and was as followed; less than 5 years (32.2%), between 5 and 10 years (33.3%), between 10 and 20 years (27.8%), or more than 20 years (6.7%).
4.2. Characteristics of Simulation Teaching Practices
4.2.1. Use of Simulation
Of the 90 participants, 57 (63.3%) reported using simulation in their teaching activities (Table 2). Among them were multipurpose nurses (56.1%), midwives (33.3%), mental health nurses (12.3%), anaesthesia-resuscitation nurses (3.5%), and emergency and intensive care nurses (1.8%) (Table 2).
4.2.2. Use of Simulation by Level
As shown in Table 3, simulation was used for different levels of basic nursing training: 18 used it for one level only (31.6%), 23 for two levels (40.35%), 14 for three levels (24.6%), and only two during the whole training course (3.5%).
4.2.3. Characteristics of Simulation Activities used by Teachers
The results showed that 36.4% of the teachers used procedural simulation in their practices, followed by situational simulation (role-playing) at 31.5%, and standardised patients and hybrid simulation were used by 14.4% and 9.1%, respectively. Serious games, high-fidelity simulation, and virtual reality based on screen interfaces were rarely used. The average time reserved for simulation sessions was more than 10 hours for 47.4% of teachers. Regarding the areas of use, according to Table 4, we note a strong use of simulation for the development of technical skills (24.2%) and knowledge acquisition (19.2%), as well as communication (20.8%). The simulation was also used for emblematic situations such as team management (10.0%), error management (10.0%), and emergency management (10.8%).
4.2.4. Use and Type of Scenarios
As shown in Table 5, 62.9% of the teachers reported using scenarios as a support in their practices. The scenarios used in simulation mostly concerned the field of obstetrics (53.6%), comprising neonatal resuscitation (26.8%), pre-and postnatal consultation (9.7%), delivery (7.3%), postpartum haemorrhage (7.3%) and family planning (2.4%). The other types of scenarios were marked by their heterogeneity such as cardiorespiratory arrest (4.9%), bad news (14.6%), therapeutic incidents (7.3%), basic nursing care (12.2%), and first aid (7.3%).
| Use of Simulation by Semester | N (%) | Total/level |
|---|---|---|
| S1 | 4 (7.0%) | 18 (31.6%) |
| S2 | 10 (17.5%) | |
| S3 | 2 (3.5%) | |
| S4 | 2 (3.5%) | |
| S1, S2 | 8 (14.0%) | 23 (40.35%) |
| S1, S3 | 2 (3.5%) | |
| S2, S3 | 7 (12.3%) | |
| S2, S4 | 3 (5.3%) | |
| S1, S4 | 1 (1.8%) | |
| S2, S6 | 1 (1.8%) | |
| S3, S4 | 1 (1.8%) | |
| S1, S2, S3 | 10 (17.5%) | 14 (24.6%) |
| S1, S2, S5 | 2 (3.5%) | |
| S1, S3, S4 | 2 (3.5%) | |
| S1, S2, S3, S4, S5, S6 | 1 (1.8%) | 2 (3.5%) |
| S2, S3, S4, S5, S6 | 1 (1.8%) |
| Simulation Technique Used | N (%) |
|---|---|
| Role-playing situation | 43 (31.5%) |
| Standardised patient or simulated patient | 21 (14.7%) |
| Procedural simulation | 52 (36.4%) |
| Virtual reality based on screen interfaces | 6 (4.2%) |
| Hybrid simulation (combination of several techniques) | 13 (9.1%) |
| Serious games | 2 (1.4%) |
| High-fidelity manikin | 4 (2.8%) |
| Average Time of Simulation Use | |
| Less than 5 hours | 11 (19 .3%) |
| Between 5 and 10 hours | 19 (33.3%) |
| More than 10 hours | 27 (47.4%) |
| Area of Simulation Use | |
| Knowledge acquisition | 23 (19.2%) |
| Error management | 12 (10.0%) |
| Technical skills | 29 (24.2%) |
| Communication | 25 (20.8%) |
| Team management | 12 (10.0%) |
| Emergency management | 13 (10.8%) |
| Leadership | 6 (5.0%) |
| Use of Scenario for Simulation | N (%) |
|---|---|
| No | 13 (37.1%) |
| Yes | 22 (62.9%) |
| The Type of Scenario Used | N (%) |
| Pre- and postnatal consultation | 4 (9.7%) |
| Family planning | 1 (2.4%) |
| Delivery | 3 (7.3%) |
| Cardiorespiratory arrest | 2 (4.9%) |
| Postpartum haemorrhage | 3 (7.3%) |
| Neonatal resuscitation | 11 (26.8%) |
| Bad news announcement | 6 (14.6%) |
| Therapeutic incidents | 3 (7.3%) |
| Basic nursing care | 5 (12.2%) |
| First aid | 3 (7.3%) |
4.3. Obstacles to the Implementation of the Simulation
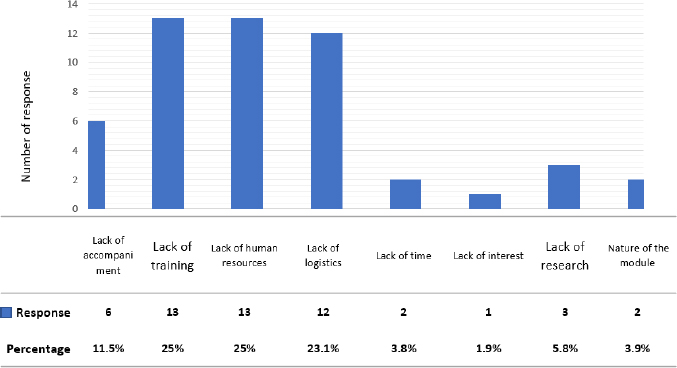
A variety of barriers were reported to the implementation of simulation by teachers (Fig. 1). Resources presented the greatest obstacle: a lack of logistics (23.1%) and a lack of human resources (25%). The majority of teachers reported difficulties integrating simulation into their practices. A lack of training was reported (25%), along with a lack of accompaniment (11.5%) and a lack of research (5.8%). Notably, all the teachers wanted to benefit from simulation training and confirmed that its integration into training programmes can improve the quality of teaching services.
5. DISCUSSION
In this study, we tried to illustrate the modalities of simulation use by teachers at the level of Higher Institutes of Nursing and Technical Health Professions. A total of 90 teachers voluntarily participated in this study. Most were early in their teaching careers with specialised training in pedagogy and nursing.
The results indicated that 63.3% of faculty members integrated simulation into their practice, a fairly modest use compared to the recent success of this advanced method to support nursing learning [3, 12]. The literature increasingly favours formalising the use of simulation in training programmes [9].
The impact of simulation on the development of technical and soft skills has been supported by several studies [6, 14]. This study found that teachers mobilised simulation for the development of different skills, including technical skills, communication, and team management. These results are supported by the recent literature review by [39], which endorsed the use of simulation for the integration of skills necessary for the training of qualified nurses.
Our study highlights heterogeneity in the type of simulation used by teachers, ranging from low-fidelity simulations to high-fidelity simulations that integrate new technology, such as serious games and virtual reality based on-screen interfaces. However, the use of the latter remains very low. This can be attributed to the lack of expertise in using the new technology, which presents a new challenge for teachers to develop their technical performance [40, 41, 26].
Most teachers reported informal use of simulation in their practices because many obstacles hinder its optimal use. In this sense, we cite the lack of logistics (23.1%) and lack of resources (25%). These results corroborate the data of several studies [23, 26, 29]. One of the studiesnoted that implementing simulation in training requires an increased investment in technical and human resources, especially with the integration of new technologies [25]. In addition, the participants in this study raised the issue of the lack of information and training on simulation teaching practices. Certainly, the acceptance of new approaches and their integration into training goes beyond the simple application of an instrument; it is rather a question of questioning the pedagogical and didactic practices that accompany it. The new recommendations of the Haute Autorité de Santé impose the application of specific standardised protocols to protect and optimise the use of simulation [5]. Similarly, the standards committee of the International Nursing Association for Clinical Simulation and Learning (INACSL) has listed certain standards as a standardised design framework [3]. The training of simulation users is thus necessary to guarantee its effectiveness and secure its practice.
CONCLUSION
This study charted the use of simulation in basic nursing student education. This use has raised diverse applications for different levels and training options, with the flexibility of integration in a variety of situations for technical and non-technical skill development. In addition, the study highlighted a series of difficulties encountered by users, which hindered the effective and efficient implementation of this educational approach. In light of these initial results, the time appears right to train pedagogical actors to generalise this teaching strategy and maximise the effectiveness of its use in teachers’ practices.
A study on training modalities is necessary to develop the skills of trainers and improve the teaching and learning process of simulation in our context. From this perspective, our research project will attempt to propose an innovative system of continuous training in simulation based on the analysis of the activity of expert simulation trainers.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals were used in the studies that form the basis of this research. All procedures performed in studies involving human participants were in accordance with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The teachers’ consent was obtained at the beginning of the questionnaire in the note presenting it, concerning the commitment to respect the anonymity and confidentiality of the data.
AVAILABILITY OF DATA AND MATERIALS
The data support the findings of this study are available from the corresponding author [F. B], on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors do not declare any conflict of interest, financial or otherwise
ACKNOWLEDGEMENTS
We would like to thank all the teachers who agreed to participate in this study.


