All published articles of this journal are available on ScienceDirect.
Evidence-Based Knowledge, Beliefs, and Skills Among Healthcare Professionals
Abstract
Introduction:
Common for all research is the approach that Evidence-based Practice (EBP) is a wide range term and essential for a good patient-centered treatment of health care providers.
Objective:
Objective of this study is to analyze the level of Knowledge, Beliefs and skills of healthcare workers The Aim of the article was to evaluate and understand the levels of Evidence Based Practice knowledge, beliefs, and skills of healthcare workers in Kosovo.
Methods:
We used a sample 611 healthcare workers randomly from seven municipalities of Kosovo who works in three levels of healthcare facilities to participate in this cross-sectional survey.
Results:
Sixty-five percent (65%) of the participants were female. The mean age of participants was 38 years. 78% of participants were working in the public health facilities. Kosovar healthcare professionals have a lower point on the use of EBP (2.15±0.65), and on attitudes toward EBP (3.60±1.06), and highest points on knowledge about EBP (5.34±1.04). The nurses found to have higher point in the dimension of use of EBP compared to medical doctors (p<0.05). Health workers working in tertiary health facilities had higher points on the use of EBP compared to those working in primary health care facilities in post hoc analyses (p<0.05). Healthcare workers working in primary health care facilities had lower points on the attitudes toward EBP compared to those working in secondary and tertiary health care facilities (p<0.05). Health workers living in urban setting had a higher points of the dimension knowledge of EBP compared to those living in rural area (p<0.05).
Implication for Nursing:
Implication of the study are as following: Raise the awareness of importance to use EBP in health professionals, the research can be used to build guidelines for use of EBP in Kosovo as transition country. Also, will help nurses to provide better services in line with developed countries.
Conclusion:
This study shows the importance of the use of EBP, attitudes and knowledge in healthcare institutions and its implementation Evidence-based practice (EBP).
1. INTRODUCTION
Evidence-based Practice (EBP) is a fundamental part of the daily work of professionals in healthcare and became more and more famous in the last three decades. Thereby, there is a growing body in the literature that has been focused on the principles, framework and necessary steps to implement EBP [1-5]. Moreover, studies on the development of specialized scales and questionnaires to measure the implementation, learning assessment tools and also the beliefs and attitudes, ability, knowledge plus practices of nurses [5-7] including the validation of Evidence-based Practice scale in different languages [8, 9].
Scholars argue that EBP is a wide range of terms and essential for the good patient-centered treatment of health care providers. Decision-making in this context should be based on the current, related and evidence-based research, combined with clinical experience and knowledge and also the values and perceptions of patients to achieve the best reachable outcome for them [1-3, 10]. Therefore, the impact of EBP contains different advantages. Besides decreasing costs or better cost-effectiveness [11-13] benefits for the patients in the enhancement of treatment options, better judgement of available therapies, more weight to their values and a higher quality of life were described [11-14]. Furthermore better patients outcome was measured by lower mortality and shorter stay at the hospital [2]. Advantages for healthcare providers, in detail higher awareness of their specific roles and for themselves, better team cohesion and lower attrition were described [13, 15].
The adoption of EBP has been focused on different countries and contexts such as empirical studies in Asia [16-18] and Africa [19, 20]. In the Balkan Region otherwise, studies could be only found marginally. Here, especially for Kosovo, a study [21] explored the lack of communication between healthcare workers, policy makers, and other barriers at the implementation of guidelines. As a result, the rationale behind this study is to examine the extent healthcare professionals in Kosovo employ EBP as EBP provides an excellent opportunity for health professionals in Kosovo to provide better services to patients and meet the consistently changing demands in healthcare institutions. Therefore, the purpose of this study is to evaluate and understand the levels of Evidence-Based Practice knowledge, beliefs and skills of healthcare workers in Kosovo. This study employs the Evidence-based Practice Questionnaire (EBPQ), developed by Upton & Upton [22] and the validity and internal validity has been tested by other studies [18, 23-27].
1.1. Literature Review
Several studies examined the dimensions of Evidence-Based Practice such as the practice, knowledge and skill and attitudes/beliefs. With regards to beliefs including attitudes and perceptions studies show positive results of nurses towards EBP among the majority of participants [15, 17, 18, 28, 29]. Another group of studies found moderating levels in attitudes and perceptions of nurses in relation to EBP [26, 30]. The attitudes and perceptions in relation to EBP according to studies are influenced by different factors such as positive development work experience [17] unit culture [29] and level of education or graduation [31, 32], and negative aspects self-awareness of own limited autonomy [23] and a lack of time to search and read scientific articles [28]. In addition, studies found that between barriers and attitudes a significant correlation was founded [23] but barriers should have only a minimal influence on the implementation of EBP [24]. Studies show that the lack of nurses' knowledge and self-belief to carry out research and apply findings in clinical settings in practice [33] and the factors that lead to misconceptions that are related on teaching on EBP [34] and barriers that are related to the lack of authority to change current practices, challenge to understand statistical analysis and nurses perception that knowledgeable colleagues do not share their knowledge. The perceived barriers on regards to attitude and barriers may change from country to country as the studies show due to the trainings on nurses [35]. Therefore, the continuation of nurses education ad attempting to minimize barriers may increase the use of EBP [36].
Studies show that education and training influence the attitudes of health professionals towards EBP as well as the differences in health professionals regards to attitudes toward EBP. Another study [27] shows that after an EBP-education attitudes not significantly increased, but six months later the intervention group had a significantly higher level of attitudes before after twelve months the improvement began to decrease [27]. Opposite to this, Kim, et al. [25] ascertain after a ninth-month fellowship that practice, skills and knowledge increased but not the attitudes. Also, implemented a course with a duration of six months and found that attitudes toward EBP were constant moderate positive [30]. Thiel and Ghosh [29] show that the awareness of own attitude could be a benchmark for the implementation process. In their review, Mallion and Brooke [13] present that positive attitudes have no influence on the implementation of EBP and increasing skills and knowledge. However, another systematic review indicates that attitudes towards EBP are associated with higher research utilization specifically among nurses [37]. In addition, it was [16] found that physicians had significantly higher awareness and attitudes towards EBP than nurses.
These variations were noticeable for EBP knowledge as well. According to a study by Upton and Upton [7], pediatricians, radiologists, and orthoptists had lower knowledge levels than physiotherapists, speech therapists, and psychotherapists. Additionally, there are differences within one field. For instance, hospital doctors perceive their understanding of EBP as being higher than general practitioners [7, 38]. In one research, nurses demonstrated average knowledge, while a sudy [26] found lower scores. A different study [18] revealed that institutional readiness and a lack of adequate EBP knowledge were significant positive predictors of EBP implementation. The authors show a strong link between training in research methodology and increased EBP activity [28]. Furthermore, according to one study, knowledge increased significantly nine months after a fellowship [25] and six months after an intervention [27] before beginning to decline twelve months later. Additionally, the higher chance of early EBP implementation following training [20] or educational initiatives in the form of collaboration between healthcare professional and clinical educators [39] was examined. Similarly, a study [37] reported in its systematic review that taking courses and attending conferences had a favorable impact on how people used research.
The skills for EBP, are the final factor to be investigated, depending on the use of several EBP practice procedures in daily work. The concept was originally composed of five steps [1, 2], including: Translation from open-ended to specific queries, systematic analysis of the available data, a critical evaluation of the evidence's applicability to clinical problems, Treatment application and implementation evaluation [30]. This pattern has been modified to a seven-step model. The author group expanded Step 4 to include clinical expertise and patient preferences and completed the model with Step 6 for sharing results with colleagues and institutions in round tables, conferences, and journals. The author group added the attitude of health care professionals in the sense of cultivating the spirit of inquiry as Step 0, specified Step 1 with the PICOT-Scheme, and extended Step 4 with clinical expertise and patient preferences. Another study [30] postulated before that confronting student with EBP-Paradigm could increase this development. Also, a dew studies [20] and [19] showed insufficient skills, especially for Steps 1-3. A general lack was founded in others [29] and [26]. A study [25] showed an increasing level of skills after a ninth-month fellowship-program, but opposite to this [31] observed a general need to enhance these in the US.
In summary, the studies above show the importance regards to the use of EBP knowledge, and attitudes and the importance of implementation of EBP for healthcare professionals. Therefore, the aim of this study is to understand the extent of use of EBP, knowledge and attitudes of healthcare professionals in Kosovo. This topic is relevant in the case of Kosovo due to the challenges that institutions face to implement reforms in various fields [40, 41], including healthcare institutions.
2. MATERIALS AND METHODS
This study employs a cross-sectional study of the use of EBP, knowledge, and attitudes of healthcare professionals. The sample of this study consists of 611 healthcare professionals randomly from seven municipalities (Peja, Prishtina, Mitrovica, Vushtri, Prizren, Ferizaj, Gjakova and Gjilan) in Kosovo who works in three levels of healthcare facilities (primary, secondary and tertiary). In Kosovo, there were 13518 healthcare workers working in the public sector. A sample size calculation based on an error margin of 5%, a 95% confidence level, and a response distribution of 50% were performed for this study at the sample size calculator website: http://www.raosoft.com/samplesize.html, and the result was 374. The study protocol was approved by the institutional review board of Heimerer College. The survey was distributed in person, each participant got a print version of the survey. All participants provided written informed consent before enrolment. Participation in the study was on a voluntary basis. Since it was a random sampling, every participant had an equal probability to be part of the study.
2.1. Procedures and Data Analysis
The procedures of this study complied fully with the provisions of the Helsinki Declaration on research on human participants. Data were collected through a structured, anonymous, self-directed questionnaire, including socio-demographic characteristics, and the Evidence-Based Practice (EBP). We have used the Evidence-Based Practice (EBP) questionnaire developed by Upton and Upton [22] to collect the data in this survey. The questionnaire consists of socio-demographic information: age, gender, education, income status, marital status, living setting, profession and work experience. The questionnaire consists of practice (the use of EBP), knowledge’ skills and attitudes. After piloting, the internal consistency of the questionnaire has been established for three dimensions of the questionnaire: use of EBP (Cronbach’s Alpha 0.679), attitudes toward EBP (Cronbach’s Alpha 0.212), and knowledge of EBP (Cronbach’s Alpha 0.911). The scale consists of 24 items with three sub-dimensions. EBP knowledge consists of 14 items, followed by use of EBP with 6 items and attitudes with 4 items and using Likert scale of 1 to 7 measuring the level of agreement-disagreement. Since the questionnaire was originally written in English, an identical version of the questionnaire was translated into Albanian, using the double-forward-backward method [42].
The Statistical Package for the Social Sciences software (SPSS version 21.0) was used for data analysis [43]. Frequencies (n) and percentages (%) were used to summarise categorical variables, and continuous variables are summarised with mean±standard deviation (SD). The distribution of normality was evaluated using Kolmogorov-Smirnov tests, while the independent samples t-test, one-way ANOVA and post-hoc Tukey test and linear regression were used to analyze variables. For all statistical tests, a p-value of <0.05 was considered statistically significant.
3. RESULTS
Sixty-five percent (65%) of the participants were female. The mean age of participants was 38 years. One-fifth of the participants in the study sample received a secondary school education, and the majority were married with an economic status equivalent to the middle class and living in an urban setting. Two third of the participants were nurse and majority were working in primary health care facilities. 78% of participants were working in the public health facilities, and 16% had a managerial role (Table 1).
| - |
Total N (%) or Mean±SD |
Medical Doctor N (%) or Mean±SD |
Nurse N (%) or Mean±SD |
Other Health Professionals N (%) or Mean±SD |
|---|---|---|---|---|
|
Gender Male Female |
213 (34.9) 398 (65.1) |
79(49.4) 81(50.6) |
114(28.1) 291(71.9) |
20(43.5) 26(56.5) |
| Age (years) | 38.8±12.1 | 430±11.6 | 37.5±12.1 | 35.6±10.3 |
|
Education Secondary school Bachelor degree Master Degree PhD degree Specialization |
123(20.1) 250(40.9) 130(21.3) 35 (5.7) 73 (11.9) |
-- -- 69(43.1) 33(20.6) 58(36.3) |
108(26.7) 211(52.1) 85(21.0) 1(0.2) -- |
9(19.6) 16(34.8) 20(43.5) 1(2.2) -- |
|
Income Low Medium High |
162(26.5) 425(69.6) 24(3.9) |
3(1.9) 89(55.6) 68(42.5) |
19(4.7) 305(75.3) 81(20.0) |
2(4.3) 31(67.4) 13(28.3) |
|
Marital Status Single Married Widowed |
182(29.8) 390(63.8) 39(6.4) |
37(23.1) 108(67.5) 15(9.4) |
127(31.4) 257(63.5) 21(5.2) |
18(39.1) 25(54.3) 3(6.5) |
|
Living Setting Urban Rural |
423(69.2) 188(30.8) |
106(66.3) 54(33.8) |
281(69.4) 124(30.6) |
36(78.3) 10(21.7) |
|
Level of Heath Service Facility Primary Secondary Tertiary |
361(59.1) 181(29.7) 69(11.3) |
100(62.5) 38(23.8) 22(13.8) |
241(59.5) 121(29.9) 43(10.6) |
20(43.5) 22(47.8) 4(8.7) |
|
Working Health Sector Public facility Private facility |
479(78.4) 132(21.6) |
131(81.9) 29(18.1) |
330(71.5) 75(18.5) |
18(39.1) 28(60.9) |
|
Having Managerial Role Yes No |
103(16.9) 508(83.1) |
34(21.2) 126(78.8) |
58(14.3) 347(85.7) |
11(23.9) 35(76.1) |
| Work Experience (Years) | 12.0±10.5 | 13.3±9.7 | 11.8±10.9 | 9.2±7.4 |
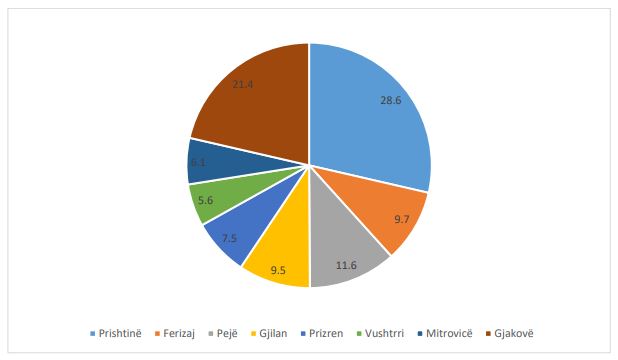
Fig. (1) shows the participants’ distribution by the municipality. The majority of respondents were from Prishtina (28.6%) followed by Gjakova with (21.4%) and Ferizaj (9.7%)
| - | Total | Medical Doctor | Nurse | Others | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | |||||||
| Use of EBP | Gender | Female | 2.13±0.62 | t=-0.883, p=0.378 | 1.99±0.57 | t=-0.829, p=0.408 | 2.18±0.64 | t=-1.496, p=0.219 | 2.07±0.39 | t=-0.230, p=0.844 |
| Male | 2.18±0.71 | 2.08±0.69 | 2.27±0.77 | 2.10±0.36 | ||||||
| Living Setting | Urban | 2.16±0.65 | t=0.539, p=0.590 | 1.99±0.64 | t=-1.218, p=0.225 | 2.23±0.67 | t=1.312, p=0.190 | 2.09±0.34 | t=0.021, p=0.984 | |
| Rural | 2.13±0.66 | 2.12±0.61 | 2.14±0.70 | 2.08±0.48 | ||||||
| Working Health Sector | Public | 2.14±0.66 | t=-0.803, p=0.422 | 2.04±0.67 | t=0.169, p=0.866 | 2.16±0.66 | t=-2.085, p=0.038 | 2.25±0.40 | t=2.524, p=0.015 | |
| Private | 2.19±0.62 | 2.02±0.45 | 2.34±0.71 | 1.98±0.32 | ||||||
| Profession | Medical doctor | 2.04±0.63 | F=4.136, p=0.016 | Na | Na | Na | ||||
| Nurse* | 2.20±0.68 | Na | Na | Na | ||||||
| Other | 2.08±0.37 | Na | Na | Na | ||||||
| Level of Health Facility | Primary | 2.09±0.68 | F=5.127, p=0.006 | 2.04±0.71 | F=0.029, p=0.971 | 2.10±0.69& | F=7.896, p<0.0001 | 2.09±0.43 | F=0.115, p=0.891 | |
| Secondary | 2.21±0.59 | 2.01±0.45 | 2.30±0.64 | 2.07±0.35 | ||||||
| Tertiary** | 2.32±0.62 | 2.03±0.53 | 2.49±0.63 | 2.17±0.00 | ||||||
| Attitudes Toward EBP | Gender | Female | 3.61±1.05 | t=0.149, p=0.882 | 3.53±1.15 | t=-0.358, p=0.721 | 3.61±1.05 | t=0.543, p=0.587 | 3.82±1.18 | t=-0.208, p=0.836 |
| Male | 3.59±1.07 | 3.59±1.14 | 3.55±1.07 | 3.88±0.73 | ||||||
| Living Setting | Urban | 3.62±1.03 | t=0.478, p=0.633 | 3.55±1.01 | t=-0.222, p=0.825 | 3.60±1.05 | t=0.218, p=0.828 | 3.95±0.81 | t=1.372, p=0.177 | |
| Rural | 3.57±1.12 | 3.59±1.14 | 3.57±1.09 | 3.47±1.50 | ||||||
| Working Health Sector | Public | 3.54±1.05 | t=-2.715, p=0.007 | 3.50±1.03 | t=-1.437, p=0.153 | 3.55±1.04 | t=-2.037, p=0.042 | 3.94±1.28 | t=0419, p=0.677 | |
| Private | 3.82±1.07 | 3.82±1.13 | 3.83±1.13 | 3.81±0.83 | ||||||
| Profession | Medical doctor | 3.56±1.05 | F=1.386, p=0.251 | Na | Na | Na | ||||
| Nurse | 3.59±1.06 | Na | Na | Na | ||||||
| Other | 3.85±1.00 | Na | Na | Na | ||||||
| Level of Health Facility | Primary*** | 3.40±1.04 | F=18.235, p<0.0001 | 3.41±1.04 | F=2.968, p=0.054 | 3.40±1.05$ | F=14.274, p<0.0001 | 3.40±0.99 | F=4.299, p=0.020 | |
| Secondary | 3.82±1.02 | 3.89±1.05 | 3.74±1.02 | 4.14±0.93§ | ||||||
| Tertiary | 4.08±0.95 | 3.67±1.03 | 4.25±0.88 | 4.50±0.58 | ||||||
| Knowledge of EBP | Gender | Female | 5.37±1.02 | t=0.951, p=0.342 | 5.35±1.15 | t=1.496, p=0.137 | 5.37±1.01 | t=-0.197, p=0.844 | 5.36±0.78 | t=-0.330, p=0.743 |
| Male | 5.28±1.08 | 5.08±1.15 | 5.39±1.05 | 5.45±0.87 | ||||||
| Living Setting | Urban | 5.40±1.02 | t=2.162, p=0.031 | 5.27±1.18 | t=0.760, p=0.448 | 5.45±0.98 | t=2.192, p=0.029 | 5.37±0.82 | t=-0.462, p=0.646 | |
| Rural | 5.20±1.08 | 5.12±1.10 | 5.21±1.08 | 5.51±0.85 | ||||||
| Working Health Sector | Public | 5.33±1.05 | t=-0.245, p=0.806 | 5.22±1.19 | t=0.137, p=0.891 | 5.38±1.00 | t=-0.202, p=0.840 | 5.35±0.83 | t=-0.207, p=0.837 | |
| Private | 5.36±1.01 | 5.19±1.00 | 5.40±1.08 | 5.40±0.82 | ||||||
| Profession | Medical doctor | 5.22±1.15 | F=1.395, p=0.249 | Na | Na | Na | ||||
| Nurse | 5.38±1.02 | Na | Na | Na | ||||||
| Other | 5.40±0.82 | Na | Na | Na | ||||||
| Level of Health Facility | Primary | 5.36±1.05 | F=0.849, p=0.428 | 5.20±1.28 | F=0.363, p=0.696 | 5.43±0.96 | F=2.932, p=0.054 | 5.35±0.80 | F=0.125, p=0.883 | |
| Secondary | 5.26±1.01 | 5.34±0.86 | 5.20±1.09 | 5.41±0.80 | ||||||
| Tertiary | 5.42±1.07 | 5.08±1.00 | 5.58±1.09 | 5.57±1.15 | ||||||
** Health workers working in tertiary health facilities had higher points on the use of EBP compared to those working in primary health care facilities in post hoc analyses (p<0.05).
*** In post hoc analyses healthcare workers working in primary health facilities had lower points on the attitudes toward EBP compared to those working in secondary and tertiary healthcare facilities (p<0.05).
$ Nurses working in primary health facilities had lower points on the attitudes toward EBP compared to those working in secondary and tertiary health care facilities in post hoc analyses (p<0.05).
§ Other health workers working in secondary health facilities had lower points on the attitudes toward EBP compared to those working in primary and tertiary health care facilities in post hoc analyses (p<0.05).
There was no statistically significant difference in the points of healthcare workers of the dimension of questionnaire regarding the use of EBP based on gender, living setting, and working health sector. In the post hoc Tukey analyses, the nurses were found to have higher points in the dimension of the use of EBP compared to medical doctors (p<0.05). Health workers working in tertiary health facilities had higher points on the use of EBP compared to those working in primary health care facilities in post hoc analyses (p<0.05) (Table 2).
There was no statistically significant difference in the points of healthcare workers of the dimension of questionnaire regarding the attitudes toward EBP based on gender, living setting, and profession. Heath workers working in private facilities showed higher points attitudes toward EBP compared to those working in public sector (p<0.05). In post hoc analyses, healthcare workers working in primary healthcare facilities had lower points on the attitudes toward EBP compared to those working in secondary and tertiary healthcare facilities (p<0.05) (Table 2).
Health workers didn’t change on the point of the dimension of questionnaire knowledge of EBP based on gender, profession, level of health facility and working health sector (p>0.05). Health workers living in urban settings had a higher point of the dimension knowledge of EBP compared to those living in the rural area (p<0.05) (Table 2).
The following predictor factors showed a statistically significant impact in the adjusted linear regression analysis for the dependent variable use of EBP: being a medical doctor (β: 0.086, 95%CI: -0.002 - 0.170, p=0.044), and working in a primary healthcare facility (β: 0.134, 95%CI: 0.066-0.201, p<0.0001); for the dependent variable attitudes toward EBP: working in primary healthcare facility (β: 0.309, 95%CI: 0.174 – 0.454, p<0.0001), and the single marital status (β: 0.346, 95%CI: 0.238-0.454, p<0.0001); for dependent variable knowledge of EBP: the low income (β: 0.277, 95%CI: 0.133 – 0.421, p<0.0001), and work experience in years (β: -0.012, 95%CI: -0.019 – -0.006, p<0.0001) (Table 3). Table 3 also shows the un-adjusted regression analysis results for the dependent variables, use of EBP, attitudes toward EBP and knowledge of EBP for the total study sample and the nurses’ professionals, separately.
4. DISCUSSION
This study employed cross-sectional study of the use of EBP, attitudes and knowledge of Healthcare professionals in Kosovo. Evidence-based practice (EBP) is an important indicator to ensure stable quality care [43]. The purpose of this study was to evaluate and understand the levels of knowledge, beliefs and skills in healthcare workers (N=611) in Kosovo.
| - | Total | Nurses | ||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted** | Unadjusted | Adjusted** | |||||
| Use of EBP | ||||||||
| - | B (95% CI) | P | B (95% CI) | P | B (95% CI) | P | B (95% CI) | P |
| Female Gender | -0.084 (-0.258-0.90) | 0.342 | -/- | - | 0.074 (-0.059- 0.207) | 0.274 | -/- | - |
| Age (years) | -0.011 (-0.017- -0.004) | 0.002 | -/- | - | 0.001 (-0.004 – 0.006) | 0.644 | -/- | - |
| Medical Doctor* | 0.118 (-0.033- 0.268) | 0.125 | 0.086 (0.002-0.170) | 0.044 | -/- | -/- | - | |
| Working in Pimary Health Facility* | -0.011 (-0.132- 0.109) | 0.854 | 0.134 (0.066-0.201) | <0.0001 | 0.197 (0.111 – 0.284) | <0.0001 | -/- | - |
| Low Income | 0.248 (0.085-0.412) | 0.003 | -/- | - | 0.024 (-0.106 – 0.154) | 0.717 | -/- | - |
| Single Marital Status* | -0.115 (-0.265- 0.34) | 0.131 | -/- | - | 0.004 9-0.106 – 0.115) | 0.939 | -/- | - |
| Work Experience (Years) | -0.009 (-0.017 - -0.001) | 0.025 | -/- | - | -0.002 (-0.008 – 0.003) | 0.411 | -/- | - |
| Attitudes Toward EBP | ||||||||
| Female Gender | -0.023 (-0.188- 0.142) | 0.786 | -/- | - | -0.052 (-0.267- 0.162) | 0.633 | -/- | - |
| Age (Years) | 0.012 (0.005-0.018) | <0.0001 | -/-- | - | 0.009 (0.001-0.017) | 0.024 | 0.010 (0.002- 0.018) | 0.010 |
| Medical Doctor* | 0.066 (-0.077- 0.210) | 0.364 | -/- | - | -/- | -/- | - | |
| Working in Primary Health Facility* | 0.343 (0.234-0.453) | <0.0001 | 0.309 (0.174-0.454) | <0.0001 | 0.394 (0.259-0.530) | <0.0001 | 0.402 (0.267- 0.536) | <0.0001 |
| Low Income* | -0.058 (-0.212- 0.97) | 0.465 | -/- | - | 0.019 (-0.184- 0.221) | 0.855 | -/- | - |
| Single Marital Status* | 0.305 (0.165-0.445) | <0.0001 | 0.346 (0.238-0.454) | <0.0001 | 0.241(0.067- 0.415) | 0.007 | -/- | - |
| Work Experience (Years) | 0.006 (-0.001 – 0.014) | 0.100 | -/- | - | 0.002 (-0.007 – 0.010) | 0.709 | -/- | - |
| Knowledge of EBP | ||||||||
| Female Gender | -0.114 (-0.268 – 0.040) | 0.145 | -/- | - | -0.015 (-0.218- 0.118) | 0.887 | -/- | - |
| Age (Years) | -0.011 (-0.017- - 0.005) | 0.001 | -/- | - | -0.007 (-0.015- 0.0001 | 0.051 | -/- | - |
| Medical Doctor* | 0.041 (-0.091- 0.174) | 0.541 | -/- | - | -/- | -/- | - | |
| Working in Primary Health Facility* | -0.037 (-0.143- 0.068) | 0.488 | -/- | - | 0.003 (-0.129- 0.135) | 0.962 | -/- | - |
| Low Income | 0.265 (0.118-0.408) | <0.0001 | 0.277 (0.133-0.421) | <0.0001 | 0.220 (0.030- 0.411) | 0.024 | -/- | - |
| Single Marital Status* | -0.160(-0.292- -0.028) | 0.017 | -/- | -0.230 (-0.395- -0.065) | 0.007 | -/- | - | |
| Work Experience (Years) | -0.012 (-0.019- -0.005) | 0.001 | -0.012 (-0.019- -0.006) | <0.0001 | -0.012 (-0.020- -0.004) | 0.003 | -/- | - |
**Only variables that had a significant effect on the model are presented
The primary findings of our study show that healthcare professionals in Kosovo have a lower point on the use of EBP points (2.15±0.65). These findings are not in line with the findings of previous studies conducted by health professionals in other countries [16, 44]. The possible explanation why these low points in the use of EBP might be the lack of institutional readiness regards using EBP [18]. Likewise, increasing the use of EBP in healthcare institutions is crucial to provide extra trainings and increasing the awareness of healthcare professionals. These findings are in line with previous studies on low practice of EBP [45-47]. Furthermore, the use of EBP in healthcare institutions needs to go simultaneously with institutional reforms [48].
The findings of our study show a lower point in attitudes toward EBP (3.60±1.06). These findings are not in line with previous studies that show high attitudes towards EBP of healthcare professionals [49, 50]. The possible explanation of these studies might be the lack of training and consistent education for a period of time to increase healthcare professionals’ attitudes towards EBP [27]. This is important due to the increase in attitudes might be a benchmark in relation to EBP [29]. Furthermore, improving the attitudes toward EBP may reflect in increasing the level of skills and knowledge of healthcare professionals [37]. Findings show the highest points on knowledge about EBP (5.34±1.04), compared to other dimensions lower points the use of EBP points and attitudes toward EBP. These findings are in line with previous studies [29].
In our study, we found that nurses’ found to have higher points on the use of EBP compared to medical doctors, and those working in tertiary healthcare facilities have higher points compared to those working in the primary healthcare facility. Nurses' higher scores in the use of EBP compared to doctors may reflect, on the one hand, their dedication to being in line with their duties and responsibilities, and, on the other, the routine practice of doctors who may not have paid enough attention to it. In terms of tertiary care, we believe that health professionals with the highest skills are employed and have the highest care for daily work, given that they are the last point of reference for patient care. Healthcare workers working in private healthcare facilities had higher points on attitudes toward EBP, and those living in urban areas had higher points on knowledge about EBP. These findings are in line with Upton and Upton [38] on differences between various professionals namely nurses and medical doctors. Furthermore, these findings contribute to the literature on the use of EBP, knowledge and attitudes at different levels of healthcare institutions. In addition, findings from the regression analyses have shown that the following predictive factors are related to a lower use of EBP: being a medical doctor and working healthcare facility level; lower attitudes toward EBP: healthcare facility level and marital status; and knowledge of EBP: income and work experience. Providing training regards to EBP may be an opportunity to influence the attitudes and as a result, increase the use of EBP. Scholars maintain that health professionals that are exposed to EBP influences positively their attitudes and health professionals become more familiar with practices and materials used in healthcare institutions [51]. Furthermore, the attitudes and the use of EBP can be enabled through various forms such as providing research infrastructure, professional trainings and adopting an organizational culture that would influence both the attitudes and use of EBP [52].
The implication of the study is as follows: Raise awareness of the importance to use EBP in the nursing field, the research can be used to build guidelines for use of EBP in Kosovo as a transition state. Also, will help nurses to provide better services in line with developed countries. However, Kosovo compared to developed and developing economies still is facing several challenges regards to institutional reforms that had negatively reflected on advancement of healthcare system development [48]. Therefore, as discussed above it is of crucial importance for policy makers to provide the needed infrastructure, training and education to develop and adopt guidelines from developed countries adopt in Kosovo by taking into the context of Kosovo.
CONCLUSION
This study aimed to provide proof regarding Evidence-Based Practice knowledge, beliefs, and skills among Kosovo healthcare practitioners. This study observed that there was no statistically significant difference in the points of healthcare workers of the dimension of questionnaire regarding the use of EBP based on gender, living setting, and working health sector. Meanwhile, the main conclusion resulted was health professionals working in tertiary health facilities had higher points on the use of EBP compared to those working in primary health care facilities in post hoc analyses.
LIMITATIONS AND FUTURE SUGGESTIONS
This study has some limitations that are addressed as future suggestions. The first limitation of this study is related to the number of respondents and the hospitals included which makes it difficult to generalize these findings within other contexts. Secondly, this study addresses only EBP but not the barriers. Hence, for the future suggestions, it is worth examining EBP and barriers to include a larger sample. Examining EBP and barriers would provide additional information to decision-makers to ensure more efficient implementation. This study also shows the importance of components of EBP for nurses and the crucial importance of providing consistent education to Nurses to provide better services to patients. Another limitation of this study was we did not include health professionals that received training in EBP standards of care before. Thereby, we recommend that future research scholars examine EBP dimensions using the sample of health professionals that have already received training in EBP standards of care.
LIST OF ABBREVIATIONS
| EBP | = Evidence based practice |
| EBPQ | = Evidence-based Practice Questionnaire |
| SPSS | = The Statistical Package for the Social Sciences software |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ad-hoc Commission on Research Ethics has reviewed the study protocol described below. Your project proposal is considered to meet the requirements of Law No. 040-135 on Scientific- Research
Activities, and ethical principles of Heimerer College, and has been given full ethical approval.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the guidelines of Helsinki, Declaration as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [B.K.H] upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


