All published articles of this journal are available on ScienceDirect.
Interventions to Reduce Patient Identification Errors in the Hospital Setting: A Systematic Review
Abstract
Background:
Patient identification is considered as a fundamental part of the care process and a relevant resource for safety practices in hospital settings.
Objective:
We aimed to review the literature on interventions to reduce patient identification errors in hospital settings.
Methods:
A systematic review of effectiveness using The Joanna Briggs Institute (JBI) methodology was conducted. A three-step search strategy was utilised to explore primary research published up to March 2020 in English, Spanish, and Portuguese across eight databases. Grey literature was also assessed. The titles and abstracts of the studies were screened for assessment of the inclusion criteria. Two reviewers independently appraised the full text of the selected studies and extracted data using standardised tools from JBI. Due to the heterogeneity of studies and insufficient data for statistical pooling, meta-analysis was not feasible. Therefore, the results were synthesised narratively.
Results:
Twelve studies met the review criteria; all were rated at a moderate risk of bias and four different groups of interventions were identified: educational staff interventions alone and those combined with a partnership with families and patients through education; and information technology interventions alone, and combined with an educational staff strategy. Although most studies showed a statistically significant reduction in patient identification errors, the overall quality of the evidence was considered very low.
Conclusion:
High-quality research is needed to understand the real impact of interventions to reduce patient identification errors. Nurses should recognise the importance of patient identification practices as a part of their overall commitment to improving patient safety.
PROSPERO Registration Number: CRD42018085236
1. INTRODUCTION
Over the past two decades, several global initiatives for patient safety have been highlighted to develop interventions for preventing and reducing hospital errors. The increased useof technology has enhanced medication administration safety, the implementation of checklists has contributed to the decline of surgical errors, and the application of safety procedures has reduced the incidence of hospital-acquired infections [1]. Proliferation in research and the notification of adverse events at a global level, combined with the use of validated measurement tools and incentives to build a consistent safety culture, have been pivotal for the advancement of safe care [2].
Although it has been 20 years since the publication of ‘To Err is Human: Building a Safer Health System’ [3], patient harm still occurs. Furthermore, many areas need improvements to reach adequate levels of safety, such as patient misidentification, Information Technology (IT), communication failures during patient transfer and handover, pressure ulcers, and falls [1].
Considerable importance should be dedicated to patient identification errors because these are the root cause of several other incidents that seriously affect health service provision [4]. Failure to identify the patient can result in poor healthcare outcomes related to the administration of medication, blood products, or diet to the wrong patient; delays in starting treatment due to incorrect identification of a blood sample or biological specimen; incorrect patient orders; mistaken surgical interventions; misidentification of new-borns; and cancellations of surgical procedures due to inaccuracies in filling out medical records, exams, and referral letters, among others [5-10].
A growing body of research has demonstrated the occurrence of these events. A literature review conducted in 181 health organisations in several countries detailed 7,613 incidents related to patient identification, including near misses and adverse events [11]. A recent report in the United Kingdom described 216 episodes of patient identification errors during blood transfusions [12]. A 10-year retrospective analysis developed in England and Wales identified 2,627 incidents associated with technology use, of which 1.1% were regarding incorrect patient identification [13]. In light of this evidence, there is an ongoing need for interventions that effectively guarantee patient identification process safety and account for the available resources and particularities of the health services using an interdisciplinary approach involving professionals and patients.
Important strategies have been instigated by the World Health Organisation (WHO) to ensure that each patient is correctly identified at all levels of care. These include the use of a minimum of two identifiers to verify the patient’s identity, for instance, the name and date of birth upon admission or transfer and prior to carrying out a treatment, procedure, or care [14]. In addition, the implementation of technological resources and tools, the incorporation of continuous training regarding patient identification protocols to health professionals as well as service users and families about the importance of correct patient identification should be mentioned [14].
Several studies have also explored similar interventions and recommended the inclusion of educational strategies and patient participation, use of reliable and standardised identifiers, implementation of comprehensive patient identification protocols with continuous monitoring, and the adoption of new technologies to enhance patient identification safety [15-19]. However, thus far, no systematic review has attempted to assess different interventions to reduce patient identification errors, and their benefits have been insufficiently recognised.
Therefore, this paper is the first to conduct such a systematic review and proposes to broaden the theme. It aims to evaluate the effectiveness of various interventions in reducing patient identification errors in both adult and paediatric hospital settings and to assess the certainty of the evidence and recommendations to enhance patient safety practices.
To facilitate the literature search, the Population, Intervention, Comparison and Outcomes Framework (PICO) was applied [20]. The problem addressed in this review included the following research question: How effective are the technological and educational interventions that may reduce patient identification errors in a hospital setting?
2. MATERIAL AND METHODS
This study was conducted under the JBI methodology for systematic reviews of effectiveness [21]. Moreover, this report was based on the Preferred Reporting Items for Systematic Review and Meta-analysis Protocols guidelines [22]. The review protocol was developed beforehand [23] and was recorded on PROSPERO under the number CRD42018085236.
2.1. Inclusion Criteria
The inclusion criteria were as follows:
- Population: This review included papers on children and adult patients of any age, race, ethnicity, or gender who were admitted to inpatient or emergency services for any condition.
- Interventions: The review examined any type of IT, such as Electronic Health Records (EHR); Computerised Physician Order Entry (CPOE); decision support systems and barcoding; and any type of educational intervention of frontline staff, patients, and families aimed at reducing the patient identification errors rate.
- Comparisons: Any comparator employed within the included studies.
- Outcomes: The primary outcome reported patient identification errors rate during a hospital stay. Moreover, surrogate outcome measures related to the patient identification process included patient Identification Bands (ID bands) errors and patient identity checks error rates. The secondary outcomes were the causes of patient identification errors and wrong-patient electronic orders rate.
- Types of studies: This review considered both experimental and quasi-experimental research designs, including non-randomised and Randomised Controlled Trials (RCTs), pre-post studies, and interrupted time-series studies. Other research designs of quantitative nature, such as observational, analytical and descriptive studies were also considered for inclusion.
2.2. Search Strategy
The search strategy aimed to locate both published and unpublished studies, and this review employed a three-step procedure. An initial limited search of Medline (NICE Healthcare Databases Advanced Search) and CINAHL (EBSCO) was undertaken, followed by an analysis of the text words in the title, abstract, and index terms used to describe the article.
A second search using all identified keywords and index terms was performed across all databases: the Cochrane Central Register of Controlled Trials, Medline, CINAHL (EBSCO), EMBASE, SCOPUS, Latin American and Caribbean Health Sciences (LILACS) and Medes. The search for unpublished studies included: ProQuest Dissertations and Theses, Google Scholar, National Health Service Improvement, Dart-Europe, System for Information on Grey Literature in Europe (Open Grey), Banco de Teses – CAPES, and Theses Canada.
Subsequently, the reference lists of all studies selected for critical appraisal were screened for additional research. All databases were searched from inception until March 2020. Moreover, studies published in the English, Portuguese, and Spanish languages were considered for inclusion to avoid language bias and missing key studies with significant findings related to the aim of this review.
A systematic approach was applied based on the research question [23], and a Medline search strategy was developed (Table 1). Individual search strategies were formulated for each database and are available in Supplementary file 1.
|
1: “Patient identification systems” [MESH] 2: (“patient identification systems” OR “patient identification system” OR “patient tracking”) [Title/Abstract] 3: (((patient ADJ2 identf*7) OR bracelet* OR wristband*) ADJ2 (error* OR integrity OR mistake*)) [Title/Abstract] 4: (patient* ADJ3 misidentfif*7) [Title/Abstract] 5: 1 OR 2 OR 3 OR 4 6: (“Inpatients” [MESH]) OR Hospitals” [MESH] 7: (((hospital OR hospitalisation OR hospitalization OR hospitals OR hospitalized OR hospitalized) 8: “Patients [MESH] 9: (patient*[Title/Abstract]) OR inpatient*[Title/Abstract] 10: 6 OR 7 OR 8 OR 9 11: 5 AND 10 Total articles found: 577 |
2.3. Selection of Studies
The search results were uploaded to EndNote TM online (Clarivate Analytics, PA, USA). Following the removal of duplicates, the relevant studies were retrieved and their citation details were imported into the JBI System for the Unified Management, Assessment and Review of Information - JBI SUMARI (JBI, Adelaide, Australia), and selected according to the eligibility criteria using a two-step process:
- The title and abstract screenings were examined by two independent reviewers for assessment of the review’s inclusion criteria. Disagreements were resolved through discussion.
- Full-text screening studies were retrieved and assessed in detail by two independent reviewers based on the inclusion criteria. Any disagreements between them were resolved through discussion or by a third reviewer.
2.4. Assessment of Methodological Quality
To ensure the quality of the analysed evidence, a cut-off point for inclusion was applied with at least 60% of the questions with affirmative answers in the JBI's critical appraisal tools [21]. Eligible studies were assessed by 2 independent reviewers, and any disagreements were resolved through discussion or by a third reviewer.
2.5. Data Extraction
Data were extracted using the standardised JBI extraction tool [21] and included specific details regarding the interventions, populations, study methods, and outcomes. Discrepancies were resolved through discussion among the reviewers. When required, the authors of primary quantitative studies were contacted for missing information or clarification of unclear data.
2.6. Data Synthesis and Assessing Certainty in the Findings
A meta-analysis was unfeasible because of the heterogeneity of the population, study design, interventions, and outcomes, as well as the insufficiency of data for statistical pooling. A summary of findings was created using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) for rating the quality of evidence [24].
2.7. Deviation from the Protocol
Patient identification errors, indicated in the protocol of this systematic review [23], were scarce and were only addressed in two studies. Therefore, the ID band errors and patient identity check error rates were analysed as substitute outcomes. Research has suggested that surrogate outcomes should be considered in the absence of relevant evidence for healthcare providers and the population [24-26]. Additionally, the wrong patient electronic orders rate was considered as the secondary outcome.
These deviations from the protocol were because these outcomes were a fundamental part of the patient identification process in the hospital setting; consequently, they were highly relevant to answer the review question and may provide decision support to improve patient safety.
3. RESULTS
3.1. Review Selection
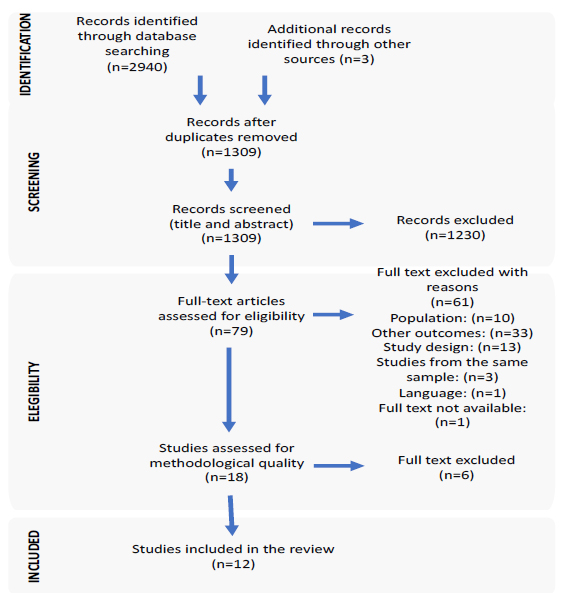
The search identified 2,943 potentially relevant studies (three articles were obtained through the reference lists of all identified reports). Of these, 1,634 were duplicate records. The remaining 1,309 records were screened by title and abstract. After examination, 1,230 studies failed to meet the inclusion criteria. The full texts of the remaining 79 records were retrieved. Subsequently, two reviewers independently reviewed each article; of these, 61 studies were excluded because they did not address a minimum of one inclusion criterion, and one article was unavailable (the list of full-text articles excluded with reasons is available in Supplementary File 2). Overall, 18 studies were appraised for methodological quality, and six were omitted. Finally, the remaining 12 records were included in the review. The flow chart presented in Fig. (1) displays the details of the search results as well as the selection process and reasons for exclusion.
3.2. Methodological Quality of the Studies
The reviewers independently assessed the methodological quality of the 18 studies. When necessary, for additional data or clarification, the authors of the papers were contacted; however, not all of them provided further information. Furthermore, 6 studies failed to reach the cut-off point for inclusion [27-32]. The list of citations and reasons for the excluded research is provided in Supplementary File 3.
Of the 12 studies included in this review, the RCT [33] scored nine out of 13 (69.2% quality score) for quality assessment with a moderate risk of bias (Table 2). The allocation of the intervention groups was not concealed, thus including potential performance bias. Due to the nature of the educational intervention, it was not possible to blind the participants and auditors. However, there was no blinding of the researchers, which may have induced a performance bias risk.
All 11 pre-post studies met at least six of nine criteria (60% quality score) with a moderate risk of bias (Table 3). Only two studies [34, 35] included a control group. However, the comparisons were made ‘within the groups only’ and reduced the possibility of exploring the consequences on the groups of exposure to different treatments in addition to the intervention of interest. In seven studies [35-41], it was unclear whether the participants were included in similar comparisons, contributing to the risk of selection bias. Additionally, in three studies [42-44], it was uncertain whether the results were derived from various measures before and after the intervention. Therefore, it was not possible to explore the changes in the ‘in time’ effect in each group and compare them between groups. Furthermore, one study [34] presented inconclusive data regarding loss of follow-up, limiting its internal validity. There was a lack of clarity with respect to whether the results were measured in a reliable way for two studies [34, 42] that may have threatened the validity of the statistical inference and its relationship between the intervention and the outcome. Lastly, one study [43] did not present conclusive details of the statistical analysis that may have caused an error in statistical inference.
| First Author year |
Critical Appraisal of Randomized Controlled Study | Total (yes) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | ||
| Murphy 2007 a | Y | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 9 |
Yes (Y), No (N)
Q1. Was true randomization used for the assignment of participants to treatment groups?
Q2. Was allocation to treatment groups concealed?
Q3. Were treatment groups similar at the baseline?
Q4. Were participants blind to treatment assignment?
Q5. Were those delivering treatment blind to treatment assignment?
Q6. Were outcomes assessors blind to treatment assignment?
Q7. Were treatment groups treated identically other than the intervention of interest?
Q8. Was follow-up complete? and if not, were differences between groups in terms of their follow-up adequately described and analysed?
Q9. Were participants analysed in the groups to which they were randomized?
Q10. Were outcomes measured in the same way for treatment groups?
Q11. Were outcomes measured in a reliable way?
Q12. Was appropriate statistical analysis used?
Q13. Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial?
|
First Author Year |
Critical Appraisal of Quasi-Experimental Studies | Total (yes) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | ||
| Adelman 2017 a | Y | Y | Y | Y | Y | U | Y | U | Y | 7 |
| Adelman 2015 b | Y | Y | Y | N | U | Y | Y | U | Y | 6 |
| Cuadrado-Cenzual 2015 c | Y | U | U | N | Y | Y | Y | Y | Y | 6 |
| Franklin 2007 d | Y | U | U | N | Y | Y | Y | Y | Y | 6 |
| Garnerin 2008 e | Y | U | Y | N | Y | Y | Y | Y | Y | 7 |
| Green 2015 f | Y | U | U | Y | Y | Y | Y | Y | Y | 7 |
| Hyman 2012 g | Y | Y | Y | N | U | Y | Y | Y | U | 6 |
| Howanitz 2002 h | Y | U | U | N | Y | Y | Y | Y | Y | 6 |
| Phillips 2012 i | Y | U | U | N | Y | Y | Y | Y | Y | 6 |
| Spain 2015 j | Y | Y | Y | N | U | Y | Y | Y | Y | 7 |
| Walley 2013 k | Y | U | U | N | Y | Y | Y | Y | Y | 6 |
Yes (Y), No (N), Unclear (U)
Q1. Is it clear in the study what is the ‘cause’ and what is the 'effect' (i.e., there is no confusion about which variable comes first)?
Q2. Were the participants included in any comparisons similar?
Q3. Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?
Q4. Was there a control group?
Q5. Were there multiple measurements of the outcome both pre and post the intervention/exposure?
Q6. Was follow-up complete? and if not, were differences between groups in terms of their follow-up adequately described and analysed?
Q7. Were the outcomes of participants included in any comparisons measured in the same way?
Q8. Were outcomes measured in a reliable way?
Q9. Was appropriate statistical analysis used?
3.3. Characteristics of the Included Studies
The 12 studies were conducted between 2002 and 2017 and included one RCT [33], two controlled pre-post-test studies [34, 35] and nine single group pre-post-test studies [36-44]. A table describing the included studies is provided in the appendix.
Overall, 11 studies were published in English [33-35, 37-44], while only one in Spanish [36]. Furthermore, eight were single-centre studies conducted in multiple countries, including the USA [34, 41-43], Spain [36], Australia [44], the United Kingdom [37] and Switzerland [38]. Moreover, four multi-centre studies were conducted in five emergency services in New York City, USA [35], one in Canada, Australia and the USA [39], one in England, the USA, Canada, Norway, Brazil, and Australia [39], and one in six hospitals across the USA [40].
Among the included studies, sample types varied between patients, ID bands, electronic orders, and medication rounds; they ranged from 282 [41] to 11,377 [40] patients. The studies conducted in adult services were as follows: two studies in inpatient wards [37, 39], two in Accident and Emergency Services - A&E [36, 44], one in Theatres [38] and one in both intensive care unit (ICU) and ward [39]. Furthermore, five studies were carried out in neonatal and paediatric settings. Of these, three were developed in both neonatal and paediatric ICUs [34, 40, 41], one in a paediatric ward [43] and one in a single paediatric ICU [42]. In addition, one study was conducted in both adult and paediatric A&Es [35].
3.4. Follow-up and Interventions
The follow-up period varied significantly between studies and ranged from less than six months [ 40, 44] to three and half years [34]. The interventions of interest examined in the studies were categorised into four major groups as described below.
Four studies included educational staff interventions [ 33, 38, 39, 41]. The RCT [33] compared a tag on blood bags educating the staff to verify the patient’s wristband and identity before transfusion against control (no addition of the tag on blood bags). One study [38] implemented a protocol to confirm patient identity with periodic audits and ‘just in time’ staff feedback after an error had been identified, discussing inadequate identification verification issues. Furthermore, supplementary training was provided at staff meetings. Two studies [39, 41] standardised ID bands, followed by audits and consequent staff feedback after each error had been identified to raise awareness about the importance of correct patient identification.
Only one study [40] combined staff education regarding correct patient identification with a partnership with families and patients through education and audited wristbands providing prompt feedback to them about the importance of identification for safe care. A complementary poster was developed to be hung in the patient’s room, reminding that the ID bands should remain on them constantly.
Five studies applied IT interventions. Franklin et al. [37] used a closed-loop system incorporating electronic prescribing, ward-based automated dispensing, and barcode patient identification to enhance patient identity check prior to medication administration. Hyman et al. [43] modified the EHR provider interface, including a verification screen (with the patient’s photograph) that requested the employees to confirm patient identity when ordering. Three studies [34, 35, 42] employed the CPOE ID re-entry function to verify patients’ identity; additionally, two of these [34, 42] also incorporated a new name convention for newborns.
Furthermore, two studies combined IT resources with an educational staff strategy. Cuadrado et al. [36] implemented the CPOE in addition to staff education, emphasising the different measures of improvement in relation to patient misidentification. Spain et al. [44] implemented two interventions: staff education alone (regarding the technology, patient identity checks, and the risks of misidentification) and combined with an armband barcoding scan.
3.5. Outcomes
The measures used for primary outcomes varied across studies and were classified as follows:
- Patient identification errors rate was addressed by two studies measuring them in the analytical request process [36] and the total number of reported patient identification errors [43].
- The ID band errors rate was emphasised by three studies reporting the percentage of wristband errors rate [39-41].
- Patient identity check errors rate in four studies was addressed by measuring the number [33] and the percentage of incorrect patient identity checks [37, 38, 44].
The secondary outcome causes of patient identification errors were not measured in any of the studies included in this review. The wrong-patient electronic orders rate was addressed in three studies [34, 35, 42].
4. REVIEW FINDINGS
The effectiveness of the interventions was categorised into four groups according to their types and effects on the primary and secondary outcomes; these are presented below.
4.1. Effectiveness of Educational Staff Interventions
Two studies measured the ID band errors rate outcome. Walley et al. [41] reported a statistically significant decrease in the rate by 4% compared to baseline (95% CI [2.5–5.5] p<.001). Similarly, Howanitz et al. [39] indicated a statistically significant decrease in the overall mean ID wristband error rate by 4.3% compared to baseline (p=.001). Despite the overall positive results, there was considerable heterogeneity among studies regarding population, sample size, and intervention delivery.
The patient identity check errors rate outcome had inconsistent results. Garnerin et al. [38] reported an increase in the full compliance of the patient identity check from 9.7% to 58.7% compared to baseline (p<.001). The results from the RCT [33] showed that the label on the blood bag failed to improve bedside patient identity check when comparing the intervention with the control group on immediate (pooled OR 1.09; 95% CI: 0.54-2.17) and long-term effects (pooled OR 0.49; 95% CI: 0.22-1.06). Meta-analysis could not be conducted due to the different types of interventions employed in the included studies.
4.2. Effectiveness of Educational Staff Interventions Combined with a Partnership with Families and Patients through Education
Only one study [40] delivered this combined intervention and had a statistically significant reduction in ID band errors rate by 77% after the interventions were compared to baseline (p=.001). Nonetheless, this study was conducted at a multi-centre site where each hospital had its own standard process to confirm patient identity, and the authors did not ensure interrater reliability.
4.3. Effectiveness of IT Interventions
Franklin et al. [37] demonstrated a statistically significant reduction of 63% in the patient identity check errors rate during medication administration compared to baseline. The authors noted that full compliance in examining patient identity was not achieved because of incorrect practices, such as the bar code’s affixation on patients’ furniture. Moreover, the study had unclear information about the inclusion of participants in any similar comparisons.
Hyman et al. [43] reported a 25% decrease (51 versus 37) in the patient identification errors rate after the intervention compared to baseline. However, the research did not provide further statistical analysis and researchers relied on voluntary reporting of recognised errors.
The following 3 studies assessed the secondary outcome of the wrong-patient electronic orders rate. Adelman et al. [42] found a statistically significant reduction of 36.3% in this rate as compared to baseline (OR 0.64; 95% CI: 0.42-0.97). Similarly, Green et al. [35] reported a statistically significant 30% and 24.8% decrease in the rate after the intervention in the short-term impact (RR=0.70; 95% CI: 0.63-0.77) and 2 years after the intervention, respectively (RR=0.76; 95% CI: 0.69-0.83). Adelman et al. [34] also indicated a statistically significant reduction in wrong-patient electronic orders. In the neonatal ICU, intervention 1 (CPOE ID re-entry function) reduced the frequency of wrong-patient orders by 48.7% (p<.001), and the combined intervention (with new name convention) yielded a 61.1% decrease from baseline (p<.001). In the non-neonatal ICU, the former and the latter had 34.1% (p<.001) and 28.4% (p<.001) reductions from baseline, respectively.
Despite Adelman et al. [34] and Green et al. [35] using control groups, the comparisons were made only ‘within groups’ resulting in the absence of a direct comparison between the control and experimental groups. Moreover, the heterogeneity presented within the studies in this group precluded meta-analysis.
4.4. Effectiveness of IT Interventions Combined with an Educational Staff Strategy
Cuadrado et al. [36] found a patient identification errors rate of 6.18 per 10,000 requests in the analytical process. The authors reported a statistically significant decrease of the patient identification errors rate, in the analytical process (when compared within the intervention periods only) from 17.4 (after combined intervention) to 6.37 (end of study) per 10,000 requests (p<.0001). No statistically significant reduction in patient identification errors was found when comparing the baseline with the intervention period, concluding that the estimates of the effect may be imprecise.
Spain et al. [44] found a statistically significant reduction in the patient identity check errors rate before blood collection compared to baseline with staff education alone: when the patient was not asked to state their name 33.2% (p<.001) and their date of birth 35.1% (p<.001); this was further augmented by combining the armband scanner: 67.4% (p<.001) and 71.4% (p<.001) reductions in blood collection when the patient’s name and the date of birth were not asked, respectively. However, the cost of education alone appeared to be low compared to the armband scanner technology. Despite the positive effects, the study had a small sample size and short follow-up time.
5. SUMMARY OF THE EVIDENCE
The overall quality of evidence for all the included studies was very low, according to the GRADE criteria [ 24 ]. The level of evidence was downgraded due to limitations in study designs, imprecision (studies with small sample size), and inconsistency because of evident heterogeneity across populations, interventions, and indirectness (Table 4).
6. DISCUSSION
This review included 12 studies and aimed to determine the effectiveness of staff and patient education interventions and implementation of IT measures to reduce patient identification errors, ID band errors, patient identity check errors, and incorrect patient electronic orders in a hospital setting.
The significant heterogeneity in study methods, interventions, and outcomes measures precluded a meta-analysis. Moreover, synthesising the results across the available research included in this review was challenging. Due to the limited number of RCTs and problems inherent with lower-quality designs, the overall effect of educational and IT interventions on reported outcomes was found to be uncertain; hence, additional rigorous studies are needed.
It is also essential to stress the lack of findings related to the causes of patient identification errors. The investigation of this outcome attempted to identify the causal factors of the root cause of patient identification errors that can contribute to the management and prevention of adverse events [45].
6.1. Effectiveness of the Interventions
The results of this review demonstrated that educational interventions, using audit and feedback to improve accountability and raise awareness about the importance of correct patient identification, may lead to a small, but significant, decrease in the ID band errors rate [39, 41] and a larger reduction of the patient identity check errors rate [38]. However, both outcomes had limited results due to the small number of high-quality studies. The use of a reminder to educate the staff about the importance of patient identification before blood transfusion was ineffective in reducing the rate of patient identity check errors [33]. This finding is similar to another review [11], which reported that the reminders could simply increase the amount of information during the delivery of care where there is a lacking on account of professionals.
| Outcomes | Impact | Number of Studies | Certainty of Evidence (GRADE) | Comments |
|---|---|---|---|---|
| Educational staff interventions | ||||
| Patient ID band errors rate | Significant impact reported in two studies | 2 pre-post-test studies |
 VERY LOW |
Lack of control group in one study. Heterogeneity: different populations and interventions |
| Patient identity check errors rate | Significant impact reported in one study | 1 RCT and 1 pre-post-test study |
 VERY LOW |
RCT with true randomization, lack of allocation concealment and blinding and small sample size. Lack of control group in one study. Heterogeneity: different interventions |
| Educational staff intervention combined with a partnership with families and patients through education | ||||
| Patient ID band errors rate | Significant impact reported | 1 pre-post-test study |
 VERY LOW |
Lack of control group, unclear inclusion of participants in any similar comparisons |
| IT interventions | ||||
| Patient identity check errors rate | Significant impact reported | 1 pre-post-test study |
 VERY LOW |
Lack of control group, unclear inclusion of participants in any similar comparisons |
| Patient identification errors rate | Evidence is insufficient to determine impact | 1 pre-post-test study |
 VERY LOW |
Lack of control group, estimates of effects are not precise |
| Wrong patient electronic orders rate | Significant impact reported | 3 pre-post-test studies |
 VERY LOW |
Lack of control group in one study. Two studies with control group, however the comparisons were made within groups only. Heterogeneity: different populations |
| IT interventions combined with an educational staff strategy | ||||
| Patient identification errors rate | Some significant impact reported | 1 pre-post-test study |
 VERY LOW |
Lack of control group, selective outcome reporting |
| Patient identity check errors rate | Significant impact reported | 1 pre-post-test study |
 VERY LOW |
Lack of control group, small sample size and short follow-up time |
| Causes of patient identification errors | - | - | - | - |
High certainty: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate certainty: We are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low certainty: Our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect.
Very low certainty: We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
The ID band errors rate had a significantly higher reduction when audit and feedback interventions were combined with a partnership with families and patients through education. However, this evidence was limited to only a single group pre-post study [40]. Despite the increasing awareness of the demand for patient-centered strategies to improve the safety of healthcare delivery, additional studies are required to develop a complete picture of the impact of service users’ engagement on the patient identification process. Moreover, healthcare leaders need to facilitate a collaborative approach between the recipients of care and staff to enable relevant and effective patient participation [46-48].
As highlighted in a previous report [1], IT is an essential resource for improving quality. However, in this review, the evidence was insufficient to support decision-making regarding the use of IT interventions, and its effectiveness was based on the results of five pre-post studies. Overall, these studies reported that the CPOE framework might lead to a significant reduction in the wrong-patient electronic orders rate [34, 35, 42]. However, patients’ photographs in the EHR had insufficient evidence to determine the effect on the patient identification errors rate [43]. Nevertheless, it may be considered a good tool to measure near misses and to assist in preventing adverse events. Electronic prescribing, automated dispensing, and barcode technology can reduce the rate of patient identity check errors [37]. These findings support other reviews that suggest these technologies can have positive benefits on patient safety outcomes [49-51]; however, there is limited evidence regarding this [52].
The effectiveness of health-related IT interventions combined with an educational staff strategy has been described in two pre-post studies. Overall, they reported a significant reduction in the patient identification errors rate [36] and a significant reduction in the patient identity check errors rate (44). These results are also in accord with other reviews in which educational strategies have been found to enhance nurses’ adherence to patient safety attitudes and assist in the proper use of IT in hospitals [53, 54]. It is worth noting that education alone was more cost-effective than combined with an armband scanner to reduce the rate of patient identity check errors. Hospital managers should weigh the potential benefits of these technologies against possible challenges with their implementation and costs [55].
This review provided some evidence for the use of staff and patient education and IT interventions in reducing patient identification errors as well as the rates of ID band errors, patient identity check errors, and wrong-patient electronic orders in the hospital setting. However, it is also worth considering that all the included studies had methodological limitations and delivered many interventions to different populations and contexts. Consequently, the findings denote a lack of a valid effect, making it difficult to ascertain which interventions were the most effective.
7. LIMITATIONS
To our knowledge, this is the first systematic review to synthesise evidence on the effectiveness of interventions to reduce patient identification errors. Nevertheless, it has several limitations.
Most studies were conducted in North America, Europe, and Australia in tertiary and university hospitals, and some in specialised units. These results may impact the generalizability of the findings. The studies showed significant heterogeneity in methodology, population, interventions, and outcomes; therefore, these differences restricted the ability to combine studies in a meta-analysis. Moreover, these limitations did not allow the calculation of standardised effect sizes. Furthermore, there was a protocol deviation to the primary outcome which involved including surrogate outcomes related to patient identification errors that might influence the quality of the evidence due to indirectness.
The studies were found to vary in terms of reporting. The only RCT research had a small sample size and failed to conceal the group allocation. For most of the studies, the pre-post design without a control group weakened the validity of causal inferences. Regarding the two pre-post design studies with control groups, the comparisons were made only within the groups resulting in the absence of a direct comparison between the control and experimental groups, suggesting that the former was not truly comparable. Thus, the interventions may have had an apparent effect that may not be real. The authors of studies that presented inconclusive answers to the questions of JBI’s critical assessment tools were contacted; in the great majority, no response was received, which limited a more accurate analysis of the risk of bias.
Despite the aforementioned limitations, this review contributes to the current knowledge of patient identification practices to improve patient safety in hospital settings.
CONCLUSION
Patient identification interventions are recommended by the WHO [ 14 ] and are implemented worldwide, with the potential to reduce patient identification errors in hospital settings. Although evidence for these interventions remains incomplete, primarily due to methodological limitations, imprecision, inconsistency, and indirectness of the studies included in this review. Therefore, according to the GRADE criteria, the overall certainty of the evidence was considered very low.
Future high-quality research is recommended to examine IT systems, barcodes, and staff education with increasing participation of service users in mitigating patient identification errors that result in severe losses and unnecessary costs in healthcare.
RECOMMENDATIONS FOR PRACTICE
This systematic review had level B evidence based on the JBI Grades of Recommendation [56], indicating that the recommendations are ‘weak’. Innovative educational strategies are paramount to enhance professionals’ consideration of patient identification as an initial and essential part of safe care. Moreover, these interventions need to involve patients and family members to increase the awareness of their importance in the patient identification process to guarantee safe practices.
Hospital managers should implement transparent processes and comprehensive identification protocols from patient admission to discharge, involving all staff responsible for direct or indirect patient care and implementing ID wristbands with standardised identifiers. Furthermore, leaders must provide tested and validated IT resources based on the organisation’s needs and priorities that strengthen patient identification safety, such as barcode readers and secure computer systems for ordering and documenting. Finally, the interdisciplinary team must recognise the importance of incident reporting of ID errors as a part of its overall commitment to improving patient safety culture.
RECOMMENDATIONS FOR RESEARCH
First, regarding future research, larger and more robust primary studies with quality designs are required to refute or confirm and consolidate the findings of this review. Second, further studies need to be conducted to investigate the effectiveness of interventions to reduce patient identification errors in different hospitals’ levels of complexity and diverse socioeconomic contexts. Developing countries should examine and extensively address patient safety issues in their health contexts to encourage those involved in decision-making to prioritise this topic [ 57 ].
Third, additional research is required to understand the effectiveness of staff educational strategies to improve professional practices and their applicability in different hospital settings that welcome patients and families as partners in care to enhance patient safety. Similarly, additional research is necessary to evaluate IT-related safety and its cost-effectiveness, and to allow healthcare organisations to invest in technologies that consider evidence-based decisions to reduce patient identification errors. Lastly, qualitative research exploring patients’ and healthcare staff’s perceptions of patient identification safety to prevent and reduce patient identification errors would further support this review’s findings.
LIST OF ABBREVIATIONS
| A&E | = = Accident and Emergency |
| CINAHL | = Cumulative Index to Nursing and Allied Health Literature |
| CPOE | = Computerised Physician Order Entry |
| GRADE | = The Grading of Recommendations Assessment, Development and Evaluation |
| EHR | = Electronic Health Records |
| IT | = Information Technology |
| LILACS | = Latin American and Caribbean Health Sciences |
| PROSPERO | = International Prospective of Systematic Reviews |
| JBI | = The Joanna Briggs Institute |
| JBI SUMARI | = JBI System for the Unified Management, Assessment and Review of Information |
| PICO | = Population, Intervention, Comparison and Outcomes Framework |
| PRISMA-P | = Preferred Reporting Items for Systematic Review and Meta-analysis Protocols |
| RCT | = Randomized Controlled Trial |
| WHO | = World Health Organisation |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publishers web site along with the published article.
APPENDIX
|
First Author Date |
Methods Follow-up |
Participants/setting | Intervention | Outcomes |
|---|---|---|---|---|
| Educational staff interventions | ||||
| Murphy (2007) | RCT | A total of 724 direct observational audits were performed. Pre intervention: n=258 Post intervention short term n=242 Post intervention long term: n=224/ 15 matched-paired clinical areas at 12 hospitals in England, United States, Canada, Norway, Brazil and Australia. |
The authors compared a label on blood bags reminding staff to check the patient’s wristband and identity Control: no addition of the label on blood bags |
No effect of the intervention on patient identity check errors rates in the immediate effect compared to control; pooled OR, 1.09, [95% CI: 0.54-2.17] as well as long term effect; pooled OR 0.49 [95% CI: 0.22-1.06] |
| Garnerin (2008) | Single group pre-post study | A total of 1,000 interactions between patients and their anaesthetic nurse were audited/ University Hospital in Geneva, Switzerland |
The authors developed 2 verification protocols: to verify patient identity and the surgery site, plus educational intervention explaining the protocol and discussing the issues of inadequate verification within the professionals involved. Additional training was provided at staff and institutional meetings and in departmental newsletters. | Full compliance with the patient identity check protocol increased from 9.7% in the 4th quarter of 2003 (n=13/134), [95% CI: 5.3–16.0], to 58.7% in the 4th follow up period (n=121/206) [95% CI: 51.7–65.5; p<.001] |
| Howanitz (2002) | Single group pre-post study | A total of 1,757,730 wristbands were audited in inpatient services/ 217 hospitals in USA, Canada and Australia. |
Phlebotomists audited ID bands before collecting blood samples. ID band errors were recorded and the data were analysed, monthly. Professionals received summary reports of results each quarter and an annual summary report and suggestions for improvement written by the authors | Overall mean of patient ID band error rates decreased from 7.40% (first quarter) to 3.05% (eighth quarter) (p=.001). |
| Walley (2013) | Single group pre-post study | A total of 4,556 patients were audited/ 13 inpatient units and Paediatric and Neonatal Intensive Care Units, USA |
The authors standardized labels and styles on patient identification wristbands, followed by audits and feedback to the nursing staff after each error has been identified. An additional intervention of education on ID band placement policy on admission and education of standardized ID bands and labels to nursing staff, was also applied. | Patient ID band errors rates decreased from 9.2% at baseline to 5.2% post-intervention (p<.001) |
| Staff education regarding correct patient identification combined with a partnership with families and patients through education | ||||
| Phillips (2012) | Single group pre-post study | A total of 11,377 patients were audited/ Paediatric A&E, medical-surgical wards, Paediatric ICUI and Neonatal ICU (NICU), at 6 paediatric hospitals in USA. |
Audits of ID bands and each failure was an opportunity to provide just in time education to the staff, family, and patient about the importance of ID bands. Complimentarily, a poster was developed to be given to families or hung on the wall in the patient’s room about why ID bands should remain on the patient at all times. | Patient ID band error rates reduction of 77% over the 13 months of the initiative (p=.001). |
| IT interventions | ||||
| Adelman (2017) | Pre-post study with the control group. | NICU Baseline (n=2,832) Intervention 1 (n=1,493) Intervention 2 (n=2,186) Paediatric Units (non-NICU) Baseline (n=24,340) Intervention 1 (n=11,248) Intervention 2 (n=15,476)/ Level 3 Paediatric Hospital, USA |
Intervention 1 (used in all patients) was the wrong Patient Retract and Reorder – RAR ID re-entry (a validated computerized method for identifying wrong patient electronic orders The intervention 2 (newborns only) was the RAR ID re-entry combined with a distinct naming convention (incorporation of mother’s first name into the new-born’s temporary first name, e.g., Wendysgirl). Control: non-NICU |
Wrong patient electronic orders reduced by 48.7% (p<.001) in NICU. The combined intervention had a decrease of 61.1% from baseline (p<.001); In non-NICU, wrong patient electronic orders had a 34.1% reduction (p<.001). The combined intervention had a 28.4% decrease from baseline (p<.001) |
| Adelman (2015) | Single group pre-post study | Pre-intervention period: 157,857 orders placed for 1,115 neonates. Post-intervention: 142,437 orders placed for 1,067 neonates/ NICU at a Paediatric Hospital, in New York, USA. |
The authors incorporated the mother’s first name into the newborn’s temporary first name (e.g. Wendysgirl) to provide an additional level of distinction normally rendered by a unique first name. | The wrong patient electronic orders rate decreased by 36.3% after the intervention; OR 0.64 95% [CI: 0.42–0.97] |
| Franklin (2007) | Single group pre-post study | A total of 111 medication rounds were audited on a 28 adult bed ward/ University hospital, United Kingdom | A closed-loop system incorporating electronic prescribing, ward-based automated dispensing, barcode patient identification and electronic medication administration error, followed by drug rounds audit | Patient identity check error rates for medications administration decreased from 82.6% pre-intervention to 18.9% doses after the intervention (p=.001); a decrease of 63.7% [95% CI: 60.8-66.6]. |
| Green (2015) | Pre-post study with the control group | A total of 3,457,342 electronic orders were audited/ Five A&Es (two adults, two paediatrics, and one combined in USA) |
The authors developed a CPOE. A patient verification dialog box appeared at the beginning of each ordering session, requiring professionals to confirm the patient's identity. Control: inpatient areas where the verification module was not active |
Wrong patient electronic orders reduced by 30% on short-term impact RR=0.70, [95% CI: 0.63–0.77]. In the long-term analysis, a 24.8% decline was observed in wrong patient orders RR=0.76, [95%CI: 0.69–0.83]. |
| Hyman (2012) | Single group pre-post study | The sample size was not stated/ Paediatric inpatient areas on a Children’s hospital in Colorado, USA. |
The authors modified the electronic medical records/provider interface including a verification screen (with patients photograph) that requested the employees to confirm patient identity when ordering | At baseline, the number of patient identification errors was 51. After intervention, the total number of reported patient identification error rates decreased by 25% to 37. |
| IT interventions combined with an educational staff strategy | ||||
| Cuadrado (2015) | Single group pre-post study | A total of 483,254 blood requests were audited/ A&E at a large Hospital in Madrid, Spain. | The authors implemented an electronic request in ED, as a technological resource. An additional intervention of education of personnel involved in the process of obtaining samples related to the electronic request emphasizing the different measures of improvement in relation to patient and blood samples misidentification was also applied. | At baseline, the rate of patient identification errors in the analytical request process was 6.18 per 10,000. In the second semester of 2012: 17.4 per 10,000 analytical requests. From the first semester of 2013 was observed a statistically significant decrease of errors with 6.37 patient identification errors per 10,000 requests, compared to the second semester of 2012 (p<.0001) |
| Spain (2015) | Single group pre-post study | A total of 282 patients were audited during pathology collection. Pre-intervention (arm 1): n=115 Post-intervention: -education only (arm 2): n=95 education+ wristbands scan (arm 3): n =72/ Public regional ED in Australia |
The authors compared two interventions (education alone and education plus armband scanner) to measure Key Behaviours (KB) for an incorrect patient identity check, on the patient identification process at baseline and post-implementation periods. | There was a statistically significant improvement between Arms 1, 2 and 3 for Patient identity check error rates. Armband checked before taking a sample (yes): Arm 1: 11.3% (p<.001) Arm 2: 33.7% (p<.001) Arm 3: 58.0% (p=.004) Patient asked to state name (no): Arm 1: 73.2% (p<.001). Arm 2: 40% (p<.001). Arm 3: 5.8% (p<.001) Patient asked to state date of birth (no): Arm 1:77.2% (p<.001). Arm 2: 42.1%(p<.001). Arm 3: 5.8% p<.001) |


