SYSTEMATIC REVIEW
Barriers to and Opportunities for Male Partner Involvement in Antenatal Care in Efforts to Eliminate Mother-to-child Transmission of Human Immunodeficiency Virus in Kenya: Systematic Review
Brian Barasa Masaba1, *, Rose M Mmusi-Phetoe1
Article Information
Identifiers and Pagination:
Year: 2020Volume: 14
First Page: 232
Last Page: 239
Publisher ID: TONURSJ-14-232
DOI: 10.2174/1874434602014010232
Article History:
Received Date: 8/05/2020Revision Received Date: 20/09/2020
Acceptance Date: 22/09/2020
Electronic publication date: 20/11/2020
Collection year: 2020

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
Men’s involvement in antenatal care (ANC) is intended to encourage husbands to support women’s care and associated interventions, including prevention of mother-to-child transmission from pregnancy to delivery, and throughout the postnatal period. The present study aimed to systematically review the barriers and opportunities for male partner involvement in antenatal care in efforts to eliminate mother-to-child transmission of Human Immunodeficiency virus (HIV) in Kenya.
Methods:
A systematic search of articles was from the following databases; Scopus, Science Direct, PUBMED, OVID, and Google scholar. The reference list of included studies was manually searched for possible additional eligible articles. The searches were conducted from May 2019 to April 2020. Qualitative analysis was done and data were presented in thematic domains.
Results:
The search generated 2208 articles, of which only 19 met the inclusion criteria. The major findings were discussed under two thematic domains: 1) Barriers: Knowledge, Social-cultural/economic factors, Institutional factors, and Age. 2) Opportunities: Skilled Birth Attendant, Human Immunodeficiency virus-free infant and Human Immunodeficiency virus testing.
Conclusion:
The review notes that the main barriers to male partner involvement in antenatal care in efforts to eliminate mother-to-child transmission of Human Immunodeficiency virus in Kenya include; socio-cultural factors, the low maternal-child health education by the male partner, and institutional factors. It further provides insight on the opportunities associated with male partner involvement in antenatal care/prevention of mother-to-child transmission, which includes; having Human Immunodeficiency virus-free infants and increased, skilled birth deliveries. The review strongly calls out for sustainable initiatives to incorporate males into the antenatal care/prevention of mother to child transmission programs.
1. INTRODUCTION
In 2016, the WHO recommended a minimum of eight Antenatal-Care (ANC) contacts, a move from the previous four contacts [1]. The increased ANC contacts were associated with better maternal and child health outcomes [1]. One of the major services offered to pregnant mothers during these contacts is the HIV interventions, using ANC as a common platform [1]. The elimination of mother-to-child transmission (EMTCT) of HIV interventions include HIV/ syphilis counseling and testing, antiretroviral therapy (ART), condom use, infant prophylaxis, safe infant feeding, and hospital delivery [2, 3]. Previously in 2016, UNAIDS and its partners strategized that in order to end AIDS by 2030, the world was first to eliminate new HIV infections among children by 2020 [4]. This target is unlikely to be met, as, globally, in 2019, there were 160 000 infections among children aged 0-14 [5]. Nearly 90% of these infections were in sub-Sahara [5]. In Kenya, new infections among children declined from 13,500 in 2010 to 8,000 in 2017 [6]. Without treatment, if a pregnant woman is living with HIV, the likelihood of the virus passing from mother-to-child is 15% to 45% [6]. However, antiretroviral treatment (ART) and other interventions can reduce this risk to below 5% [6].
Pregnancy presents a window of opportunity to identify HIV infection and engage women and their partners in HIV treatment for their own health and the health of their future children [7]. It can aid in the identification of sero-discordant couples [8]. Additionally, it is associated with improved uptake of effective interventions such as ART drug adherence for the infected, leading to infant HIV-free survival [8, 9]. Walcott et al. noted that without partner support, it is often difficult for women to adhere to recommended HIV treatment and breastfeeding regimen needed to reduce the infection risk of their child [10]. This is because of the men’s economic dominance and decision-making power in the family [11]. Findings from Malawi showed that women with male partner involvement were more likely to have infants who tested HIV negative than those without male partner involvement [12]. In support of this, lower (2.3%) seropositive was noted in the group of infants born to mothers with male ANC attendance, compared to (8.7%) for those born to mothers lacking partner participation in Kenya [13].
Men’s involvement in ANC is also intended to encourage husbands to support women’s care and associated interventions from pregnancy to delivery and throughout the postnatal period [14]. Recently, in an Ethiopian study, researchers demonstrated significant associations between male partners’ involvement in maternal health care and the utilization of some maternal health care services by female partners [15]. In Malawi, women with male partner involvement were more likely to use condoms, deliver at the hospital, and complete the follow-up in the program, compared to those without male partner involvement [12].
Accordingly, male involvement in ANC can mean different strategies from education and awareness creation to actual participation [16]. In the literature, there is no standard definition of male partner involvement in the PMTCT of HIV [3]. However, Weiss et al. argued that male ANC involvement must be more than just “presence” at the maternal health clinic [17]. It must also include active participation in a program that provides them both information and opportunity for exploration of those factors relevant to both maternal and infant well-being, which include PMTCT [17].
Despite the mentioned benefits associated with ANC male partner involvement, the uptake of the initiative is low in Kenya [18, 19]. Correspondingly, in a study conducted in Malawi, the rate of male partner involvement in PMTCT was noted at 3.2% [12]. Similarly, in Ghana, a study on barriers to and opportunities for men’s involvement in maternal healthcare noted that less than a quarter of male participants had ever accompanied their wives for antenatal care or postnatal care in a health facility [19]. Due to low male partner testing, the HIV status of male partners is often not known throughout the pregnancy and postpartum period [9].
It is, therefore, imperative as the world gears towards increasing male partner involvement in ANC/PMTCT; it pays attention to the barriers and opportunities of the initiative. This will make the available evidence provide guidance to the male partner involvement in ANC/PMTCT initiatives.
1.1. Objectives and Review Questions
The present study aimed to systematically review the barriers to and opportunities for male partner involvement in ANC, in efforts to eliminate mother-to-child transmission of HIV in Kenya. The adopted question for this study was what are the barriers to and opportunities for male partner involvement in ANC in efforts to eliminate mother-to-child transmission of HIV in Kenya?
2. METHODS
Guidelines for preferred reporting items for systematic reviews (PRISMA) were utilized [20].
2.1. Inclusion and Exclusion Criteria
An article was included if it met the following criteria: 1) Conducted in Kenya, between 2012 and 2019, 2) had study participants as the women or men seeking ANC/PMTC and related maternal-child health services, 3) published in English, 4) no limitation to the type of study designs previously utilized was made. For the present study, the PMTC services were along a broad spectrum from pregnancy to delivery and throughout the postnatal period. Conference abstracts were excluded.
2.2. Data Sources and Search Strategies
A systematic search of articles was from the following databases; Scopus, Science Direct, PUBMED, OVID, and Google scholar (Fig. 1). The following were the keywords used in the search: “opportunities,” “male partner,” involvement in ANC,” “barriers,” “male partner involvement in ANC,” “Kenya” and “opportunities,” “barriers,” “male partner involvement,” “PMTCT”. The reference list of included studies was manually searched for possible additional eligible articles. The searches were conducted from May 2019 to April 2020. In particular, the researchers used the following search terms in the PUBMED database; “barriers,” “male partner involvement,” “ANC/PMTCT” “Opportunities,” “male partner involvement” “ANC/PMTCT” AND “Kenya”.
2.3. Selection of Studies for Inclusion in the Review
Titles and abstracts of studies retrieved from each database search were stored in Mendeley Research Manager. Two review authors (BBM and RM) independently reviewed the titles and abstracts of all studies in the initial screening phase. Disagreements were solved by discussion. The same steps were taken for full-text screening of the results.
2.4. Data Extraction and Management
Using a standardized data extraction form, two review authors (BBM and RM) independently extracted data from eligible studies, including the first author’s last name, year of publication, study location, participant characteristics, study design utilized, and major findings of the study.
2.5. Quality Assessment
Two review authors (BBM & RM) independently assessed the quality of all included studies using the Critical Appraisal Skills Programme (CASP). BBM assessed the quality of the included studies while RM checked the assessed studies. Disagreements were resolved by discussion between the four review authors. No study was excluded at this point after the quality assessment.
2.6. Synthesis of Results
The qualitative analysis was approved by the technical task team, who got expert experience in systematic biomedical review. This was a secondary analysis and all identifiers of the individual participants were removed or presented using unique codes. This study adopted PRISMA (Fig. 1) reporting, as demonstrated previously by Liberati et al. [20]. Data was presented and organized under two thematic domains: 1) Barriers; Knowledge, Social-cultural/economic factors, Institutional factors, and Age. 2) Opportunities; SBA (Skilled Birth Attendant), HIV-free infant, and HIV testing.
3. RESULTS AND DISCUSSION
The search generated 2208 articles, of which 102 duplicate articles were removed. After the screening process of their titles and abstracts, only 22 articles were identified and were thereafter included in the full-text review. The identified articles were further assessed using the adopted inclusion criteria. Among 22 articles, only 19 met the inclusion criteria (Fig. 1). Table 1 gives a further summary of publication year, study design, study participants, study settings, and study results of the articles reviewed.
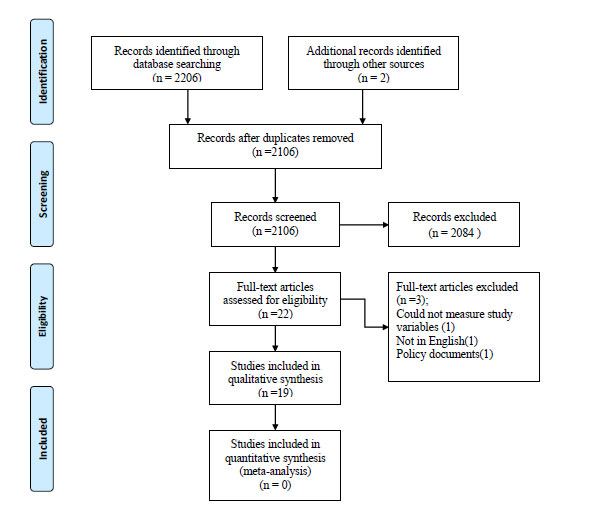 |
Fig. (1). PRISMA flow diagram. |
| Article (reference) | Year | Design | Participants | Setting | Results |
|---|---|---|---|---|---|
| (Katza et al., 2011) [21] | 2011 | Cross-sectional | 1,993 men | Nairobi | Men tested in the antenatal care setting may have a greater likelihood of disclosing HIV test results than men receiving VCT |
| (Aluisioa et al., 2012) [22] | 2012 | Prospective | 140 (31%) partners | Nairobi | The combined risk of HIV acquisition or infant mortality was lower with male attendance |
| (Oyugi et al., 2017) [8] | 2017 | Cross-sectional study | women aged ≥ 18 years who had children aged ≤ 12 months | Western Kenya | Education, having a male partner who was employed, history of previous couple testing associated with male involvement |
| (Odeny et al., 2019) [23] | 2019 | Cross-sectional survey | 2521 women attending MCH clinics | Nationwide MCH clinics | Male partner antenatal clinic attendance is associated with increased uptake of maternal health services and infant BCG immunization |
| (Nyandieka, Njeru, Ng’ang’a, Echoka, & Kombe, 2016) [11] | 2016 | Qualitative method | Study population consisted of in-charges of health facilities, reproductive health services heads, private stakeholders who provide and support maternal health services, and health facility committee members. | Malindi | Husbands are very influential in regard to decisions on skilled birth service utilization in this community. Their lack of involvement in maternal health planning may contribute to under utilization of skilled care by pregnant women. |
| (Mason et al., 2015) [24] | 2015 | Qualitative study | Using 8 focus group discussions, each consisting of 8–10 women | Western Kenya | Women perceived their husbands provided little support, either financially or in terms of help with household duties, during pregnancy and delivery. |
| (Thomson et al., 2018) [7] | 2018 | Qualitative methods | 31 focus group discussions and 35 in-depth interviews | Nairobi | Male involvement in antenatal care, and counseling customized to assist each woman in her own unique risk assessment, may improve uptake of and retention in care and optimize the HIV prevention benefit of PMTCT interventions. |
| (Gichangi et al., 2018) [18]. | 2018 | Randomized control study | 1410 women at their first ANC visit | Eastern and central Kenya | Provision of oral HIV self-tests, with a convenient, private distribution method through female partners, maybe a way to reach male partners who do not accompany ANC clients for testing at the facilities. |
| (Osoti, John-stewart, Kiarie, et al., 2015) [25] | 2015 | Cross-sectional study | 188 male partners, | Nyanza province | Pregnant women and their male partners preferred home-based tests compared to clinic or VCT-center based |
| (Mark et al., 2018) [26] | 2018 | Observational cohort study | Among 601 pregnant women | Kisumu | High acceptability of both syphilis and HIV testing among male partners of pregnant women when offered together at home in a couple testing environment. |
| (Kinuthia et al., 2018) [27] | 2018 | Cross-sectional surveys | 2522 mothers | 141 maternal and child health (MCH) clinics across Kenya from | Facilitating maternal disclosure to male partners may enhance PMTCT uptake |
| (Kwambai et al., 2013) [28] | 2013 | Cross-sectional | 68 married men | western Kenya | The three main barriers relating to cultural norms identified were: 1) pregnancy support was considered a female role; and the male role that of provider; 2) negative health care worker attitudes towards men’s participation, and 3) couple unfriendly antenatal and delivery unit infrastructure |
| (Mangeni, Mwangi, Mbugua, & Mukthar, 2013) [29] | 2013 | Kenya Demographic and Health Survey (KDHS) | 730 couples | National representative survey in Kenya. | Indicates that women whose husbands attended at least one ANC visit were more likely to have skilled birth attendance than those whose husbands did not attend any ANC visits |
| (Kamau, Chepkurui, & Chepketer, 2017) [30] | 2017 | Advocacy approach |
- | Kericho, Kenya | Male partners tend to isolate themselves when it reaches a time when a woman is in the perinatal period. |
| (Onchong, Were, & Osero, 2016) [31] | 2016 | Descriptive cross-sectional study | 207 couples | Mombasa County | The study established that most women (60.1%) and most male partners (62.3%) had poor knowledge of male partner involvement in the choice of delivery site and its benefits. |
| (Aluisio et al., 2017) | 2017 | A Prospective Cohort Study | 830 enrolled women | Nairobi | Male Partner participation in Antenatal Clinic Services is Associated with Improved HIV-free survival Among Infants in Nairobi, Kenya: |
| (Osoti, John-stewart, Richardson, et al., 2015) [32] | 2015 | A Randomized Clinical Trial | 495 women | Nyanza province, Kenya | More men were newly diagnosed as HIV positive at home and referred for HIV care. |
| (Onyango, Owoko, & Oguttu, 2010) [33]. | 2010 | Qualitative descriptive design. | Forty-two participants | 3 provinces of western Kenya: Nyanza, North Rift Valley, and Western. | Factors that influence male involvement in reproductive health emerged in two themes, namely gender norms and the traditional approaches used to implement reproductive health |
| (Nanjala & Wamalwa, 2012) [34] | 2012 | Cross-sectional study design | 380 male partners and their spouses | Busia district in Western Kenya | Lack of knowledge in male partners of complications associated with delivery, cultural beliefs, high fees charged for deliveries at health facilities and “un-cooperative” health workers are major contributing factors to low male partner involvement in child birth activities. |
The present study aimed to systematically review the barriers to and opportunities for male partner involvement in ANC in efforts to eliminate mother-to-child transmission of HIV in Kenya. The findings were presented and discussed under two thematic domains: 1) Barriers; Knowledge, Social-cultural/economic factors, Institutional factors, and Age. 2) Opportunities; SBA (Skilled Birth Attendant), HIV-free infant, and HIV testing.
3.1. Knowledge
The results of the present review demonstrate that the male partners’ knowledge of maternal-child health issues is directly proportional to the level of support of the initiative. This implies that male partners who have less knowledge about maternal health are less likely to accompany their wives at the ANC clinic. Thomson et al. study in Nairobi, Kenya, noted that how well a male partner understood the opportunities to prevent vertical transmission could have an influence on his decision to support the male involvement initiative [7]. Additionally, a study in Kisumu, Kenya, revealed that high male involvement was associated with the reports of the male partner having read the mother-child booklet during pregnancy compared to those who did not read the mother-child booklet during pregnancy [8]. Similar trends were observed in a Kenyan national cross-sectional survey [23] and a previous study in Busia, Kenya [34]. Some male participants associate the maternal-child health facilities with family planning and contraception only [33]. Implying that the male participants had a poor level of maternal health knowledge [33]. Corroborating this finding, in Uganda, knowledge about ANC services was the main independent variable associated with male attendance of ANC with their spouses, as only 47.1% of respondents (males) knew 3 - 5 services offered at ANC [35]. Recently, a similar trend was noted in Ghana, where men with a high level of knowledge on maternal health were 4 times more likely to be involved in maternal health than men with a low level of knowledge [36]. Ganle and Dery’s study in Ghana added that there is still ignorance on the part of many men about health issues, including maternal health [19]. Similarly, in a sub-Saharan Africa review [37] and rural Tanzania, lack of knowledge among male partners was also noted as a barrier for ANC involvement [38]. Health and gender programs often only target women, and men remain uneducated on relevant health issues [39]. This suggests the need for maternal health educational programs targeting males in society.
3.2. Social-cultural/Economic Factors
The present review results demonstrate that gender roles, as anchored in the social context, are a barrier to the male ANC involvement. The males in Kenyan society are brought up learning that maternal-child health issues are for women [33]. Health clinics in Kibera, Kenya, were viewed as places for women and children, especially for ante-natal and postnatal care [7]. In a western Kenyan study, ANC was seen as a ‘female’ role and, thus, the responsibility of mothers-in-law or co-wives rather than the males [28]. This makes the community easily suspicious of the male partner who gets involved in maternal health issues. Thomson et al. study in Nairobi explained that the moment male partners are seen coming with their wives to ANC/PMTCT, then the neighborhood tends to imagine that something is wrong with the couple [7]. Additionally, those who attended were mocked by their peers as having done something unusual with statements such as; “He goes to the women’s clinic” are viewed as insulting and keep the men away from reproductive health clinics [33, 34]. Similarly, Onchong et al., in Mombasa, Kenya, reported that the negative perception of male partners involved in maternal-child-health activities posed a challenge to male partner involvement [31]. Elsewhere in rural Tanzania [39] and South Africa [40], similar trends were noted as traditional gender roles were a barriers for male partner ANC involvement [38]. Suandi et al. adds that, from a social perspective, the notion of joining one’s wife at the antenatal clinic is unusual in many communities and the husband’s presence is often considered superfluous [41].
The review notes a mixed association of male ANC involvement and employment/job. For instance, in a study conducted in Kisumu, Kenya, women with employed male partners were more likely to report high male involvement [8]. Correspondingly, in Busia, Kenya, spouses of male partners with formal employment or engaged in a business were more likely to support the initiative [34]. On the other hand, for those males that are working, they perceive themselves too busy to attend the clinic [40]. Kwambai et al.s’ study in western Kenya explained that men’s focus was more on economic activities, which was more important for them to concentrate on than going to the clinic [28]. Elsewhere in Uganda, the indirect cost of transport to the health facility as long (greater than 5 km) was a prominent barrier and associated with reduced male attendance of ANC [35]. This demonstrates the indirect cost of transport was a barrier for those without income.
3.3. Institutional Factors
The main findings noted under institutional factors that were barriers to male ANC involvement included the long turn-around time, the negative attitude by the health provider, and lack of space to accommodate males. For instance, in a western Kenya study, men reported having been ignored by HCWs, subjected to an unfriendly attitude or even abusive language [28]. Similarly, in rural Tanzania, previous negative experiences in health facilities were noted as a barrier for male partner ANC involvement [38]. Onyango et al. study in Kenya noted that men do not like being kept waiting for long periods of time hence the long wait at ANC puts them off [33]. This is supported by Koo et al. study in South Africa, which observed that men had busy lives, making them impatient [40]. In Uganda, the long waiting time at the health facility was also observed as a barrier [35]. Kwambai et al. study in Kenya further noted that men would readily accompany their wives to ANC if they would be given priority in the queue before women who were unaccompanied (by a male partner) [28]. Lastly, in Ghana, limited physical space to accommodate male partners was one of the reasons why healthcare providers had difficulties incorporating male partners in the maternal-child health care initiative [19]. Similar trends were noted in a sub-Saharan Africa review [37].
3.4. Age
The review findings demonstrate mixed results on the association of the male partner’s age and ANC attendance. Some previous studies showed a younger male partner was more likely to attend the ANC while others noted contrarily. For instance, in a Kenyan national cross-sectional survey, a woman having a male partner who was younger increased the male partner’s likelihood of attending ANC [23]. Correspondingly, Onyango et al. study in western Kenya, previously explained that most married men (especially the older generation) rarely discuss reproductive health issues with their wives [33]. This implies the younger male partners are more open with their wives hence easy to get involved in maternal-child health programs. Conversely, in Kisumu, Kenya, women whose partners were aged < 24 years were less likely to experience high male involvement compared to those whose partner was aged > 24 years [8]. A study conducted in Ghana observed that male partners in the older age group (31-51 years) were more likely to get involved in maternal health issues compared to their counterparts in the younger age group (20-30 years) [36]. While Nanjala and Wamalwa’s study in Busia, Kenya, established no significant difference between the age of a male partner and the maternal-child health involvement [34].
3.5. Opportunities for HIV Testing, SBA (Skilled Birth Attendant) and HIV-free Infant
The present review provides some insight into increased hospital deliveries being associated with male partner involvement during ANC. The 3rd Prong of PMTCT advocates for delivery by skilled birth attendants in preventing HIV infection from HIV- positive pregnant women to their children [42]. A Kenyan national cross-sectional survey revealed that male partner involvement during ANC increased maternal adherence to 4 or more ANC visits and facility delivery [23]. Similarly, Mangeni et al.s’ study found that women whose husbands accompanied them to at least one ANC visit were almost twice as likely to deliver using a Skilled Birth Attendant as those who had ANC but without husband’s presence [29].
The review notes that male partner involvement supports the adherence of the 4th Prong of PMTCT. Prong 4 advocates for care, treatment, and support to women living with HIV, their children and families [42]. In Nairobi, Kenya, a Prospective Cohort Study noted that infants lacking male ANC engagement had an approximately 4-fold higher risk of death or infection compared to those born to women with partner attendance [13]. This is explained by the fact that male ANC engagement improves adherence to PMTCT feeding and treatment strategies in the family. For instance, male involvement in antenatal voluntary counseling and testing (VCT) has been associated with the increased use of antiretroviral prophylaxis in their HIV-infected pregnant partners [22]. Furthermore, improved adherence to PMTCT feeding strategies has been associated with partner support [22]. Correspondingly, in a Kenyan national cross-sectional survey among 158 HIV-infected women who had partner ANC attendance data, male ANC attendance was associated with a significantly higher prevalence of ARV use for PMTCT [23].
Finally, as mentioned before, ANC/PMTCT provides a platform for male partner HIV testing. However, some of the partners who fail to accompany their wives at ANC are unaware of their status. Findings reveal that it is not uncommon for some male partners to turn positive when provided with PMTCT services at their homes. For instance, a study in eastern and central Kenya identified 10 HIV-positive male partners when PMTCT services were rolled out in homes [18]. Similarly, in a study conducted in Nyanza Province, Kenya, it identified 1.4% of Syphilis test positivity among male partners during home PMTCT [26] Point-of-care diagnostics outside facilities can increase testing of male partners who rarely accompany women to antenatal clinics [26].
CONCLUSION
The present study adds to the current debate on male involvement in maternal child health programs. The review notes that the main barriers to male partner involvement in ANC in efforts to eliminate mother-to-child transmission of HIV in Kenya include socio-cultural factors, low maternal-child health education by the male partner, and institutional factors. It further provides insight on the opportunities associated with male partner involvement in ANC/PMTC, which include having HIV-free infants and increased skilled birth deliveries. The review strongly calls out for sustainable initiatives to incorporate males into the ANC/PMTCT programs.
LIST OF ABBREVIATIONS
| ANC | = Antenatal Care |
| ART | = Antiretroviral therapy |
| EMTCT | = Elimination of mother-to-child transmission |
| HIV | = Human Immunodeficiency virus |
| MOH | = Ministry of Health |
| PMTCT | = Prevention of Mother To Child Transmission |
| PNC | = Post Natal Care |
| SBA | = Skilled Birth Attendant |
| TBA | = Traditional Birth Attendant |
| UNICEF | = United Nations Childrens Fund |
| VCT | = Voluntary counseling and testing |
| WHO | = World Health Organisation |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors have declared that no conflicts of interest exist.
ACKNOWLEDGEMENTS
The authors declare no conflict of interest, financial or otherwise.









