Beliefs About Health, Health Risks and Health Expectations from the Perspective of People with a Psychotic Disorder
Abstract
Aim:
To examine beliefs about health, health risks and health expectations from the perspective of people diagnosed with a psychotic disorder
Background:
People with psychotic disorders have a threefold higher risk of developing physical health problems than the general population, and prevention of these problems is warranted. Examining patients´ health beliefs could help deepen our understanding of how to plan successful health interventions with this group.
Methods:
Qualitative semi-structured interviews were conducted from November 2010 to October 2011 with 17 people with psychotic disorders. Data were analyzed using a qualitative content analysis.
Results:
An overall positive picture of health was found despite the fact that physical health was found to be hard to verbalize and understand. Health was mainly associated with psychological wellbeing, while health risks were found to be related to uncertain bodily identity, troublesome thoughts and inner voices, and exclusion from society. Interest in learning, and visions and goals of health seemed to increase awareness of health risks and health expectations, while not worrying could be viewed as a hindrance for health expectations.
Conclusion:
There is a lack of expressed awareness of physical health risks, but such awareness is fundamental to performing life-style changes [14]. Nurses thus have an important task to help patients understand and verbalize potential physical health risks, and to find out what motivates them to adopt health behaviors.
INTRODUCTION
On average, people with severe mental Illness (SMI) have a shorter life-expectancy and die 8-25 years earlier than the general population [1,2] and most deaths are due to preventable medical conditions. To manage these conditions, the health care system has improved physical health care generally but there is strong evidence that this has not happened for people with SMI, who have been shown to have poorer access to physical health care than the population in general [3,4]. One explanation for this unequal treatment may be that medical health staff treat people with SMI less thoroughly and are guided by negative stereotypes [3]. Among people with SMI, those with signs and symptoms of psychosis are the most vulnerable to metabolic conditions [1,5]. Numerous factors may account for this, for example low socioeconomic situation [4], which often includes unhealthy lifestyle behaviors such as smoking, abuse of alcohol, unhealthy eating habits, and low physical activity levels [6]. To treat psychotic symptoms, psychopharmacological interventions [7] are predominant. These medications can save lives by decreasing psychiatric symptoms and suicide, but they also increase the risks of weight gain [8]. Therefore, it is necessary to perform routine screening and monitoring of glucose and hyperlipidaemia levels before and during treatments [9,10] and the potential risks and benefits of the treatment need to be considered together. However, it has been found that mental health staff are concerned about the patients becoming aware of the risks of weight gain as this is one reason for discontinuation [11]. This shows that mental health staff consider their primary aim to be to reduce psychotic symptoms and they do not have a holistic approach towards people’s health. Discussions concerning medical interventions continue to be in focus, although life expectancy in people with SMI has remained unchanged over the last 20 years, which is why there is a need to move forward with potential health promotion actions [12].
To mitigate and prevent physical health problems among people living with psychotic disorders, health promotion is essential. Health promotion is a process of enabling people to increase control over their health and its determinants, and thereby improve health [13]. One of the keystones of health promotion is the performance of health-related behaviors. According to the health belief model [14] and the health promotion model [15], variables explaining health-related behaviors are beliefs regarding health and health risk, including perceived susceptibility to illness, severity of illness, and health expectations including efficacy expectations and outcome expectations [14]. Efficacy expectations are the individual’s own judgment of a person’s capability to manage particular health behavior, and they need not reflect the actual health behavior [15]. Outcome expectations are the expected benefits to health due to a change of behavior. If a person has efficacy expectations and positive outcome expectations, this is a motivation to engage in healthy behavior. Thus, to understand a person’s level of motivation to perform health actions, we need to understand people´s beliefs regarding health, health risks and health expectations [16]. Studies concerning health beliefs among people with psychosis, focus exclusively on beliefs about mental health [17], and knowledge of health risks and health expectations among persons with psychotic disorders is limited [18]. What is known is that people with SMI have difficulty in living healthily, understanding their medical problems, remembering appointments [19], and feel a limited sense of improved, subjective well-being after completing health interventions [20]. Those with symptoms of psychosis have been shown to have many difficulties carrying out lifestyle changes [5] as psychotic symptoms can create difficulties in maintaining concentration and assimilating new information [21]. It has also been found that people with psychotic disorders have highly positive attitudes towards their physical health care even when showing higher physical health risk parameters than general population [22]. Perhaps this is a result of limited health risk beliefs? For example, people participating in a quit smoking group, pointed out professional support, the cost of cigarettes, instructions from a doctor and advice from friends as important motivators to quit smoking [23] rather than the health risks of smoking. Among people on anti-psychotic drugs, as many as 86% believed that the drugs were responsible [24] for their overweight, and in one weight loss program, barriers to weight loss were identified as difficulty changing familiar eating habits [25]. If a person places the responsibility of overweight on family and psychopharmacological interventions this affects health behavior expectations negatively, as the person might lose belief in his/her own capability to affect his/her own health, and therefore may adopt passive health behaviors. To understand a person’s level of motivation to perform health behaviors, individual beliefs concerning health, health risks and health expectations need to be further explored [16] as these variables provide motivation to engage in healthy behaviors.
Aim
To examine beliefs about health, health risks and health expectations from the perspective of people diagnosed with a psychotic disorder.
MATERIALS AND METHODOLOGY
Design
A qualitative explorative study design was selected as we were interested in understanding the participants’ own beliefs about their health, health risks, and health expectations, which have not previously been explored. Content analysis is appropriate when existing literature on a phenomenon is limited, as it allows new insights to emerge [26] and identifies people’s experiences and beliefs about the phenomenon under study.
Sampling Procedure
To catch many different voicing opinions the study was conducted in a mental health service in Sweden, both in a psychosis outpatient department at the psychiatry county hospital and in a community mental health service. The psychosis outpatient department offers adequate treatment methods which are administrated according to the Health and Medical Service Act [27] and the Compulsory Institutional Care Act [28], and involve specialized treatments. The community mental health services are responsible for meeting the needs of acceptable housing and meaningful employment of individuals with certain functional disorders [29] and support those who live in the municipality [30]. We wanted to recruit a convenience sample of people who had been diagnosed with a psychotic disorder according to the ICD 10 code numbers F20-F29 [31], and who were receiving care from one or both of the services.
First the managers of the services were contacted and given information about the study, after which they gave their written informed consent to implementation of the study. The managers informed health care staff working in their clinics, which then identified people who had been diagnosed with a psychotic disorder and who were willing to participate in the study. Those who were willing to participate gave their name and phone number, which were forwarded to the principal investigator who then contacted them to arrange a time and place for the interview. The participants chose the time and place for the interviews, eleven of which were carried out in the clinic and six in the participants’ homes (Table 1).
Characteristics of the Study Participants
| Variable | Participants (N=17) |
|---|---|
|
|
|
| Gender | |
| Male | 10 |
| Female | 7 |
|
|
|
| Age (years) | 34-66 (median 48 ) |
|
|
|
| Country of Birth | |
| Sweden | 12 |
| Iraq | 2 |
| Ethiopia | 1 |
| Bosnia | 1 |
| Syria | 1 |
|
|
|
| Antipsychotic treatment | |
| First generation antipsychotics | 5 |
| Second generation antipsychotics | 9 |
| Mixed first and second generation antipsychotics | 3 |
|
|
|
| Diagnoses | |
| Schizophrenia | 5 |
| Schizoaffective disorder | 6 |
| Unspecified non-organic psychosis | 2 |
| Delusional disorder | 2 |
| Paranoid schizophrenia | 2 |
Data Collection
Data were collected between November 2010 and October 2011 during individual interviews while following an interview guide that included the questions: What is health for you and how can you control your health? What do you think about your future health and health risks? Three test interviews (not included in the study) were carried out, leading to minor revisions of the interview guide. Each interview lasted for 0.25 to 1.5 hours in free-flowing discussions. The interviews were digitally recorded and transcribed verbatim. The texts were coherent.
Data Analysis
The analysis is guided by the study aim; thus a conceptual framework [14], relevant to the research question, guided the analysis in this study. Before beginning to analyze the data, an initial coding scheme was developed, including three overall fields of interest, to explore concerning beliefs about health, health risks and health expectations. To obtain direct information from the study participants, the texts were first read through line by line to obtain a sense of the whole [26]. The text was then searched for statements related to the coding scheme. Significant statements or answers given by each participant were marked with a highlighter and longer statements were reduced to find the central part of each dialogue. The statements were sorted into three categories, one for each of the fields in the coding scheme, and the statements of each category were then further analyzed and sorted, with statements with similar meaning being brought together in subcategories. The categories and subcategories were compared to find dividing lines in order to establish categories that were separate from each other. The analyses also involved searching for beliefs, patterns and perceptions which could not be coded according to the coding scheme, and these were analyzed later to determine whether they represented a new category or a subcategory of an existing field. In the last step of the analysis, the subcategories and categories were given names that were as close to the participants’ descriptions as possible to avoid excessive interpretation. To ensure trustworthiness the analyses were performed by a psychiatric nurse experienced in the care of people with psychotic disorders and the qualitative method as the coders´ knowledge and experience have a significant impact on the results [32]. Furthermore, the content of the categories was discussed and agreed with second author, which is another way to limit the risks of different interpretations and ensure trustworthiness in qualitative studies [33].
Ethical Considerations
The study was approved by the Ethics Committee of Linkoping University in Sweden Dnr 2010/315-31. Before each interview, the participants were given verbal information about the aim and the implementation of the study, and the voluntary nature of participation, which could be ended at any time without giving a reason. Written, informed consent was obtained in accordance with the declaration of Helsinki [34].
RESULTS
The results are presented in three categories based on the Health Beliefs model [14]: Beliefs about Health, Beliefs about Health Risks, and Health expectations. The variations in each category are presented in subcategories (Fig. 1).
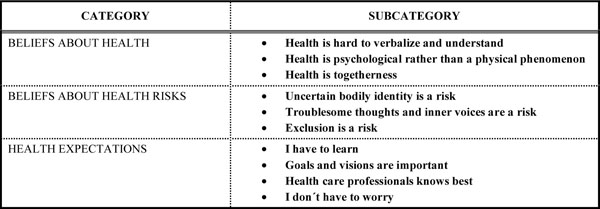
The categories and subcategories explaining health and health risk beliefs among persons with psychotic disorders.
Beliefs About Health
Health is Hard to Verbalize and Understand
This category shows that it is both difficult to understand and verbally explain what health is:
1: It´s impossible to tell what health is. I don’t really think about it like that…I take each day for what it is.
These difficulties were also apparent in participants’ many questions during the interviews about what a healthy behavior is and what to do to achieve health. Some of the questions concerned what food to eat, while other questions concerned which activities were advisable. Furthermore, it was found difficult to keep up with what was considered healthy due to the amount of quite easily accessible but ambiguous health information on the Internet.
Health is a Psychological Rather than a Physical Phenomenon
When health was verbalized by the participants it was first conceptualized as psychological well-being. Beliefs about health as being represented by mental stability and the capacity to put up with different kinds of feelings were prominent. Furthermore, to feel mentally well and to have peace of mind appeared as descriptions of health. Psychological health was also seen as related to feeling good when with others:
9: My son is important… how he makes me happy…and my sisters.
4: it feels good being with others… talking about normal things…hanging out and having a good time.
While the phenomenon of health in general was hard to describe by the participants, beliefs about how physical health manifests itself in the body were rare during the interviews. The salient beliefs about aspects of physical health were general and comprehensive and were defined as being agile and free from pain, and as a phenomenon which needed adjustment to time and one´s own capacity and will:
13: It needs to be adjusted to suit my age and capacity… Not setting unrealistic goals… but managing to do things I want.
Health is Togetherness
Beliefs about health appeared to be related to earlier experiences of togetherness with relatives as well as to cultural behaviors and traditions. Feeling healthy could be associated with memories from the childhood or spending time with family members. Specific lifestyles and cooking traditions were referred to as healthy ways of living. Such beliefs appeared especially distinctly among the foreign-born participants:
4: Health is… in Ethiopia… we drink wine more often which is good to prevent cardiovascular disorders… it helps… also where I am from we are more active interacting with each other… we don’t have to sit alone… we don’t lock the door… we are together. It’s a different social life.
Beliefs About Health Risks
Uncertain Bodily Identity is a Health Risk
It was made clear that health risks were related to beliefs about the body and about beliefs about how others perceive your body. The participants voiced dissatisfaction with the way their bodies looked, and descriptions of themselves as fat were common. The importance of being thin, wearing fancy clothes and looking good was highlighted as evidence of feeling mentally good:
14: It is all about how you look…it is important to look good.
Consequently, the participants described experiences of problematic eating behaviors:
13: I was so afraid of being fat when I was a teen… …It still affects me because I think about it all the time… I am ashamed because of that experience…I ate and threw up…even today I have to force myself to accept that I have eaten too much, it is OK and I’ll stop here… instead of thinking I’ve spoiled it all so I might just as well continue eating.
The body was also seen to reveal to others that one was suffering from a mental illness:
16: If I feel unattractive… I stay inside… feeling people staring at me …I feel insecure about myself…people can tell that I am ill by the way I look.
Uncertainty regarding sexual orientation also appeared to be an issue which negatively affected health:
16: I wonder if I am homosexual… It’s bugging me all the time… if I knew… things would be so much easier… at the same time, I’m scared to find out.
Troublesome Thoughts and Inner Voices are a Health Risk
Major complications of health in everyday life were too many disruptive thoughts or internal voices, as described below:
8: It is difficult because at night I eat in front of the TV… ice cream, sweets, chocolate… if I haven’t spoken to anyone that day… and I hear a lot of voices and they tell me things… it affects me… I feel sorry for myself and eat for comfort… The voices are tiring… it is difficult…
Inner voices and thoughts were described as causing inner stress, which was seen as a health risk.
Exclusion is a Health Risk
It also appeared that limited opportunities for participation in work and society represented prominent health risks. Exclusion could involve beliefs of not having enough strength to be part of the society. It could also be about being scared to be pushed towards a real job. Another reason for exclusion was a belief that one was vulnerable to stress, and fear of becoming psychotic again. One man from Iraq shared his history of stress:
10: We stayed in Sweden for five years without a residence permit… they extended our stay six months at a time… I felt ill and stressed… it is better now…since we got residence permits.
Health Expectations
This category points out that learning, visions and goals regarding health create successful health consequences and that placing the responsibility for health on others can also reduce health expectations.
I have to Learn
Participants found it advantageous to be aware of factors affecting health. Those who found it relevant and interesting to know how to act to achieve health and avoid future health risks were active in searching for this information. Below, it is shown that finding information about what is good for your health was regarded as easy:
10: On the web you can read about the latest research findings and news… they publish news continuously… you don’t even have to look for it.
One girl described how she educated herself in order to increase her knowledge about health and health promotion; an experience that she found useful:
16: I want to learn more about health and psychiatry… I feel the knowledge is useful for me… It encourages reflection.
Participants illustrated the successful consequences of adapting their knowledge. For example quitting smoking was described as necessary as it was believed to be bad for the health. Healthy eating and weight loss were believed to be important to avoid ill-health. Despite the knowledge about the importance of changing unhealthy habits this was experienced as difficult. Sometimes it was described as necessary to decide to accept bad blood tests as these were a consequence of unhealthy habits during a time when not feeling mentally well.
Goals and Visions are Important
Different factors were experienced as important for future health. Motivation was found important, as well as having determination and a positive outlook on the future. One woman told how she had lost weight by being determined and making her mind up to succeed. Dreams about the future created motivation and led to success:
13: I have a positive outlook on the future… Dreams of good things… it is important… if I have a plan… things keep moving.
It was stated that creativity was fundamental to finding health strategies adapted to the individual. Inspiration from having lost weight on different diets was seen as important for motivation. It was also found good to change at the right time:
12: I tried different things… the GI and soup diet… I am kind of lazy… It’s a matter of doing the right thing in the right phase of your life… Jogging is not for me… but aerobics is suitable for me… Right now I find myself in a phase where I can change.
No goals or visions for future health were found to be related to lack of inspiration or motivation, and the smallest change then seemed impossible to manage.
Health Care Professionals Knows Best
The participants believed that they needed lifestyle changes but they had no motivation to change and they talked about external pressure as necessary in order to change:
16: I want to have the energy to be active… it is so hard…I need the stick and the carrot … someone to drag me out… I’m so unmotivated.
Respondents did not verbalize any health expectations and relied on health care professionals to take responsibility for their health:
7: I don’t think about what’s good for my health… staff point out to me what is unhealthy …and make sure I have food to eat…I choose food I like…I don’t know if it is healthy food… but I think I eat what I need… otherwise BST would tell me.
There were participants who believed that the doctors’ advice about what was not good for health was the truth, and then prescribed medicine was seen as necessary. Annual check-ups were felt to be a good thing, and some relied completely on the doctor to tell them if something was wrong with their health. Furthermore, participants relied on health care professionals to give lifestyle advice:
9: My nurse gives me advice about what to eat and how much to exercise… to stay healthy.
I Don´t have to Worry
Some of the participants expressed no health expectations and showed an unconcerned attitude towards their future health and did not worry about their lifestyles. One man who smoked illustrated this clearly:
S: Do you smoke (smelling smoke) 1: Yes… S: How does smoking affect your health…(pause) … 1: No…I don’t know if there are things that are no good for my health. …I don’t think about dangerous things…I feel good.
Lack of health expectations involved not paying attention to unhealthy habits; for example smoking and overweight were not associated with any health risks. Furthermore, these behaviors did not cause worry when feeling good. These good feelings were described as feeling mentally calm and having no physical pain, and were seen as more important than to think of possible future health risks:
2: I can’t figure it out… I don’t know anything special that is not good for health…I don’t think about my future health because I feel good at the moment.
Even if participants expressed awareness of unhealthy habits they did not seem to understand the real significance of these habits for their health. For example, some had increased levels of fasting glucose with a risk of diabetes but did not worry as this was not related to any pain or feelings of being unhealthy. One man told how he was prescribed medicine for his heart but did not worry because you never know what will happen in the future. It was also found that psychological health was given priority over future health or possible physical health risks:
5: It’s relaxing to smoke…it’s my way of decreasing the Haldol effect… it’s good for me…I need to smoke in order to function and to manage the day… I am aware of the risks but I need to smoke to function
DISCUSSION
An overall positive picture of health was found despite the fact that physical health was found to be hard to verbalize and understand among people with psychotic disorders. When health was verbalized it was first conceptualized as psychological well-being, and represented as mental stability, as being able to put up with different kinds of feelings, as feeling good when with others, and as togetherness. Beliefs about how physical health manifests itself were rare, general, and comprehensive and physical health was defined as being agile and free from pain. Beliefs regarding uncertainties about bodily identity as well as limitations in opportunities for participation in work and society represented prominent health risks. Increased awareness of health risks, along with positive health expectations could result from having an interest in learning about health and health risks, and having visions and goals about health. When placing the responsibility for health in others it could cause a lack of health expectations.
The result indicates that there were generally positive health beliefs and participants mainly focused on feeling good here and now rather than worrying about possible future health risks. In other studies, people with SMI likewise have shown more positive attitudes towards physical health than the general population, while most of their clinical risk factors were above the normal parameters [9]. Previous studies illustrate that people with psychotic disorders express worry about developing diabetes due to anti-psychotic treatment [35]. Healthcare professionals need to address health issues early in the management of patients, especially those treated with anti-psychotics which increase the risk of becoming overweight [8].
When health is found hard to verbalize and understand by persons with psychosis it points out the importance of having dialogue in mental health care, where patients have opportunities to put their thoughts and feelings into words. As health was found hard to verbalize, the health belief model could be useful as it is subject-oriented and proposes that health-related behaviors are associated with subjective experiences of illness, the severity of a potential illness, the benefits of adopting preventive action, as well as possible barriers to taking action [14].
In this study it was shown that health first of all appeared as psychological well-being in the participants’ experiences and beliefs, and that it was problematic for them to identify physical aspects of health. Maybe this can be understood as a possible reason for the known limitations among persons with SMI in recognizing and changing their own health risk behavior [18-20]. This, along with being treated less thoroughly by medical health staff [3], presents a risk that these individuals are excluded from physical care when they really need extra support. As medical health professionals are in a position to contribute to identify and support physical health among people with psychosis, there could be advantages if they have basic knowledge of the health beliefs of the group. As it has also been found that mental staff give priority to psychological well-being [36] before physical health among people with psychosis, it also seems important to motivate them to take into consideration physical health issues. Screening for and treating psychotic symptoms is an important role for mental health nurses, as psychotic symptoms drain energy from the person and prevent healthy behavior [18,37,38]. However, physical health is not to be ignored, and actions that address lifestyle and health considerations need to be included in all nursing care of people who have frequent relapses or who are psychotic for long periods of time. Based on the results of this study, nurses also need to consider the impact of troublesome thoughts and inner voices on health interventions [39]. It could be viewed as a challenge to incorporate this philosophy and train mental health nurses to address health interventions among people with psychotic disorders. The challenge is exacerbated by scarce care resources and limited time [17].
One factor increasing the risk of physical health problems is unawareness of health risks. Based on the results of this study, health risk beliefs were not associated with physical health problems that are over-represented among persons with psychosis, such as metabolic deviations [40], cardiovascular diseases and Type 2 DM [1, 41]. Metabolic risks were not frequently discussed; instead health risks were mainly related to uncertain bodily identity, troublesome thoughts and inner voices, and exclusion from society. Most participants in this study felt that being overweight was bad for their looks but was not a health risk. Insecurity about one’s own identity and perceived external stress were seen as major threats to health. It is important to be aware that people with psychotic disorders are vulnerable to stress, and stress increases the risk of relapse [42,43]. In this study, the participants said that they continued smoking due to the positive effect on their psychological well-being, and were not concerned with health risks due to smoking. Thus, people living with psychotic disorders may face difficulties in health performance due to both psychological and physical factors.
Wanting to learn more, along with motivation and creativity, were seen as important for positive health expectations and to encourage action to achieve health among participants, for example by quitting smoking. Successful health behaviors are based on the person’s motivation to change [15]. People with SMIs who quit smoking [23] highlighted expenses due to smoking as the motivator, rather than risk of physical health problems. It was also indicated by participants in this study that they were in need of external pressure in order to make a change, which is something a nurse may not be used to. So, to motivate health behaviors, nurses need to identify what motivates the individual to perform health-behaviors, and where the individual requires pressure from his social network and/or health care staff in order to perform these health behaviors. Health expectations indicate that participants found exercise to be good for achieving health but difficult to perform. Several studies have shown that regular physical exercise is significantly beneficial on both a biological and a psychological level. Positive effects of controlled exercise include improved metabolic responses, increased quality of life, and reduced psychopathological symptoms [44]. Results from a 10-year modified group activity show that there is a relevant correlation between physical activity, quality of life, and medication treatment [45]. One way to motivate physical activities could be to support the involvement of family and friends in these activities, as the participants in this study described togetherness as contributing to wellbeing. This is in line with results from another study which also found that those with a high level of family contact appeared to experience better physical and mental health [46]. Maybe family habits are transferred into the patients´ daily lives with a positive effect on the patient’s health. Thus treatment in a team setting with a holistic and multidisciplinary approach, integrating physical activity into patients’ social lives, could be an effective treatment strategy and may lead to improved physical health in the group. Even though a range of interventions have been performed and evaluated worldwide [20,47-50], there has been little focus on family involvement [51], which indicates a future challenge for researchers. Individual expectations of health motivate a person to follow a particular health behavior [15]. Therefore, individuals will engage in health-related preventive behaviors based on their perceived expectations of the effectiveness of treatments [14].
In this study, some participants described how they were not worried about their health and relied on health care professionals to take responsibility for their health. According to the health belief model [14] an experienced threat towards one’s own health is one of the variables causing people to change risk behaviors, but that was not the case among participants in this study who did not experience threat towards their health and therefor did not seem to understand the importance in performing healthy behavior. Similar findings were found in another study which showed how long-term psychiatric patients were less likely to engage in health promotion compared to non-psychiatric populations. This was because they were found to show lower scores for internal locus of control and higher scores for measures of external locus of control, which means that other people controlled their decisions and their lives [52]. This is suggested to be an adaptive coping mechanism among people with inexplicable episodic symptoms who modify health beliefs towards an external locus of control. People with an external locus of control need to receive adequate support to guide them towards health, as the seriousness of a mental illness is viewed as a factor hindering physical health promotion [15,53]. From the findings that the participants had beliefs that they could totally rely on health care professionals taking responsibility for their health, which may lead to no expectations of good health, empowerment stands out as a core issue in the health promotion directed at persons with SMI.
STUDY LIMITATIONS
This study is unique as it explores beliefs about health, health risks, and health expectations of people with psychotic disorders, none of which have previously been studied. However, some study limitations need to be mentioned, such as the restriction to people with psychotic disorders in outpatient care in Sweden. Thus the results may not be generalizable to all people with SMI worldwide. Nevertheless, the results provide important information on health beliefs and health expectations in a vulnerable population as a first step to understanding. To help the reader make judgments about the transferability of the results to another sample, a rich description of the characteristics of the sample, context and the research process [33,54] has been provided. When interviewing people with psychotic disorders it may be claimed they are not capable of giving informed consent [55], and that we cannot assume that the answers given are not psychotic experiences. In patient-centered care this argument is not valid as it is each patient´s right to make treatment decisions, and that does not mean professionals must agree with all of the patient´s decisions. A patient should be deflected from his or her own decision-making only if there is evidence of danger to the patient or others [56]. To avoid including people who could be of danger to themselves or others, mental health staff who knew the patients made a clinical assessment of their well-being, and people in an acute psychotic phase were not asked to participate. Many people suffering from a psychotic disorder have residual psychotic symptoms [42], so involving people with this experience was regarded as important in order to understand their lived reality. As mental health staff identified participants to include in the study there is a risk that only those most interested in and capable of caring for their health were identified. Based on the broad range of backgrounds and demographics of the participants and the rich data collected we would argue that our sample includes a sufficient range of participants. One thing to reflect on is the age of the participants, which range from 34-66 years (median 48). If a younger population had been studied, further beliefs may have been found as beliefs shape and changes during the entire life process [15].
It could be argued that using the direct content analysis approach makes the findings more likely to support previous theories, rather than being non-supportive [26]. Throughout the study, thoughts and behaviors were elicited, and the health belief model was considered suitable to explain certain health behaviors [14]. An inductive analysis was also performed in order to find experiences and patterns which could not be explained by the health belief model. The participants frequently asked questions about how to improve health. This could be seen as an interview bias. After a total understanding of the interviews was obtained, it was judged that these questions probably reflect awareness about living a healthy life, but also uncertainty about what this involves.
CONCLUSION
As physical health was found to be hard to verbalize and understand, health professionals need to support persons in putting into words their thoughts and feelings concerning physical health. Health was first of all verbalized as psychological, and from a holistic point of view physical and psychological health are inseparable and dependent on each other. In light of such understanding, the results clarify several challenges and also opportunities for changing risk behavior and for health development. Health risks were mainly related to uncertain bodily identity, troublesome thoughts and inner voices, and exclusion. Thus, there was a lack of expressed awareness of physical health risks and perceived threats towards own health, which according to the health belief model [14], is fundamental to performing life-style changes. As health behaviors are determined by our health beliefs, nurses play an important role in supporting people in becoming aware of the physical dimensions of their bodies as well as potential health risks. Striving to learn more about health behaviors and having goals and visions for health were important for positive health expectations, while potential hindrances to positive health expectations included not being worried about health. Nurses need to identify what motivates health behaviors and support people’s participation in their own health process. Reasonable external pressure and social support in health interventions seem to help people to succeed in lifestyle changes.
AUTHOR CONTRIBUTIONS
The first author was responsible for the study concept, design, and data collection and conducted the analysis. The second author double-checked the content of the categories, and both authors drafted the manuscript and made critical revisions of important intellectual content of the manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
The study was performed with grants from Futurum and the Psychiatric Clinic, County Hospital, Ryhov, Jönköping, Sweden. The funders had no involvement with the design, data collection, analysis or interpretation of results.


