Post-Operative Pain Management Practices in Patients with Dementia - The Current Situation in Finland
Abstract
The aim of this study is to describe current post-operative pain management practices for patients with dementia and hip fracture in Finland. Older adults with hip fracture are at high risk of under treatment for pain, especially if they also have a cognitive disorder at the stage of dementia. Previous studies have provided limited information about the quality of acute pain treatment for persons with dementia. In this study data concerning current pain management practices was collected by questionnaire from 333 nursing staff. They worked in surgical wards of seven universities and ten city-centre hospitals. The response rate to the questionnaire was 53%. The data was analysed using factor analysis and parametric methods. Half the respondents (53%) considered that post-operative pain management was sufficient for patients with dementia. Less than one third of respondent nurses reported that pain scales were in use on their unit: the most commonly used scale was VAS. The use of pain scales was significantly related to the respondents’ opinion of the sufficiency of post-operative pain management in this patient group (p<0.001). The findings can be utilised in nursing practice and research when planning suitable complementary educational interventions for nursing staff of surgical wards. Further research is needed to explain the current situation of pain management practices from the viewpoint of patients with dementia.
INTRODUCTION
Hip fractures are common amongst the older population. Fractured hips account for over 7000 injuries in Finland annually [1] and approximately 21- 25% of these patients have at least moderate cognitive impairment [2, 3]. Older adults with dementia are at a high risk of falling and sustaining fractures mainly because of impaired central processing leading to reduced balance and gait [4]. Dementia seems to be an independent risk factor for falling [5].
Acute pain is defined as ‘pain of recent onset and probable limited duration. It usually has an identifiable temporal and causal relationship to injury or disease [6]. Under-treatment of acute pain is more likely to occur in cognitively impaired patients [7-9]. There is evidence of this in acute pain management, where older persons have not received adequate pain management during their hospitalisation [10, 11]. Furthermore older adults with hip fracture are at risk for underassessment of pain and considerable delays in analgesic administration while pain is identified. Persons with severe or moderate dementia and hip fracture received one third the amount of opioid analgesia as cognitively intact subjects [12]. Similar findings were seen among older persons with a total hip or knee arthroplasty. The cognitively intact group received three times more opioid analgesic than the cognitively impaired group [13].
Proper pain management includes paying attention to human subject rights. Frail older adults with dementia lack verbal communication ability, and so are at high risk of insufficient pain management. The role of nursing staff is crucial in asserting quality care for this vulnerable patient group [14]. Insufficient pain treatment in older patients with hip fracture causes not only human suffering but longer stays in hospital, delayed ambulation and long-term functional impairment [10, 15].
NURSING PRACTICES IN ACUTE PAIN MANAGEMENT
Evidence-based principles to follow include providing pain medication prior to painful events (such as dressing or wound healing) [16-19], prior to physical activity [16-18] and regularly [16, 19-22], administering analgesics around the clock [16, 20-23], assessing and documenting the effect of analgesics (including side-effects) [20, 21, 23, 24], assessment for post-operative pain at least every four hours during the first days [20-21, 23] and assessing pain by means of pain scales [16, 19-21, 23, 25].
Providing adequate pain medication prior to painful events (such as dressing or wound healing) is essential, because post-surgical movement associated pain is more intense (95-226%) than pain at rest [17]. However it seems that movement associated pain has been a minor concern in managing post-surgical pain [17, 18].
In an acute care setting there is a need for baseline and routine follow-up pain intensity ratings at least every 4 hours to guide pain management and treatment decisions [24]. A study by Mehta and colleagues [16] found that only 7% of cognitively impaired surgical patients (62% fractures as an aetiology of acute pain) were placed on an around the clock analgesic regimen. Such limited use of around the clock analgesic administration could be explained by a lack of familiarity with, and/or application of existing evidence-based pain management guidelines.
Cognitively impaired patients are often able to self report pain scores [16, 25-27]. The golden standard for pain assessment is self reporting and it is the most reliable indicator of presence or intensity of pain [28, 29]. People with mild dementia can provide valid reports of pain, but people with more severe cognitive impairment may have difficulties doing so or be unable to clearly report pain [29]. The intensity of pain is measured for example by Visual Analogue Scale (VAS), Verbal Descriptor Scale (VRS), and Faces Scale [30]. The VAS is widely used, especially in hospital settings [25] and it consists of a 100 mm horizontal line with verbal anchors at both ends and no tick marks [20]. The patient is asked to mark the line and the ‘score’ is the distance in millimetres (0 to 100 mm) from the left side of the scale to the mark. The VAS requires the ability to discriminate subtle differences in pain intensity and may be difficult for some older persons to complete [20, 25, 30]. A tool that has been specifically recommended for use with older adults is the Verbal Descriptor Scale (VRS) (0=no pain, 4=unbearable pain) [30]. It has been tested also in older persons with mild to moderate cognitive dysfunction [25, 27]. If a person is unable to report pain verbally, one option is to assess pain through behavioural tools [28]. The Pain Assessment in Advanced Dementia Scale (PAINAD) developed by Warden et al. 2003, assesses five categorical items: breathing, negative vocalisation, facial expression, body language and consolability [31]. Items are scored from 0 (no pain) to 10 (most severe pain). Each category is scored of 0 to 2 indicating intensity of behaviour.
Herr & Titler et al. [24] assessed 1454 medical records from patients with hip fractures and found, that although nearly all had some documentation related to pain (99%), only 54% had pain assessed with a numeric rating scale, 4% with a non-numeric rating scale (such as verbal descriptor or faces scale), and 7% with nonverbal pain behaviours. Thus one third of patients had no assessment of pain documented.
NON-PHARMACOLOGICAL TREATMENT PRACTICES IN ACUTE CARE SETTING
Analgesics are the cornerstone of acute pain management [17, 21]. However there are many non-pharmacological pain treatments and in an acute care setting they are used supplementary to effective pharmacological treatment methods [32, 33]. Some strategies, such as imagery or relaxation techniques, may not be feasible for cognitively impaired older adults due to communication difficulties [14]. The most frequently used non-pharmacological intervention for those hospitalised with a hip fracture includes repositioning, followed by use of pressure relief devices and cold application [16, 34].
Anxiety has been shown to be one predictive factor and is associated with a higher intensity of post-operative pain [20, 35]. The relationship between anxiety and pain is reciprocal, so that fear exacerbates pain [35] and pain in turn appears to promote fear and anxiety [29]. Attempting to alter the patient’s emotional state, from stress or fear to comfort or peace, should also be an effective feature of certain pain management practices such as therapeutic communication (e.g. quieting and consoling or soothing supportive touch) and cueing [36]. Individuals with dementia have a decreased threshold for stress from the environment, so the need for a peaceful and comfortable environment without e.g. visual, auditory or thermal stress, is highlighted [36].
The use of particular music to divert attention from pain and to promote a sense of relaxation and well-being has long been a popular approach. According to a Cochrane review, listening to music reduces pain intensity and opioid requirements after surgery, but the magnitude of benefit is small [37]. This result concurs with a prospective clinical study; listening to music has been shown to alleviate pain intensity and pain distress significantly after abdominal surgery [38]. There is little consistent evidence of benefit from massage in the treatment of post-operative pain. Evidence for benefits from post-operative local cooling is mixed. Significant reductions in opioid consumption and pain scores after a variety of orthopedic operations have been reported; other studies have shown no such reductions [20]. In one study based on the medical records of caregivers caring for hospitalised cognitively impaired patients with acute pain, the results indicated that non-pharmacological methods (such as distraction, repositioning and cold packs) were used frequently (75%) [16].
There are some limitations to the use of non-pharmacological therapies, because the evidence base regarding the use of non-drug therapies to manage acute pain requires further development; current knowledge does not support consistent outcomes from these therapies [32]. Further research is needed to provide evidence based knowledge about the effectiveness of these methods [20, 32]. The absence of evidence regarding the effects of many non-pharmacological therapies doesn’t automatically mean that these methods are ineffective. It’s advisable to use all safe methods which seem to be effective.
In the last decade, there has been a growing interest about pain in older people [39, 40]. Research is needed to develop effective strategies for managing pain among older patients with dementia in the acute-care setting [19].
The purpose of this study was to describe post-operative pain management practices in hip fractured patients with dementia. We used the following research questions:
- Which practices do the nursing staffs apply to manage post-operative pain in patients with hip fracture and dementia?
- How are the background variables of nursing staff related to their pain management practices?
MATERIALS AND METHODOLOGY
Design
A cross-sectional design was used to develop a questionnaire and to evaluate the current situation of post-operative pain management practices for patients with dementia as evaluated by nursing staff. All university and city-centre hospitals where the incidence of first hip fractures was over 100/year were included. The 17 eligible hospitals treated approximately 70% of all patients admitted to hospital for hip fractures in Finland.
Development of Questionnaire
Because no questionnaire was found to assess post-operative pain management practices by nursing staff in people with dementia in an acute care setting, a new questionnaire was developed. The scale was based on previous research studies (Table 1). The pain management practices presented in this article, are part of the total “Post-operative Pain Management in Patients with Hip Fracture and Dementia” scale which exists alongside the “Pain Treatment Practices” subscale (17 items), pharmacological pain treatment, knowledge about analgesic side effects, the barriers of pain management, pain related behavioural changes, pain documentation, the most effective non-pharmacological pain treatment practices, operational preconditions for developing pain management and expectations for pain management. The first part of the questionnaire (Table 2) focussed on demographic information, including hospital, gender, age, occupation, work experience both at current employment and in health care generally, contract, employment arrangements and work shifts. Other background information (Table 3) included participation in update training, and opinions regarding the primary aim of pain management and the sufficiency of post-operative pain management. Face validity was established by asking two pain experts (one a docent in nursing science and one a professor of pharmacological medicine), one professor of nursing science and eight doctorial students to review the questionnaire. The section “post-operative pain management practices” is a part of questionnaire which was developed to measure the current situation in post-operative pain management. The whole questionnaire was pilot tested in one surgical unit (n=19) before use. The nursing staff stated on a separate form that all the items were clearly expressed and easy to complete. After pre-testing, the questionnaire was simplified so that an individual question asked only one thing. Additionally the scale was made easier to use by modifying its visual presentation. Nursing staff were asked how post-operative pain management practices are applied on their units when caring for patients with dementia.
Questionnaire Items and Related Studies (Author(s) and Year of Publication)
| Questionnaire Items | Author(s) and Year of Publication |
|---|---|
| Helping with daily activities (e.g. washing, dressing) | Herr & Bjoro et al. 2006 [21] |
| Providing pain medication regularly | MacIntyre & Shug et al. 2010 [20]; Mehta & Siegler et al. 2010 [16]; Kelley, Siegler & Reid 2008 [19]; Herr, Bjoro et al. 2006 [21]; Herr & Titler et al. 2004 [22] |
| Repositioning | MacIntyre & Shug et al. 2010 [20]; Mehta & Siegler et al. 2010[16]; Herr & Bjoro et al. 2006 [21]; Titler & Herr et al. 2006 [34] |
| Administering analgesics around the clock | Coker E & Papanaioannou et al. 2010 [23]; MacIntyre & Shug et al. 2010 [20]; Mehta & Siegler et al. 2010 [16]; Herr & Bjoro et al. 2006 [21] ; Herr & Titler et al. 2004 [22] |
| Providing pain medication prior to painful events (such as dressing or wound healing) | Srikandarajah & Gilron 2011[17]; Kehlet 2011[18]; Mehta & Siegler et al. 2010 [16]; Kelley, Siegler & Reid 2008 [19] |
| By using cold therapy (e.g. cold bags) for pain relief | MacIntyre & Shug et al. 2010 [20]; Mehta & Siegler et al. 2010[ 16]; Herr & Bjoro et al. 2006 [21]; Titler & Herr et al. 2006 [34] |
| Providing pain medication prior to physical activity | Srikandarajah & Gilron 2011[17]; Kehlet 2011[18]; Mehta & Siegler et al. 2010 [16] |
| Quieting and consoling | Kovach & Logan et al.2006 [36] ; Feeney 2004 [42] |
| Assessment and documentation of effects of analgesics | Coker E & Papanaioannou et al. 2010 [23]; MacIntyre & Shug et al. 2010 [20]; Herr & Titler 2009; Herr & Bjoro et al. 2006 [21] |
| Assessment for pain at least every four hours | Coker E & Papanaioannou et al. 2010 [23]; MacIntyre & Shug et al. 2010 [20]; Herr & Bjoro et al. 2006 [21] |
| Soothing, supportive touch | Kovach & Logan et al.2006 [36] |
| Assessing pain by means of pain scales | Coker E & Papanaioannou et al. 2010 [23]; MacIntyre & Shug et al. 2010 [20]; Mehta & Siegler et al. 2010 [16] ; Pesonen & Kauppila et al. 2009 [25]; Kelley, Siegler & Reid 2008 [19]; Herr & Bjoro et al. 2006 [21] |
| Presence when patient seems to be in pain | Kovach & Logan et al. 2006 [36] |
| Peaceful and comfortable environment (e.g. quiet, lights, air conditioning) | Herr & Bjoro et al. 2006 [21]; Kovach & Logan et al.2006 [36] |
| Heat therapy (e.g. warm bags) | MacIntyre & Shug et al. 2010 [20]; Herr & Bjoro et al. 2006 [21] |
| Music therapy | MacIntyre & Shug et al. 2010; Cepeda & Carr et al.2006; Herr & Bjoro et al. 2006 |
Post-Operative Pain Management Practices (Factor Structure, Factor Loadings, Correlations and Internal Consistency of Questionnaire)
| Questionnaire items | Factor 1 Analgesic Treatment Practices | Factor 2 Emotional Support | Factor 3 Physical Methods | Factor 4 Specific Methods |
|---|---|---|---|---|
| 1. Providing pain medication prior to painful events (such as dressing or wound healing) (n=323) | 0.711 | |||
| 2. Providing pain medication prior to physical activity (n=322) | 0.659 | |||
| 3. Assessment and documentation of effects of analgesics (n=320) | 0.559 | |||
| 4. Providing pain medication regularly (n=323) | 0.472 | |||
| 5. Administering analgesics around the clock (n=321) | 0.416 | |||
| 6. Assessing pain by means of pain scales (n=312) | 0.374 | |||
| 7. Assessment for pain at least every four hours (n=316) | 0.353 | |||
| 8. Quieting and consoling (n=323) | 0.745 | |||
| 9. Soothing, supportive touch (n=327) | 0.688 | |||
| 10. Presence when patient seems to be in pain (n=329) | 0.551 | |||
| 11. Music therapy (n=326) | 0.680 | |||
| 12. Heat therapy (e.g. warm bags) (n=318) | 0.613 | |||
| 13. Peaceful and comfort environment (quiet, lights, air conditioning) (n=324) | 0.552 | |||
| 14. Helping with daily activities (e.g. washing, dressing) (n=327) | 0.773 | |||
| 15. Repositioning (n=325) | 0.602 | |||
| 16. By using cold therapy (e.g. cold bags) in pain relief (n=326) | 0.328 | |||
| Spearman’s correlation coefficients for individual items with each subscales (for total scale 0.311- 0.601) | 0.480 - 0.696 | 0.757- 0.806 | 0.692-0.796 | 0.692- 0.799 |
| Eigenvalue | 3.75 | 1.85 | 1.701 | 1.306 |
Kaiser-Mayer-Olkin measure of sampling adequacy: 0.76, Barthlett’s test of sphericity significance: p < 0.001.
* Only >0.30 Factor loadings are presented. Extraction method is Maximum Likelihood Rotation method: Varimax with Kaiser Normalisation.
Demographics of Nursing Staff (%)
| Variable | % |
|---|---|
| Gender (n=333) | |
| Female | 95 |
| Male | 5 |
| Age (n=330) | |
| < 36 years | 36 |
| 36-50 years | 37 |
| > 50 years | 27 |
| Occupation (n=330) | |
| Head nurse | 2 |
| Staff nurse | 5 |
| Registered nurse | 76 |
| Practice nurse | 15 |
| Other | 2 |
| Work experience in current unit (n=329) | |
| < 5 years | 36 |
| 5-15 years | 36 |
| >15 years | 28 |
| Work experience in health care (n=329) | |
| < 5 years | 14 |
| 5-15 years | 40 |
| >15 years | 46 |
| Contract (n=328) | |
| Permanent | 82 |
| Deputy | 18 |
| Employment arrangement (n=330) | |
| Fully time | 88 |
| Part time | 12 |
| Work shifts (n=328) | |
| Daytime jobs | 6 |
| Two-shift work | 12 |
| Three-shift work | 80 |
| Night work | 2 |
Procedures
A contact person from each unit distributed the questionnaires and spoke to the participants. A cover information letter detailing the procedure was attached to the questionnaire and participants were asked to respond. The data collection period was March to May 2011. In April participants were reminded to fulfil the questionnaire.
Data and Methods
Pain management practices among 333 nursing staff were investigated by calculating percentages of the extent of opinions based on a five-point Likert scale (1= completely disagree, 2= disagree to some extent, 3= neither agree or disagree, 4= agree in some extent, 5= completely agree). The individual opinions are interpreted so that number 4 and 5 indicate agreement and numbers 1 and 2 disagreement. The mean sum variables, which were derived from factors, were classified into two classes in which the value < 3.5 indicated disagreement and value ≥ 3.5 agreement.
Research data was analysed using SPSS 17.0 for Windows (SPPS Inc., Chicago, Il, USA). Descriptive statistics were generated for the demographics of the nursing staff. The normality of distribution was analysed by means of histograms. The Two Independent Samples T-test and Analysis of Variance were used to investigate whether there were significant differences in the responses of the nurses based on background variables. Statistical significance was set at P value < 0.05. Factor analysis was performed to refine the subscales (as a part of the scale development) and to investigate the underlying factor structure of each subscale [42]. Furthermore, internal consistency and reliability for the 16-item scale and associated subscales were supported by Spearman’s correlation (Table 2) [42]. The responses to participants’ answers about pain management practices were examined by calculating percentages of opinion for each statement. The two open-ended questions (other non-pharmacological pain management practices, and use of pain scales) were analysed by the Qualitative Data Analysis & Research Software ATLAS.ti 6.2.25 and qualitative content analysis was performed by categorising the data to different subcategories. After that another open-ended question “which pain scales do you use when assessing post-operative pain in patients with hip fracture and dementia?” was quantified by modifying it to SPSS-data.
Factor analysis was performed to create the final questionnaire scale and to investigate its underlying factor structure. The Explanatory Factor analysis was conducted with Varimax rotation. This is method of rotation that minimizes the number of variables with high loadings on a factor, thereby enhancing the interpretability of the factors. Varimax rotation results in factors that are uncorrelated [43]. Only factors with eigenvalues greater than 1.0 were retained. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.760 so all items were retained [44], with exception of one item (“giving pain medication”) because item-total correlation was below 0.2. Bartlett test of sphericity was used to test the multivariate normality of the set distributions. Asignificance value of (p<0.001) indicated that the data did not produced an identity matrix or differ significantly from identity [44]. Internal consistency was analysed for both total scale and subscales. Table 2 presents the Spearman’s correlation ranges of individual items correlations with the subscales and total scale resulting from the internal consistency analyses [42]. The four factor solution explained 53.8% of the total variance. The first factor explained 23.4%, the second factor 11.6%, the third factor 10.6% and the fourth factor 8.2% of the total variance. The findings indicated that the first factor was related to analgesic treatment practices in pain relieving, the second to emotional pain relieving methods, the third to the different physical manners in pain management, and the fourth to specific post-operative pain management practices in patients with dementia. The associated items are presented in Table 2.
Description of the Participants
Data was collected from nursing staff in seven university and ten city-centre hospitals in Finland (N=634). The questionnaires were returned by 53% of the nursing staff (n=333). Their mean age was 42 (SD± 11.6). The median of experience in their current working place was 7 years and the median of their experience in health care was 15 years. Table 3 summarises the respondent demographics.
Most of the nursing staff had not undergone any update of training concerning post-operative pain management in individuals with dementia (94%). The primary goal in pain management was slight pain, which does not prevent normal functioning (67%). Over half held the opinion that pain management is sufficient among patients with dementia. The other background information is presented in Table 4.
Participating in Update Training, Primary Aim and Sufficiency of Pain Management (%)
| Variable | % |
|---|---|
| Participating in update training (n= 332) | |
| No | 94 |
| Yes | 6 |
| The primary aim of post-operative pain management in patients with dementia (n=325) | |
| Complete pain relief | 25 |
| Slight pain, which does not prevent normal functioning | 67 |
| Reasonable painlessness with slight discomfort | 3 |
| Pain relief only at peak periods | 2 |
| Sufficiency of post-operative pain management in people with dementia (n=324) | |
| Pain management is sufficient | 53 |
| Pain is undertreated | 47 |
RESULTS
The results indicate that preferred methods in pain management among nursing staff were “specific pain management practices” (Factor 4) (mean 4.6±0.46), i.e. repositioning (100%), helping with daily activities (97%) and cold applications (93%). The most common analgesic administration practices (mean 4.1±0.55) were providing pain medication prior to painful events (96%), prior to physical activity (94%) and regularly (96%). The agreement of opinion that the effects of analgesic were assessed and documented was 73%. Pain was seldom assessed by means of pain scales (31%). Quieting and consoling (85%) was the most popular method among “emotional practices” (Factor 2) and presence when the patient seemed to be in pain (42%) was the least common practice. “Physical methods” (Factor 3) including music therapy (6%) and heat therapy (17%) were not preferred pain relieving methods (mean 2.3±0.85), although organising a peaceful and comfort environment scored more highly (38%). Less than one third agreed that some pain scales were in use during their work, and the most commonly used scale was VAS (n=75) (Table 8). Those who considered pain management to be sufficient thought that pain scales were in use in their unit nearly twice as often (40% agreement) as the group who thought that pain management was insufficient (21 % agreement) (p< 0.001). Tables 5 and 6 present the participant responses.
Because the distributions of variables were normal the parametric tests Two Independent Samples T-test and Analysis of Variance were applied to investigate whether there were significant differences in the responses of the nurses based on background variables. Statistically significant differences (Table 7) in the responses of the nurses depending on background variables were seen in “emotional pain relieving methods” as compared with gender (p= 0.013) and participation in update training (p =0.035). Females agreed that their current working unit more often applied “emotional pain relieving methods”. Those who had participated in update training thought that the uses of “emotional pain relieving methods” were more common compared with those who hadn’t participated. Those who considered pain management to be sufficient also agreed that general “analgesic treatment practices” (Factor 1) (p< 0.001) and “physical methods” (Factor 3) (p=0.007) were used more often in their units. Permanent staff considered that the use of “physical methods” were more unusual compared with deputy personnel (p=0.043). Those who were employed full time (p=0.006), agreed that “specific methods” were used more often when compared with those working part time. The largest number of differences as regards pain management practices (Factors 1-3) could be seen between those working in different hospitals.
The open-ended question “Which other post-operative pain management practices in patients with hip fracture and dementia are applied in your working place?” were analysed by ATLASti-software using qualitative content analysis.
Post-Operative Pain Management Practices Subscales (Mean, SD, %)
| Subscales | Mean (Range 1-5) | SD | % of Agreement (Mean Sum Variable ≥3,5) |
|---|---|---|---|
| Total scale | 3.7 | 0.54 | 71 |
| Specific pain management practices (Factor 4) | 4.6 | 0.46 | 98 |
| Analgesic treatment practices (Factor 1) | 4.1 | 0.55 | 86 |
| Emotional pain relieving methods (Factor 2) | 3.6 | 0.75 | 60 |
| Physical methods (Factor 3) | 2.2 | 0.85 | 8 |
Nurses Assessment of Post-Operative Pain Management Practices in Patients with Hip Fracture and Dementia (%)
| Questionnaire Items | Disagree (Likert 1+2) % | Neither Agree or Disagree (3) % | Agree (Likert 4+5) % |
|---|---|---|---|
| Repositioning (n=325) | 0 | 0 | 100 |
| Helping with daily activities (e.g. washing, dressing) (n=327) | 1 | 2 | 97 |
| Providing pain medication regularly (n=321) | 2 | 2 | 96 |
| Providing pain medication prior to painful events (such as dressing or wound healing) (n=323) | 2 | 2 | 96 |
| Providing pain medication prior to physical activity (n=322) | 3 | 3 | 94 |
| Administering analgesics around the clock (n=321) | 4 | 3 | 93 |
| By using cold therapy (e.g. cold bags) in pain relieving (n=326) | 3 | 4 | 93 |
| Quieting and consoling (n=323) | 4 | 11 | 85 |
| Assessment and documentation of effects of analgesics (n=320) | 12 | 15 | 73 |
| Soothing, supportive touch (n=327) | 16 | 13 | 71 |
| Assessment for pain at least every four hours (n=316) | 18 | 13 | 69 |
| Presence when patient seems to be in pain (n=329) | 31 | 27 | 42 |
| Peaceful and comfort environment (e.g. quiet, lights, air conditioning) (n=324) | 35 | 27 | 38 |
| Assessing pain by means of pain scales (n=312) | 51 | 18 | 31 |
| Heat therapy (i.e. warm bags) (n=318) | 69 | 14 | 17 |
| Music therapy (n=326) | 88 | 6 | 6 |
Differences in Nurse Responses by Gender, Participating in Update Training, Sufficiency of Pain Management, Contract, Employment Arrangement and Hospitals
| Background Variable | Analgesic Treatment Practices Factor 1 | Emotional Support Factor 2 | Physical Methods Factor 3 | Specific Methods Factor 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Gender | ||||||||||||
| Male | 15 | 4.0 | 0.49 | 15 | 3.2 | 0.66 | 15 | 2.1 | 1.1 | 15 | 4.7 | 0.41 |
| Female | 315 | 4.0 | 0.55 | 315 | 3.7 | 0.75 | 312 | 2.2 | 0.83 | 315 | 4.6 | 0.47 |
| ns.* | p=.013 | ns. | ns. | |||||||||
| Participating in update training | ||||||||||||
| Yes | 20 | 4.2 | 0.43 | 20 | 4.0 | 0.63 | 20 | 2.4 | 0.83 | 20 | 4.6 | 0.57 |
| No | 309 | 4.0 | 0.55 | 309 | 3.6 | 0.76 | 306 | 2.2 | 0.85 | 309 | 4.6 | 0.46 |
| ns. | p=.035 | ns. | ns. | |||||||||
| Sufficiency of pain management | ||||||||||||
| Undertreated | 147 | 3.9 | 0.59 | 151 | 3.6 | 0.77 | 148 | 2.1 | 0.76 | 151 | 4.6 | 0.47 |
| Sufficient | 169 | 4.2 | 0.46 | 170 | 3.6 | 0.73 | 170 | 2.3 | 0.90 | 170 | 4.7 | 0.46 |
| p< .001 | ns. | p=.007 | ns. | |||||||||
| Contract | ||||||||||||
| Permanent | 259 | 4.1 | 0.54 | 265 | 3.7 | 0.75 | 262 | 2.1 | 0.83 | 265 | 4.6 | 0.47 |
| Deputy | 60 | 4.0 | 0.57 | 60 | 3.6 | 0.77 | 60 | 2.4 | 0.90 | 60 | 4.6 | 0.45 |
| ns. | ns. | p=.043 | ns. | |||||||||
| Employment arrangement | ||||||||||||
| Fully time | 282 | 4.1 | 0.55 | 287 | 3.6 | 0.76 | 285 | 2.2 | 0.84 | 287 | 4.7 | 0.44 |
| Part time | 39 | 4.0 | 0.50 | 40 | 3.5 | 0.75 | 39 | 2.1 | 0.91 | 40 | 4.4 | 0.53 |
| ns. | ns. | ns. | p=.006 | |||||||||
| Different hospitals | ||||||||||||
| All hospitals | 324 | 4.1 | 0.55 | 330 | 3.6 | 0.75 | 327 | 2.2 | 0.85 | 330 | 4.6 | 0.46 |
| p< .001 | p=.009 | p< .001 | ns. | |||||||||
| University hospitals | 153 | 4.1 | 0.58 | 156 | 3.7 | 0.80 | 154 | 2.1 | 0.76 | 156 | 4.6 | 0.44 |
| City-centre hospitals | 171 | 4.1 | 0.52 | 174 | 3.6 | 0.71 | 173 | 2.3 | 0.91 | 174 | 4.6 | 0.48 |
| ns. | ns. | ns. | ns. | |||||||||
* ns. =not significant.
When analysing the open ended questions, clear pattern of meaningful communication in pain management practices emerged (Fig. 1). The nursing staff highlighted that patients with dementia need specifically peaceful working approach in order to make feeling comfortable and peaceful. Appropriate information about what is going to happen next and informing about the cause of pain were also seen as to be part of pain management. Positive interaction included humour and trying to get the patient to move by singing together. Presence of relatives was also highlighted in order to get patient feel more peaceful. The nursing staff mentioned that patients with dementia need especially peaceful environment with small rooms. Also concrete suggestions such as proper lifting technique, mobilisation and in case of problems in swallowing the appropriate way in giving analgesics for enhancement of pain management were mentioned.
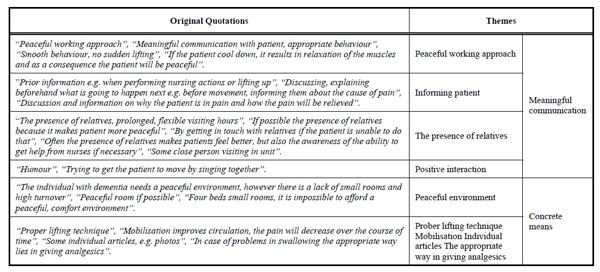
The open ended question “Other post-operative pain management practices”.
Different problems in non-pharmacologic pain management were mentioned often. Lack of resources and time to use non-pharmacological pain relieving methods and insufficient staffing were among problems related to pain management. Also the absence of means emerged in some comments. Some of the nursing staff mentioned that non pharmacological methods are ineffective in post-operative pain management and there is no evidence of effectiveness of certain therapies. One comment related that these methods work but in practice they cannot be applied because of overloaded and busy wards and there is also lack of air conditioning, music or massage.
Lack of resources and time: “Primary medication, but if there is enough time, it’s possible to use non-pharmacological pain relieving methods and healing”, “I prefer these methods, but limited time is often the barrier”, “More nursing staff in order to have time to stay close to the patient”.
The absence of means: “The means are limited”, “Non-pharmacological pain relieving methods are ineffective in post-operative pain management”, “These methods work, but in practice it’s impossible to adopt them because of overloaded and busy wards. We have no air conditioning, no music or massage or Transcutaneous nerve stimulation (TNS)!”, “There is no chance to apply non-pharmacological methods because of the small, four bedded rooms”, ”acute pain? - there are few non-pharmacological methods”, “There is no evidence of the effectiveness of TNS or heat therapy”.
The other open-ended question was a question concerned with how post-operative pain management practices were applied on the unit when caring for older adults with hip fracture and dementia. To the item “assessing pain by means of pain scales” was added the open-ended question: “What kind of pain scales do you use in pain assessment in patients with hip fracture and dementia?” (Table 8). The most often mentioned pain scale was VAS (75 related quotations). VRS (0-4 verbal rating scale) was mentioned in 66 quotations, general behavioural assessment in 83 quotations and common verbal assessment in 60 quotations. The unit of analysis (citation) was not the total comment, but the associated part of the comment e.g. “In our unit we have common practices in pain assessment; we use either NRS 0-10 or VRS, which is verbal rating scale. If the patient is unable to communicate, the PAINAD, behavioural pain assessment tool, is being road tested in our unit”. This comment mentioned three different ways (=codes) to measure the pain: VRS, NRS and PAINAD (=tree quotations).
Results of Open-Ended Question- what Kind of Pain Scales Do you Use in Pain Assessment for Patients with Hip Fracture and Dementia? (Total 231 Comments Including 348 Quotations)
| Codes | Number of Quotations |
|---|---|
| Behavioural observation | 83 |
| VAS (0-10 cm) | 75 |
| VRS (verbal rating scale 0-4) | 66 |
| Verbal assessment | 60 |
| NRS (0-10) | 27 |
| Physiological functions (e.g. heart rate, blood pressure, breathing rate) | 17 |
| Facial pain scale | 17 |
| PAINAD | 3 |
The nursing staff also used common pain scales in combination with behavioural assessment “It depends on the degree of cognitive impairment, verbal or numerical (NRS 0-10) pain scales. Facial expression, motions, moaning, agitation, confusion, pain on movement or on touching a painful area, and keeping track of reactions”. For non communicative patients, only one pain scale - behavioural pain assessment tool PAINAD -was mentioned (three times, from two hospitals). Instead observation of behavioural signs of pain was quite common practice among staff.
DISCUSSION
Discussion of the Findings
The results suggest that over half the nursing staff considered post-operative pain management to be sufficient among patients with hip fracture and dementia. Only one third reported that some pain scales were in use on their working unit. These results contradict previous findings in which only one third of patients had no objective assessment of pain documented [24]. The finding that the use of pain scales is significantly related to sufficiency of post-operative pain management (p< .001), warrants further examination. It is possible that there is another unknown interpretative element, which may explain the finding. The most commonly used pain scale was VAS, which is considered invalid when assessing pain in patients with moderate to severe dementia [25, 30]. The preferred tool for pain measurement is the Verbal Rating Scale (VRS), which seems to be a valid instrument for assessment of pain in patients with mild to moderate cognitive impairment [25]. There is evidence that nurses assess pain infrequently, and rarely use pain assessment tools [41]. In this study the effects of analgesics were frequently assessed and documented (73%) although the use of pain scales was insufficient.
Repositioning, cold therapy and helping with daily activities were commonly used methods of pain management. Medication prior to painful events (96%) and physical activity (94%) were also common practices. However, movement-evoked pain has not been the focus of the main post-surgical studies, according to meta-analysis conducted by Srikandarajah and Gilron (2011) [17]. Assessment of pain every 4 hours was often reported (69%). This result contradicts previous findings where medical records after admission for acute hip fracture were assessed. Four hourly assessment was performed in 37% cases during first 24 hours and in 6% cases during first 72 hours [22]. In this study the main differences in the use of various pain management practices were between hospitals. In those hospitals where “analgesic treatment practices” were used more often, the “emotional nursing practices” were also more commonly used methods.
The nursing staffs have an important role in enabling the presence of relatives or close friends who knows the persons individual ways to express pain. Knowing the person is highlighted when trying to discover the ways that cognitively impaired individuals express the pain, because the ability to express pain is often decreased in people with dementia [14, 20, 29]. Moreover meaningful communication on behalf of staff and relatives, such as peaceful, emphatic interaction and providing appropriate information to patients by keeping them updated (e.g. about what is going to happen and the cause of their pain) is important, because anxiety and distress are in connection to post-operative pain. According to systematic review [35] it was found that anxiety is one of the most significant predictive factors for intensity of post-operative pain. Psychological distress can increase post-operative analgesic consumption. When examining the relationship between pain and negative affects in older adults following orthopaedic surgery, the only significant predictor of pain in this population was state of anxiety [45]. Skilled communication is associated with improvement in pain relief. In a cross-sectional study of nine hospitals, Gittell and colleagues (2000) found that the better the communication, the better the postsurgical pain relief [46]. Individuals with dementia have a decreased threshold for stress from the environment, so a peaceful and comfortable environment without, for example, visual, auditory or thermal stress, is highlighted [36]. A focus on “organising a peaceful and comfortable environment” was not common practice (38 % agreement) in units. On the other hand, the nursing staff also suggested that the means for staff to organise a comfortable environment is limited due to small, noisy, multi-beds room and lack of time.
Nurses are the professional group mainly responsible for assessing pain, and administering and evaluating the quality of pain relief in older people. On this basis, they are also the group most likely to affect improved patient outcomes [14, 47]. This research provides insight into the current utilisation of certain pain management practices, and the findings should be utilised for the nursing practice when planning suitable complementary educational interventions.
Reliability, Validity and Trustworthiness of the Study
This research has limitations. It was conducted using a newly developed instrument and after analysing the open-ended questions, new aspects in nursing practices were found, such as a peaceful working approach, facilitating the presence of relatives and providing appropriate information to patients. Secondly, the response rate was 53%, which can be a risk for the potential differential dropout of subjects. Response rates between different hospitals varied greatly, so that in university hospitals the response rate was 59% and in city-centre hospitals 48%. The face-validity was conducted and the questionnaire was pre-tested in only one surgical unit (n=19) before use. Internal consistency and reliability for the 16-item scale was supported by Spearman’s correlation [42]. Each item correlated with total scale (≥ .311) and with associated four factors (≥ .480). The structure validity was established by generating a Factor analysis. The four Factor solution accounted approximately 54% of the total variance.
The open-ended questions were analysed by content analysis but it is important to be aware that text always involves multiple meanings and there is always some degree of interpretation. This is an important issue when discussing the trustworthiness of findings in qualitative content analysis [48]. The primary documents were read carefully several times and the statements given under each code were checked afterwards in order to obtain objective interpretation.
Ethical Considerations
Permission to conduct the study was obtained from each hospital according their individual procedure. Ethical permission was obtained from the Ethical Committee of Northern Savo District (83/2010). Nursing staff participated in this study voluntarily and the information was obtained anonymously.
CONCLUSIONS
This pilot study produced new information about perceived nursing practices in the management of post-operative pain in patients with hip fracture and dementia. The following conclusions were drawn on the basis of study:
- Over half the nursing staff considered post-operative pain management to be sufficient for patients with hip fracture and dementia. However, this does not delete the possibility of undertreatment, because the pain assessment is very demanding task in demented persons.
- The most common pain scale was VAS, which is not suitable for most people with dementia. There is a need for educational intervention, in which different pain scales and assessments of behavioural expressions of pain are implemented in practice according to the severity of cognitive impairment.
- There is also a need to take into account the emotional aspects of pain relief for people with dementia. The presence of relatives or other close persons can help in recognising individual ways of expressing pain and provide meaningful interpersonal communication in decreasing anxiety among patients with dementia.
- Preferred non-pharmacological methods were repositioning, cold therapy and helping with daily activities.
- Providing pain medication prior to movement or painful events, administering analgesic regularly and around the clock were commonly used pharmacological pain relieving methods.
Based on this study, there is a need for update training for nursing staff about using different pain scales according to the degree of cognitive impairment. Educational intervention is especially reasonable because a more common use of pain scales was significantly related to a belief that post-operative pain management in this patient group was sufficient. Intervention studies are needed in order to determine how acute pain assessment among patients with hip fracture and dementia could improve. A challenge for future research includes discovering the current situation of post-operative pain management from the viewpoint of older adults with dementia e.g. by reviewing medical records concerning pain management practices or observing or interviewing them, but it could be challenging due to deficits in verbal and cognitive capacities.
CONFLICT OF INTEREST
The authors declare no conflict of interest with respect to the authorship and/or publication of this article.
ABBREVIATIONS
| NRS | =Numeric Pain Rating Scale (0-10) |
| VRS | =Verbal Rating Scale (0=no pain, 1=slight pain, 2=moderate pain, 3=severe pain, and 4=unbearable pain) |
| VAS | =Visual Analogue Scale (0-10 cm) |
ACKNOWLEDGEMENTS
This study is financially supported by University of Eastern Finland and Finnish Foundation of Nursing Education.


