All published articles of this journal are available on ScienceDirect.
Living in the Presence of Death: An Integrative Literature Review of Relatives’ Important Existential Concerns when Caring for a Severely Ill Family Member
Abstract
Aim:
The aim of this study was to explore relatives’ existential concerns when caring for a seriously ill family member as well as to describe interventions that meet these concerns.
Methods:
In this integrative literature review we assessed and classified 17 papers, 12 qualitative and 5 quantitative. Literature was sought in the databases Cinahl, PubMed, Psykinfo and Web of Science in September 2009 and in March 2010. Search terms used in different combinations were: family, family caregiver, next of kin, relatives, palliative, palliative care, end-of-life care, existential, spirit*. Data were redrawn from the papers results/findings, and synthesized into a new descriptive content.
Results:
The results were categorized from 13 papers exploring relatives’ important existential concerns and 4 papers describing interventions aimed to support them in the existential area. A majority of the reviewed papers had been written in Sweden and concerned relatives of patients with cancer. One overarching theme, living in the presence of death, and three categories: responses to life close to death; support when death is near; and beyond the presence of death were created.
Conclusion:
There is an urgent demand for large-scale studies using accurate methodology, as well as a need to design qualified investigations regarding the effects of various interventions, and to determine which interventions are the most effective in supporting relatives who experience existential distress manifested physically and/or psychologically. There is also a considerable demand for educational interventions among professionals in various healthcare settings to increase their knowledge regarding existential concerns among relatives.
INTRODUCTION
In palliative care, relatives are often the primary care giver for persons with a serious illness. Their situation is difficult as they struggle with daily life while at the same time wanting to provide the best possible care. Relatives’ burdens increase as the seriously ill person proceeds from being quite active to becoming more and more bedridden. Care moves to other levels and new goals must be identified which may lead to feelings of aggravation and even burnout [1]. The future is unpredictable and relatives have to make difficult decisions’, often by themselves. Some relatives try to become as prepared as possible in this complex situationby searching for meaning, taking farewell and reaching religious and spiritual closure [2]. In this situation many relatives need support, but little is known about existing supportive interventions.
The importance of the patients’ existential concerns in end of life care was described by Cicely Saunders in the 1960:s when she introduced the term total pain, including the physical, psychological, social, and spiritual dimension [3], and became a part of the World Health Organizations’ definition of palliative care [4]. Existential needs are significant for patients with cancer, which is rather well described in literature [5]. Existential needs are described in other studies as people’s intense desire to infuse life and maintain a meaning in life [6-8], with freedom and relations [6], as well as sustaining purpose and hope [7, 8], and a desire to obtain feelings of peace [9]. The existential threats concern the loss of functions [10], control, social role functioning, continuity, relations, independency and the future [11, 12]. Saunders [3] emphasizes that meaninglessness is the essence of existential distress, and often concerns different losses. Other sources of distress are a changed personality and anxiety for death [10], dependency and feeling emotionally unrelated [13], or uncompleted life tasks and acceptance/preparation [11]. Living with cancer involves issues of transcendence, and spiritual well-being is improved by a person’s religion, sense of hopefulness, having a purpose in life, and other sources of spiritual support [7].
Relatives experience their situation as stressful and feelings of vulnerability are created when caring for a seriously ill family member. They want to be close to the ill person knowing that time is limited. It is also difficult being more aware about the situation than the ill family member, as is talking about death and dying in such a situation. Relatives often feel uninformed about the patient’s situation and lack guidance and support from healthcare professionals. Their needs differ from the patients as they are concerned that the care is not good enough for the patient while they are constantly by the patients’ side, struggling to prepare a situation that can differ from day to day [14]. Relatives also experience that they are quite unprepared for the suddenness of their role and the level of responsibility entailed in caring for a seriously ill family member. Furthermore, they felt inadequately prepared for the unpredictable nature of care giving and the timing of death [15]. Relatives’ role as the primary caregiver in caring for a seriously ill family member, who is facing death, may alert the relative’s own existential needs. They are in a vulnerable position and more information is required concerning what existential needs are actualized while facing the death of a close family member. Furthermore knowledge regarding the kind of interventions likely to be effective in meeting these complex needs is not earlier reviewed in the literature.
AIM
The aim of this study was to explore relatives’ existential concerns when caring for a seriously ill family member as well as to describe interventions that meet these concerns.
METHOD
In this integrative literature review 17 empirical studies were analyzed qualitatively. We assessed primary sources that described what alerts relatives’ existential emotions when caring for a person at the end of life, and the kind of support the relatives require in this vulnerable situation.
Literature was sought and found in the databases Cinahl, Pub Med, PsycInfo and Web of Science. No suitable paper was found in the Cochrane database. The search was restricted to adults, not child and peer reviewed and the language was English or Swedish (Fig. 1). When samples in the paper included patients, relatives or healthcare professionals text was extracted that described existential issues from the relative’s perspective. The initial search was performed in September 2009 and a complementary search was conducted in March 2010.
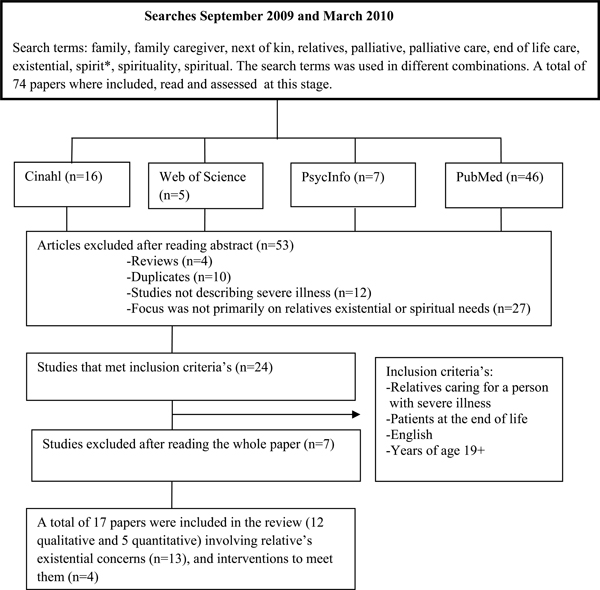
Overview of sampling procedure.
All authors were involved in the stages of the review process concerning:
- identifying the research questions and,
- searching literature. The literature was divided between the authors with the aim to evade that one of the authors reviewed papers written by herself.
- Papers that met inclusion criteria’s were read by all authors, and
- classified using a tool published by SBU [16]. Quantitative studies are divided in randomized controlled studies (RCT), clinical trials (CCT) and descriptive studies (DS) according to Goodman [17]. The studies were assessed according to sample size, well defined objectives, adequate described statistical methods and longitudinal studies. A qualitative study is when data are collected with interviews, narratives, or observations with the aim to get a deeper understanding of a person’s life world [16, 18]. The qualitative studies were assessed due to trustworthiness as well described research process, interpretations and conclusions. A scale was used when assessing the quality in included quantitative and qualitative studies, high (grade I) or low quality (grade III), a medium grade (II) were used if a study did not meet the criteria’s for grade I or III.
- The review process continued systematically by reapplying data from results/findings compiled in a spreadsheet,
- coding data and sorted item per item; similar data were grouped together,
- categorizing the content comparing them with each other concerning similarities and differences,
- and synthesizing data into a new descriptive content.
A total of 17 papers were included in this integrative literature review of which 12 were qualitative and 5 quantitative. An overview of the papers presented in the result is described in Table 1.
Overview of the Literature and Relation to Categories
| Authors and Country | Aim or Motivation for the Study | Design and Sample | Main Findings | Category | Grade of Classification K=Qualitative Studies (n=12) DS=Descriptive Studies (Quantitative n=5) Grade I= High Grade II= Medium Grade III= Low Quality |
|---|---|---|---|---|---|
| Adelbratt, Strang (2000) Sweden | To explore to what extent patients and their next of kin experience death anxiety, and how these experiences are expressed | Qualitative 20 patients with brain tumours and 15 next of kin Interviews were analyzed with content and context analysis | Six categories emerged concerning patients; (1) emotional reactions that could be related to death anxiety (2) existential fear (3) contradictions; (4) trigger situations (5) coping strategies (6) new values for life. Besides these categories, a further category emerged; experiences characteristic of the next of kin. | Response to life close to death | KI |
| Albinsson, Strang (2003) Sweden | To focus on issues of freedom/responsibility, existential isolation, death, and issues of meaning/meaninglessness. | Qualitative 20 family members of people with severe/ late stage dementia. In-depth interviews were analyzed with a hermeneutic approach. | To take responsibility was generally perceived as rewarding, but in some cases it was more a matter of duty with elements of guilt and obligation. Positive aspects of responsibility and the future involved passing on the patient's lifework. | Response to life close to death Beyond the presence of death | K II |
| Arnaert, Gabos et al. (2010) Canada | Relatives play a key role in the daily support and care of cancer patients. This role, however, can negatively affect relatives physically, psychologically, emotionally, and spiritually, challenging their health and well-being. Consequently, this could inhibit relatives abilities to continue in their roles as caregivers. | Qualitative intervention study 8 relatives of people diagnosed with cancer stage III and IV. Semi structured interviews to explore the experiences of attending a Skills for Healing Retreat Weekend. Analyzed with content analysis using the constant comparative method | Bringing people together to partake in discussions and activities fostered a sense of community among the participants. The retreat had enduring effects, contributing to relatives ongoing processes of healing as well as providing them with strategies for coping in their roles as caregivers. | Support when death is near | KII |
| Axelsson, Sjden (1998) Sweden | To gather knowledge about the quality of life both of terminally ill cancer patients and their spouses. | Quantitative Using Assessment of Quality of life at the End of Life (AQEL) 37 incurably ill cancer patients and their spouses, receiving support from a hospital-based palliative service | Spouses were more anxious than patients. The least-optimal items at the end of life for spouses were: ability to leave the patient unattended, need for assistance with hygiene/dressing and anxiety. Spouses found that meaningfulness was the item with the strongest correlation to global quality of life. | Response to life close to death Beyond the presence of death | DSII |
| Benzein,Saveman (2008) Sweden | To describe couples' experiences of participating in nurse-initiated health-promoting conversations about hope and suffering during home-based palliative care. | Qualitative intervention study 6 couples (6 spouses caring for a dying relative with cancer) participated in a health promotion conversation. Semi-structured interviews analyzed with its content. | Talking with nurses about existential issues such as hope and suffering made couples feel that they were part of a trustful relationship, and that it was a healing experience. | Support when death is near | K II |
| Cronfalk et al. (2009) Sweden | To explore relatives' experiences of receiving soft tissue massage as a support supplement while caring for a dying family member at home. | Qualitative intervention study 19 relatives of people who were dying or had severe illness. Semi-structured interviews analyzed with content analysis | Soft tissue massage gave a feeling of being cared for, energized the body and peace of mind. The overarching theme was 'inner power, physical strength and existential well-being in their daily lives'. | Support when death is near | K I |
| Hasson-Ohayon, Goldzweig et al. (2009) Israel | The current study examines the effect of perceived support from different agents (spouse, family, friends, religionspirituality) on psychological distress experienced by women with advanced breast cancer and their male spouses. | Quantitative 150 couples (women with advanced breast cancer and their spouses) completed the Cancer Perceived Agent of Support Questionnaire and the Brief Symptom Inventory Scale analyzed with descriptive statistics. | Spouses reported a lower level of support provided from family and friends. Spouses were more depressed and anxious than patients. Perceived support contributed significantly to the explanations of global psychological distress, depression and anxiety. Religious-based support was found to contribute negatively to the psychological distress.. | Response to life close to death Support when death is near | DSI |
| Hebert et al. (2008) USA | To determine what questions family caregivers want to discuss with health care providers (HCPs) in order to prepare for the death of a loved one. | Qualitative 33 current and bereaved caregivers of terminally ill patients (cancer, cardiovascular disease, COPD/pneumonia, cirrhosis, dementia, multiple illnesses). Ethnographic interviews and focus groups analyzed using standard methods. | Caregivers had a wide spectrum of questions to discuss with HPCs, and were medical, practical, psycho-social, or religious/spiritual in nature. Barriers to asking questions were feeling overwhelmed, "not knowing what to ask," the perception that HCPs were untrust-worthy, and worries about being perceived as "ignorant". | Support when death is near | KI |
| Hebert et al (2009) USA | To determine the factors that family caregivers believe are important to preparing for death and bereavement | Qualitative 33 family caregivers (bereaved or current) of terminally ill patients (cancer, cardiovascular disease, COPD/pneumonia, cirrhosis, dementia, multiple illness). Focus groups and ethnographic interviews analyzed using the constant comparative method. | Caregivers reported medical,practical, psychosocial, and religious/spiritual uncertainty. They often needed more than prognostic information in order to prepare for bereavement. Communication was used to manage uncertainty. Good communication included tangible, reliable information, combined with relationship-centered care from health care providers. | Support when death is near | KI |
| Lin,Tsao (2004) Taiwan | This study focuses on the terminally ill patients stay in a palliative care unit as a time to educate family caregivers and thereby improve the quality of continuing homecare after discharge. | Quantitative 137 caregivers of terminal cancer patients answered questionnaires (90, 65.7 analyzed with descriptive statistics. percent was completed) analyzed with descriptive statistics. | Information is needed among family caregivers who stay in the palliative care units to prepare them to provide hospice homecare after discharge. They needed specific information about the disease itself - this was highly important, less important was spiritual and religious information. | Response to life close to death Beyond the presence of death | DSI |
| Milberg, Strang (2003) Sweden | To describe and interpret the construct of meaningfulness in next of kin of cancer patients who are in advanced palliative homecare | Qualitative 19 next of kin of dying cancer patients. Interviews analyzed with a hermeneutic approach | Elements as retaining everyday life, commitment, hope, comfort and action, facilitated meaningfulness and were highly important for creating a perception of self-transcendence and for feeling that everything was done as well as possible | Response to life close to death | K II |
| Milberg et al. (2004) Sweden | To describe what characterize such experiences and the meaning of them to next of kin of cancer patients in advanced palliative home care and to make quantifications. | Quantitative Cross-sectional survey Text responses were analyzed with quantitative and qualitative content analysis 233 next of kin to diseased patients (response rate 72%) | Thirty-six percent of respondents stated that they had experienced powerlessness and/or helplessness every day or several times per week, during the palliative home care period. | Support when death is near | DSI |
| Rosenbaum et al. (2006) USA | To illuminate how existential factors may underlie some of the psychological benefits of family support, we explain one aspect of existential coping - symbolic immortality - and describe ways in which existential and social support factors work together during a Life Tape (LT). | Qualitative intervention study 35 patients with cancer and their families Videotaped interviews | Few interventions have been developed to help families support patients in dealing with fears of death and dying. The Life Tape Project (LTP) brings families closer together, increases communication, and acts as an existential intervention. | Response to life close to death | K III |
| Sand, Strang (2006) Sweden | To focus on the emotions, perceptions, and experiences of existential isolation in palliative patients with cancer and their families | Qualitative 20 patients (early or late palliative phase) and 20 family members Semi-structured interviews analyzed with existential hermeneutics | The data revealed experiences of existential loneliness with impending death as a primary source. Changes in one's own body and mood gave rise to feelings of loneliness. | Support when death is near | K I |
| Strang, Strang et al. (2001) Sweden | To describe the opinions of nurses, patients and next-of-kin on existential support and how this is prioritized. | Qualitative 20 patients with brain tumour (grade II-IV), 16 family members and 16 nurses Semi-structured interviews analyzed with phenomenography | Patients and family members were satisfied with the medical and physical treatment, but not with the existential support. | Support when death is near | K I |
| Syrn, Saveman et al. (2006) Sweden | To illuminate the way of being a family when one family member is in the midst of living and dying | Qualitative 5 families (N=48) each containing one family member with cancer. Narrative interviews were analyzed according to Giorgi | Dialectic and dynamic processes in constant motion within and between continually being in affinity-being in loneliness, being in power-being in helplessness, and being in continuity-being in disruption. | Response to life close to death Beyond the presence of death | K I |
| Tsigaroppoulos et al (2009) Greece | The aim was to survey and record the various problems faced by those who care for cancer patients at home. | Quantitative 76 family caregivers of people with terminal cancer The Problems and Needs in Palliative Care questionnaire- caregiver form (PNPC-c) was used analyzed with observational statistical methods | The most frequent problems were: anxiety regarding the patients future (61.8 %), troublesome symptoms such as pain (54 %), increased economic burden - financial difficulty (51.3 %), problems with patients feeding (50 %), unhappiness or depression (48.7 %), emotional upset (47.4 %), worsening of the patients behavior and personality (38.2 %), difficulty establishing a positive attitude regarding their current status (34.2%), transport to hospital (32.9 %), assistance from the wider family circle (25%). | Response to life close to death Beyond the presence of death | DS II |
RESULTS
The results from our literature review is divided into 13 qualitative studies exploring important existential concerns for relatives and 4 quantitative studies describing interventions aimed to support and guide relatives existentially. We did not find any interventions with randomized, controlled design. A total of 877 relatives, mainly spouses of patients with cancer were included in these studies. Seven studies included both patients and relatives, and one study included patients, relatives and nurses. An overview of the patients and relatives participating in the different papers are presented in Table 1. Ten papers were from Sweden, the rest were from USA (3), Canada (1), Israel (1), Taiwan (1) and Greece (1). When analyzing important existential concerns in the papers, one overarching theme, Living in the presence of death, 3 categories and 9 subcategories were created (Table 2).
Overview of the Overarching Theme, Categories, Subcategories and Papers Related to Each Sub-Category
| Overarching Theme Living in the Presence of Death | Data Analyzed | |
|---|---|---|
|
|
||
| Categories (n=4) | Subcategories (n=9) | Papers Related to Each Sub-Category (n=17) |
|
|
||
| Response to life close to death | Social decline | Adelbratt, Strang 2000, Milberg, Strang 2003, Milberg et al. 2004, Sand, Strang 2006, Hasson-Ohayon et al. 2009 |
| Physical expressions | Milberg et al. 2004, Sand,Strang 2006, Tsigaroppoulos et al. 2009 | |
|
|
||
| Psychological distress | Axelsson, Sjden 1998, Adelbratt, Strang 2000, Albinsson, Strang 2003, Hasson-Ohayon et al. 2009, Milberg et al. 2004, Sand, Strang 2006, Syrn et al. 2006, Tsigaroppoulos et al. 2009 | |
| Loneliness and insecurity | Albinsson, Strang 2003, Milberg et al. 2004, Syrn et al. 2006, Tsigaroppoulos et al. 2009 | |
| Responsibility and guilt | Adelbratt, Strang 2000, Albinsson, Strang 2003, Strang et al. 2004, Milberg et al. 2006 | |
|
|
||
| Support when death is near | Information and dialogue | Strang et al. 2001,Lin, Tsao 2004, Hebert et al. 2008, Hasson-Ohayon et al. 2009, Hebert et al. 2009 |
| Supportive interventions | Rosenbaum et al. 2006, Benzein, Saveman 2008, Cronfalk et al. 2009, Arnaert Gabos et al. 2010 | |
|
|
||
| Beyond the presence of death | Future hope and faith | Axelsson, Sjden 1998, Albinsson, Strang 2003, Syrn et al. 2006, Tsigaroppoulos et al. 2009 |
| A new dimension in life | Strang et al. 2001, Milberg et al. 2004, Sand, Strang 2006 | |
RESPONSES TO LIFE CLOSE TO DEATH
Social Decline
Relatives were often reminded of death e.g. due to the hospital environment [19], and the fact that they were about to lose their everyday life - i.e. normalcy was threatened [20]. Relatives of patients with brain tumors experienced that their partner just seemed to slip away; they lost their social life due to the patient’s changing personality [19]. This was a kind of social death. Relatives of patients with other malignancies no longer shared the same plans for the future or long-term life plans with their partners as they had done previously [21]. Thoughts of a common future with careers, grandchildren or retirement had to be abandoned, because they would not meet the future together. Some of the external fellowship they had shared with others ceased to exist, since the ill person no longer had the strength to socialize with friends outside the close family. The patient’s impaired function in daily life also restricted the ability to live a normal life, subsequently reducing autonomy and increasing loneliness [22]. Another study showed that spouses have significant lower levels of social support from friends and family compared with patients [23].
Physical Expressions
The patient’s physical suffering reminded relatives of death and they were worried about the patient’s poor symptom control and struggle to survive [22]. The relatives were always aware of the patient’s suffering, deteriorating health and declining strength. The relatives felt powerless in the face of the patient’s suffering, with physical symptoms, as pain, fatigue and breathlessness [21, 22]. The fact that the patient’s body began to fail and that the former physical strength was now lacking affected the relatives both emotionally and realistically [21]. Observing how the disease or treatment changed the body also contributed to relatives’ feelings of insufficiency [22]. Physical expressions in the patient were related to the relatives own physical reactions to the situation, such as muscle tension, headache, loss of appetite, and sleeplessness [24].
Psychological Distress
Death became real to relatives because they were constantly reminded of its presence. They lived with a continuous fear that the disease would deteriorate [19]. They suffered from psychosocial problems, such as depression and anxiety when the patient had “leave-takings” [22]. Relatives showed significantly higher levels of anxiety than patients [25], as well as higher levels of depression and overall psychological distress [23]. They had difficulties in expressing their emotions, such as depression and anxiety [24]. Feelings of insufficiency, powerlessness and helplessness were also experienced as the relatives felt that there was nothing else they could contribute with [21, 22]. Other experienced that they had come to terms with life, mortality and death. All this aroused feelings of awareness and reconciliation of life situation as well as overwhelming feelings of their failings and losses [26].
Loneliness and Insecurity
When patients suffering from dementia no longer could communicate, relatives experienced feelings of loneliness because they had no one to talk to [27], and consequently communication regarding life and death sometimes became difficult [26]. Relatives felt lonely when they had to take responsibility for all practical matters and they had feelings of isolation. It was not uncommon with experiences of existential loneliness in certain changes and circumstances during the disease trajectory [22]. Sometimes the situation was easier to endure when they were able to share their thoughts and feelings with the patient, which generated strength [26]. Other times the relative and the patient felt that they could not protect each other from suffering. The relatives were hovering between having experienced difficulties in the past and a readiness to manage the current life situation, as well as a need for the ability to use the necessary strengths and flexibility in daily life, learning to adapt to the situation in general. Sometimes they felt helpless, not having enough resources to manage the situation and found it difficult to know how to act in certain situations. Their trust in relations with healthcare staff was limited, the care provided was not helpful, and there was an unbalance between demands and expectations [26]. Feelings of anger directed towards the disease and healthcare staff were imminent [22].
Although relatives feared the occurrence of sudden adverse events, they strived to retain a positive attitude in their current situation [24].
Responsibility and Guilt
Reminded of the impending death relatives felt obligated to be faithful to their relation with the dying person, and that now was the time for them to repay all that they had previously received. Relatives were committed and involved in the care of the patient and did what they had to do without hesitation [20, 27]. Grown-up children to patients with severe or late stage dementia often felt like they had become a parent to their parent [27]. Other relatives of patients with cancer could feel that they were responsible for alleviating suffering and initiating healthcare staff to act [21]. They felt a responsibility to protect and distract the patient from negative feelings, but they sometimes experienced lack of resources to relieve suffering. The relatives could also feel “survivors’ guilt” about the disease and the situation to the dying person [19] and they felt guilty for not being able to do enough [22]. Other relatives found it difficult to express their emotions, for example sadness, but had no difficulty in expressing feelings of guilt [24].
SUPPORT WHEN DEATH IS NEAR
Information and Dialogue
The relatives wished for support from healthcare professionals in the form of a dialogue regarding chaos or information [28]. They expressed needs for medical, practical, psychosocial or religious/spiritual information when preparing for the death of the patient [29]. Relatives wanted healthcare staff to be present and needed confirmation from staff, i.e. they needed to be seen and acknowledged. Hindrance for providing support was staff’s lack of a holistic view, fear and lack of time [30]. Relatives want to discuss issues of a religious/spiritual nature with healthcare professionals such as for example the meaning of illness, or “Who can I speak to about religious/spiritual concerns?” or “Why is this happening?” and “Will my loved one go to heaven?” [31]. Spouses of patients with breast cancer reported that social support from patients, family and friends, as well as religious or belief-based support were extremely important and could quite well have a protective role concerning psychological distress [23].
Supportive Interventions
Four papers were found which described interventions aimed at helping relatives existentially. Two of them concerned conversations, which were assumed as being helpful. The first paper was a nursing intervention consisting of three health-promoting conversations with dying cancer patients and their spouses in palliative home care. The conversations had a salotugenic approach involving the couple’s recourses within and outside family as well as on health, hope and suffering encouraging them to reflect on their life situations. Talking about existential matters such as hope and suffering had a healing effect on participants. The couples experienced that they could unburden themselves and that they found new strategies for coping in daily life [32].
The second paper concerned life tape interviews with cancer patients and their relatives. The intervention consisted of 1-2 hour videotaped interviews in their home and an in-depth life story including family history, significant life events and personal philosophy. The patients had the chance to reflect on their lives and face issues of mortality in the presence of relatives. Patients and relatives shared the experience, which provided the patient with a feeling of not being forgotten after death. This provided the patient with a sense of symbolic immortality and the patient served as a role model to others in the family of how to face dying and death. It helped relatives to respond to their sense of helplessness and loss when a loved one is facing death. This may contribute to how they manage to handle the existential anxiety about their own mortality [33].
The third intervention concerned a nonresidential 2.5 days retreat weekend for cancer patients’ relatives. Various sessions were held during the retreat in which the participants shared stories with each other, the medical system was discussed, as well as the role of nutrition and complementary therapy. Sessions were also held about stress and relaxation response, and spirituality in cancer care as well as yoga, and group therapy. The relatives experienced emotional and spiritual healing that stemmed from a feeling of community with the other participants [34].
The fourth paper targeted relatives’ well-being through soft tissue massage, and one of the outcomes was existential well-being. Soft tissue massage, hand or foot, was given to relatives of patients in palliative care in their homes for 25 minutes once a day during a period of two weeks. Relatives perceived that they felt an inner power, strength and existential well-being in everyday life after the massage, despite worries, tiredness and their stressful situation. This reflects the psychological, physical and existential needs of relatives when caring for a severely ill or dying family member [35].
BEYOND THE PRESENCE OF DEATH
Future Hope and Faith
Hope, purpose in life and meaningfulness were also present in the situation in that the relatives tried to find the meaning of illness [25,27]. The current meaning concerned knowledge and daily routines, and good memories could constitute the meaning in the past. The meaning in the future concerned passing on skills and interest of the patient to the next generation [27]. Experiencing hope was also an issue of importance to the feeling of future meaningfulness, for example hope of patients’ improved well-being, which contributed to having something to look forward to [20]. Contacts with dead relatives and memories of them inspired confidence in eternal life, and spiritual power or a Christian faith was a source of hope. When awareness of mortality became obvious, the future became limited and short term goals were made only for the immediate future. It was difficult to find peace, and death was considered as disgusting [26]. Some relatives believed in God and their faith had not been affected due to the disease. Although church attendance was rare, a significant part of the relatives expressed that their faith had increased during illness [24]. In a study from Taiwan [36], it was found that relatives ranked spiritual issues as least important when caring for patients with cancer at the end of life.
A New Dimension in Life
Although living in the presence of death, relatives could sense a new dimension in life [28]. They perceived the patients’ suffering, fading away and felt insufficient. Powerlessness and helplessness contributed to a deeper meaning, including existential and social aspects, such as feelings of guilt, anger and loneliness [22]. Relatives stuck to frames of reference from a healthy life for a longer period of the course of the illness. Step by step the former united lives separated and the patients started to conclude their lives while the relatives began psychological preparations for a changed but ongoing existence [21].
DISCUSSION
Although there is an increased attention in research about existential needs significant for patients with cancer, our review demonstrated that the knowledge about existential concerns actualized among relatives facing the death of a close family member are limited. This could be due to that existential needs in general are ignored in palliative care because of the uncertainty over definition, lack of theoretical understanding, few documented interventions, and the lack of proper training and education for palliative care providers [37].
Our review showed that a majority of papers are qualitative, have small samples and are from Sweden. Only a few individual or group interventions were found with the specific focus on how relatives’ existential concerns were met. In another review it was described that a majority of family caregiver interventions are aimed to reduce stress levels, provide information and social support. A minority is designed particularly for family caregivers, and there is little evidence on the usefulness of these interventions in palliative care [38].
The lives of relatives living close to a severely ill person are influenced in many ways by the impending death. The awareness of living in the presence of death, while facing the death of a close family member i.e. mortality awareness, was a negative experience triggered by responses to life close to death. As for example social decline, physical expression manifested in different responses such as psychological distress, loneliness and insecurity, responsibility and guilt. In such a demanding situation relatives need professional and social support when perceiving a life beyond the presence of death. There are a variety of theories describing attitudes to death ranging from the strictly negative, which is rejecting death, towards attitudes of acceptance [39]. There is a pattern in our study that the relatives moved from the torment of watching their loved one fade away, constantly being reminded of death and responding to life close to death, through the illness trajectory towards a more “accepting” position.
Living in the presence of death was the overarching theme in our study concerning relatives who were constantly reminded of death that threatened their everyday life and normalcy. How they responded to this may be an expression of existential distress. Existential threats to normalcy may lead to fears of death which in itself may be embedded in anxiety for death. Fear has different meanings, for example the fear of being separated by death from your loved ones, or the finality of death (there is no more tomorrow) [39]. Existential distress may be an expression of death anxiety and the price one has to pay for living a genuine life [40] that is confronting ones fears as death, anxiety and uncertainty [41]. We found that relative’s death anxiety increased which may be manifested in existential loneliness i.e. despite being surrounded by friends; one is quite alone in the situation. Sand expresses this phenomenon as ”experiences of being alone in a world of one's own" [21].
Physical expressions in the patient were related to relatives own physical reactions to the situation, such as muscle tension, headache, loss of appetite, and sleeplessness. This is congruent with Merleau-Ponty who stated that people experience the world through their bodies can be seen as an object consisting of organs, bones, and flesh or a body as a subject, i.e. meaning is experienced from inside [42]. In a previous study [43] it was shown that a distressed body signals a message to the patient that death is approaching, and in the present study, we found that the same message is also conveyed to the relatives. Physical messages help the patients to prepare themselves for death, which is sometimes what patients want [44, 45]. Relatives own physical reactions may help them to prepare that death are imminent. Environmental messages in for example a hospital may remind the relatives of impending death, and hinder the feeling “at-home” [46]. The difference between the physical and the environmental reminders of death is that the physical reminders are inevitable. The deterioration of the body and the progress of the disease could be constrained but not totally stopped, but the hospital environment could be changed to become more welcoming and home-like.
Need of existential support was described in some papers in this review as well as opinions about how this could or ought to be provided by healthcare professionals. This is an implication for healthcare professionals to acknowledge and support relatives having existential needs, emphasize their vulnerable situation and existential distress. Nurses are of importance in providing spiritual support to relatives but are sometimes inadequately equipped to provide such support [47]. Spirituality in nursing is described as a multidimensional concept without any consensus about how it may be defined. Many nursing authors though include elements such as “transcendence, unfolding mystery, connectedness, meaning and purpose in life, higher power, and relationships”, and spirituality may or may not be related to religion [48]. In complex situations nurses may consider being guided by openheartedness, which is being grounded in the existential dimensions of being human. This is important, especially as care today is exceptionally technical and instrumental. It can be integrated in the interaction with a dying patient and the family by being close and not abandoning them, being open to their vulnerability without treating them as objects, using all technical recourses, specialized training and lived experiences. Nursing openheartedness is responsive to patients and families’ different needs from the very practical to the most existential [49].
Relatives want support from healthcare professionals in terms of information and dialogue. They need to be provided with adequate information about the disease as well as having someone to confide in and continually communicate with healthcare professionals. This may prevent and/or shed a light on possible conflict of interests, which was also found in another study of relatives of patients with amyotrophic lateral sclerosis (ALS) [50]. Staffs themselves perceive that they have a responsibility to provide existential support to cancer patients at the end of life. But there is a gap between the patient’s wish to discuss existential issues as healthcare staff lack strategies to meet them. This gap could be bridged by healthcare staff inviting them to a dialogue on existential issues [51]. There is a need to provide support groups, focusing on relatives’ existential distress and death anxiety, when caring for a seriously ill family member. Support groups are highly important to cancer patients and their families [52]. To participate would probably increase relatives’ feeling of security when living in the presence of death, and give them a sense of security in relation to the ill family member, the illness and nursing staff [53].
A new dimension was experienced by relatives, despite the situation being distressful. They experienced a glimpse of a new life following the period of illness. This indication was conveyed by relatives having positive feelings about future hope and faith. Hope has previously been found to be an essential resource in the lives of people with cancer helping them to cope during times of suffering and uncertainty. For relatives it was a gradual process of regaining strength and moving on [54, 55]. A new dimension in life could be the result of relative’s letting go of the ill person and may be a crucial turning point. “Letting go before death” attributes recognition of the fact that the loved one is dying and will die, acknowledging the impending physical and emotional loss that will occur at the time of death, and allowing the progression of inevitable death to occur by choosing not to prolong or impede this natural process [56]. After the death of loved a one, many relatives are in need of bereavement follow-up. They need to talk about the past, the present and the future, they need comfort in a situation of loneliness and there is a need to put words to emotions [57].
CONCLUSION
In this paper we present the fact that research concerning relatives’ existential concerns when caring for a seriously ill family member is limited. There is a need for large-scale studies with accurate methodology both qualitative and quantitative, mainly randomized controlled studies when investigating relatives’ existential concerns. Relatives living in the presence of death and being in a transitional phase need continual support from professionals, for example through dialogue. Relatives appeal for discussions relating to issues of an existential nature, such as “Why is this happening?” and stress the need for knowledge as well as strategies among healthcare professionals. Therefore educational interventions among professionals in different healthcare settings are needed, to extend knowledge about existential concerns among relatives. It is important that healthcare professionals understand the struggle relatives experience when living in the presence of death, and that they infuse future hope and faith through continuing dialogues, which may support the relatives in the transition into a new dimension in life.
CONFLICT OF INTEREST
There is no conflict of interest concerning this manuscript.
ACKNOWLEDGEMENT
To The Sahlgrenska Academy, University of Gothenburg, Sweden for funding this study and to Dorothy Björklund for linguistic revision.


