All published articles of this journal are available on ScienceDirect.
Nursing Research Priorities based on the Nurse-sensitive Indicators: Scoping Review
Abstract
Background:
Patient-centeredness, safety, and quality of care are major healthcare concerns worldwide. Clinical indicators are essential for monitoring and evaluating safety and quality of care within the health care system. Therefore, research on clinical indicators can improve the quality of care, promote good practices, clarify key concepts, and identify gaps vital to nursing care.
Objective:
The study aims to explore nurse-sensitive indicators to find significant research areas and prioritize them.
Design:
The study design is exploratory research conducted through scoping review, followed by Delphi consultation to identify nurse-sensitive indicators applicable in the Saudi Arabia health care system and prioritize these indicators as research areas.
Results:
The most frequently cited indicators are patient fall, medication error, patient satisfaction, catheter-associated infection, pain, pressure ulcer, the incidence of deep vein thrombosis or pulmonary embolism, appropriate levels of nursing skill mix, and nursing initial and need assessment. The result shows that (33) NSIs are essential to the quality of nursing care and patient safety in Saudi Arabia.
Conclusion:
Patient-centeredness, patient safety, a healthy work environment, and a nursing informatics system are significant research dimensions. We found that nurse satisfaction, patient satisfaction, pressure ulcers, patient falls, nurse-patient communication, patient engagement, and pain management are research priorities.
Recommendations:
Further studies must be conducted on NSIs that address patient-centeredness, safety, a healthy work environment, and a nursing informatics system. It can be observed that most of the studies focused on outcome indicators, and there is a need to study patient-reported indicators as a significant patient-centered concept.
1. INTRODUCTION
Nursing research is necessary to implement evidence-based practice and improve the quality of nursing research [1, 2]. Research priority-setting and gap analysis are the main steps in developing research strategies. Nursing research priority-setting assists nursing researchers and policymakers in targeting essential research areas [3].
Healthcare organizations have developed nurse-sensitive indicators (NSI) to measure the quality of nursing care and patient outcomes [4]. The American Nurses Association defines nursing-sensitive indicators as: “those indicators that capture care or its outcomes most affected by nursing care”. Nursing-sensitive indicators identify structures and processes affecting care outcomes. The effect of quality of nursing care on patient outcomes is not a new concept. Since the 1850s, Florence Nightingale has admitted the necessity of the quality of nursing care and measuring patient outcomes statistically [5]. In addition, nurses need to identify a set of indispensable indicators for monitoring their practices [6]. Therefore, nurse leaders must develop tools and collect reliable, consistent, and systematic information to assess the outcomes [6].
The National Database of Nursing Quality Indicators provides frequent reports of structure, process, and outcome indicators that evaluate nursing care in health care systems [7]. Measuring nursing-sensitive indicators helps guide quality improvement strategies [8]. There should be adequate research evidence on clinical effectiveness, safety, and efficiency based on indicators [8].
1.1. Problem Statement and Study Significance
The research significantly impacts nursing, practice, education, and health policy [9]. Therefore, nursing research must focus on effective and efficient nursing practice and factors affecting individuals, families, and communities well-being and healthcare services [10, 11]. Identifying gaps and setting research priorities based on clinical evidence and measurable indicators is considered the primary step in developing strategies that ensure the quality of nursing care and improve clinical practice and the quality of nursing research [2]. The emphasis on clinical indicators in nursing research will assure patients' safety, well-being, and risk reduction. Few published studies discussed the research priorities and nurse-sensitive clinical indicators as research areas. Therefore, this study aims to extensively explore nurse-sensitive indicators to find significant research areas and prioritize them and also highlight the vital areas for future patient-related nursing research that improve clinical practice, outcomes, and measurable indicators.
2. LITERATURE REVIEW
Nursing research is “a scientific process that validates and refines existing knowledge and generates new knowledge that directly and indirectly influences the delivery of evidence-based nursing” [9]. Nursing research enhances nursing leadership, cost-effective patient care, and quality outcomes in the nursing profession and the healthcare system [12, 13]. The nursing research journey started in the 1930s when Florence Nightingale developed studies to investigate patient morbidity, mortality, and nursing education. The development of evidence-based nursing practice has been of great concern in nursing research [9]. Evidence-based practice (EBP) aligns the best research evidence with clinical expertise, patient needs, and values.
The systematic reviews and meta-analyses conducted in nursing have been limited compared with other disciplines [9]. One of the most severe barriers to the EBP movement is the lack of research evidence regarding the effectiveness of nursing interventions [9, 14, 15]. Recognizing the areas lacking research is a significant step in developing the evidence needed for practice [9].
Research prioritization is a crucial part of the efforts required to strengthen health research systems [3]. In addition, the development of research priorities helps meet professional and practice needs [16]. Nursing research priority-setting processes assist researchers and policymakers in effectively targeting nursing research that has an optimal impact on public health [3]. The systems-based research priorities include quality and safety indicators, resource management, health systems structure and functioning, and patient safety [16]. For example, in the United States, nursing research priorities for emergency nursing have included staff-to-patient ratios, human resource management, emergency department overcrowding and patients waiting in the emergency department for hospital beds, and education strategies [17].
To evaluate the best practice and evidence-based practice, qualitative and quantitative measures are needed [6]. The development of the clinical indicators must be after reviewing adequate research evidence relevant to the quality of care [8]. These indicators based on research evidence can be helpful to guide research priorities setting in clinical nursing research. The American Nurses Association defines the clinical indicators sensitive to nurses as: “those indicators that capture care or its outcomes most affected by nursing care”.
The indicators are significant for the quality of nursing care in the hospital [4]. The impact of nursing care on patient outcomes is not a new concept. Since the 1850s, Florence Nightingale has admitted the necessity of the quality of nursing practice and evaluation and measuring patient outcomes through statistical methods [5]. Clinical indicators are an essential component of effective monitoring and evaluation of patient safety and quality within the health care system. Healthcare institutions seeking accreditation aim to provide patient-centered care through monitoring indicators [4].
The nurse-sensitive indicators measure patient-related outcomes affected by nursing care [5]. Based on the quality assessment framework, including structure, process, and outcome, the American Nurses Association has grounded its work on developing NSI on 'Donabedian's framework’ [5]. The characteristic of the structure is that the interventions conducted by nurses are a process of providing beneficial outcomes for their patients [6]. Therefore, it is challenging for the nurse manager to decide which data to measure and improve the quality of nursing care related to patient outcomes.
Nursing-sensitive indicators identify structures and processes affecting care outcomes [7]. Nursing-sensitive indicators are specific to nursing and differ from medical care quality indicators. The National Database of Nursing Quality Indicators TM (NDNQI®) provides quarterly and annual reporting of structure, process, and outcome indicators that evaluate nursing care in healthcare systems [7].
The use of NSI provides direction for nurse managers on measuring and improving nursing services and discussing the issues related to research on NSI. Most of the research on NSI is in acute care settings. A small number of studies have focused on specialist units, such as neonatal care, chronic hemodialysis, and intensive care [5, 18]. Standardized NSIs improve patient safety and workforce planning through enhanced knowledge that can help decision-making [18]. As nurse leaders, developing NSIs as standardized nursing data continues as a critical and expanding area of research to establish associations between nursing practice and patient outcomes.
Nurse leaders must use nursing reflection, evaluation, benchmark, and participation in research as one of their responsibilities [19]. The systems-based research priorities include quality and safety indicators, resource management, health systems structure and functioning, and patient safety [16]. Health organizations track up to 12-18 nursing-sensitive quality measures to provide significant insights based on structure, process, and outcome data [20]. For example, the National Quality Forum (NQF) from the United States suggested NSIs as “processes and outcomes and structural proxies for these processes and outcomes, e.g., skill mix, and nurse satisfaction, that are influenced by nurses but not exclusively responsible for them ” [21]. Nursing research/ evidence-based practice projects are one of the critical concepts of nursing shared governance [22-30]. Improved job satisfaction among nurses, improved patient outcomes, and other nursing-sensitive indicators, such as catheter-associated urinary tract infections, hospital-acquired pressure ulcers, falls with injuries, and central line-associated bloodstream infections, have the most significant clinical impacts when implementing shared governance structures and processes [30]. The National Institute of Nursing Research is one of the leading institutions in guiding nursing research and developing innovative questions for future research directions, such as promoting health, preventing illness, and self-management [31-33].
3. METHODOLOGY
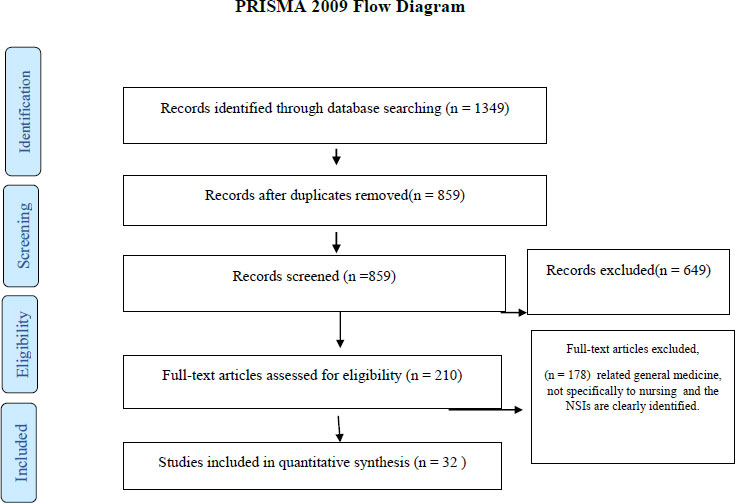
The study aims to explore nurse-sensitive indicators to find significant areas of research and prioritize them. The study design is exploratory research conducted through scoping review for electronic databases to identify key concepts and evidence with a broad approach to the scope or map topics. Scoping review method is typically systematic but without assessing the quality of included studies [22]. The Delphi Consultation was conducted to identify clinical indicators applicable in the Saudi Arabia health care system and prioritize them as research areas. The sampling technique is a purposive sample 41 participants. We used The PRISMA flow diagram in data collection through databases [23]. For eligibility criteria, we included the following types of papers:
- Papers discussing the clinical nursing indicators.
- Papers discussing the nursing-sensitive indicators.
- Papers discussing clinical nursing indicators and nurse-sensitive indicators in Saudi Arabia.
The comprehensive literature searches were performed from 1st January, 2021, until 31st March, 2021, in the following electronic databases: PubMed, CINAHL, Scopus, and the Nursing and allied health database. Search terms are as follows: “clinical nursing indicators” or “clinical nursing measures”, “nursing-sensitive indicators “or “nursing-clinical nursing,” “nursing-sensitive indicators or measures in Saudi Arabia,” “nursing clinical indicators or measures in Saudi Arabia.” All duplicated literature was removed after searching and eligibility screening. All study designs were considered eligible, including those that utilize qualitative or quantitative methods, methodology, or guideline reports. The study included 32 articles discussing NSIs and meeting the eligibility criteria.
Delphi consultation prioritized the research based on clinical nursing indicators conducted in two rounds. Round (1) identified the research themes important to nurses’ nursing clinical indicators based on review results. The experts were qualified nurses working in King Fahad Medical City in Riyadh, representing a tertiary health hospital accredited by national and international agencies. The total number of experts was 41 quality nurses working in different units. The survey included 106 NSIs summarized from the comprehensive literature reviews. In round (2), the research works identified in the round (1) were ranked and prioritized. Interviews were conducted individually with eight nursing research experts working within the general directorate of health affairs and the Ministry of Health. The list of NSIs, along with their dimensions, was explained and discussed during the interviews. The dimensions of research were based on a literature review, and four of them were selected based on expert consensus: patient-centeredness, patient safety, work environment, and informatics nursing.
3.1. Ethical Considerations
This research project was conducted following the ethical principles of the Declaration of Helsinki and the guidelines of the Research advisory council (RAC). The study provided anonymity of information collected; it did not collect any identifying or protected health information. The study was initiated after receiving the IRB approval (King Fahad Medical City IRB approval Log # 21-253E).
4. RESULTS
The scoping review was conducted within four selected databases (PubMed, CINAHL, Scopus, and Nursing and allied health database). The articles included in the review were 32, as presented in Tables 1 and 2. All included studies were related to nursing-sensitive indicators and (100%) nursing-related studies. When we reviewed the studies’ designs, it was found that 38% of the studies were literature reviews, and 19% used the Delphi technique. About 22% were cross-sectional surveys, and the same percentage was for quality improvement project-related studies. Furthermore, 6% of the studies were conducted in the Arab Gulf countries, and 84% were international studies. Finally, about 60% of the studies were conducted in the ICU setting, 15% in ambulatory care, and 25% in general units of the hospital.
| S.No. | Author | Aim | # NSI |
|---|---|---|---|
| 1 | Li et al. (2021) | Development and clinical application of nursing-sensitive indicators. | 33 |
| 2 | Stifter et al. (2021) | COVID-19 and Nurse-Sensitive Indicators. | 6 |
| 3 | Oner et al. (2021) | To provide a systematic review of the literature from 1997 to 2017 on nursing-sensitive indicators. | 20 |
| 4 | Evangelou et al. (2021) | To develop a set of potential quality indicators to quantify nursing care provided to critically ill patients through a consensus method. | 19 |
| 5 | Koch et al. (2020) | To identify indicators of nursing care performance by identifying structures, processes, and outcomes that are relevant, feasible, and have the potential for benchmarking in Swiss acute hospitals. | 21 |
| 6 | Connor et al. (2020) | To test the feasibility and performance of nurse-sensitive measures in pediatric cardiovascular programs. | 10 |
| 7 | Dufour et al. (2020) | To measure primary care nursing indicators using a wound care tracer condition. | 6 |
| 8 | McIntyre et al. (2020) | To identify hemodialysis nurse-sensitive indicators. | 26 |
| 9 | Afaneh et al. (2020) | This study aims to explore if there is a difference between the three groups of managers on the appropriateness of NSIs for monitoring nursing care quality in acute care settings. | 52 |
| 10 | Alharbi et al. (2020) | To examine the relationship between the level of compassion fatigue (CF) in critical care nurses and the rates of three nurse-sensitive indicators in Saudi Arabia. | 3 |
| 11 | Murphy et al. (2019) | To develop a suite of nursing quality care process metrics and indicators for older persons' care settings in Ireland. | 20 |
| 12 | De Carvalho et al. (2019) | To evaluate the quality of care provided in a maternal intensive care unit based on indicators of structure, process, and results. | 19 |
| 13 | Cantlin and Kronebusch (2019) | To expand NSI development, advise on modifications, and endorse measures to represent a nursing-sensitive point of view. | 6 |
| 14 | Myers, Pugh and Twigg (2018). | This review aimed to identify suitable indicators for measuring the impact of nurse staffing and nurse skill mix variations on patient outcomes in stand-alone high acuity areas. | 30 |
| 15 | Gao, Liu, Che and Xin (2018). | Construction of nursing-sensitive quality indicators for hemodialysis using the Delphi method. | 14 |
| 16 | Williams et al. (2018). | This study aimed to develop prioritized indicators of cancer patient experience for use in guiding service improvement. | 12 |
| S.No. | Author | Aim | NSI |
|---|---|---|---|
| 17 | Dubois et al. (2017) | Which priority indicators to use to evaluate nursing care performance? A discussion paper. | 25 |
| 18 | Chen et al. (2017) | To develop nursing-sensitive quality indicators consistent with current medical practices in Chinese neonatal intensive care units. | 11 |
| 19 | Wong et al. (2017). | Patient-focused outcome indicators listed in the Specialty (ICU) Guidelines | 14 |
| 20 | Pinto and Ferreira (2017) | to identify the main indicators for assessing the quality of nursing care from the perspective of nurses. | 16 |
| 21 | Wu et al. (2017) | to establish scientific, objective and comprehensive nursing-sensitive quality indicators for the OR to evaluate and monitor OR nursing care quality in China | 24 |
| 22 | Thomas-Hawkins et al. (2017) | Emphasizing the Value of Nephrology Nursing Through Nursing-Sensitive Indicators | 10 |
| 23 | Stalpers et al. (2017) | To identify nurses’ barriers and facilitators to monitoring of nurse-sensitive outcomes in intensive care units (ICUs), and to explore influential nurse characteristics and work environment factors. | 18 |
| 24 | Zhang et al. (2017) | To develop nursing-sensitive indicators for PICUs and to assess the quality of nursing in PICUs in China based on the nursing-sensitive indicators. | 13 |
| 25 | De Arruda Leitão et al. (2017) | to analyze the indexes of absenteeism and turnover, and their relationship with quality indicators in assistance | 4 |
| 26 | Twigg et al. (2016) | To develop a suite of nursing-sensitive outcome indicators for monitoring the safety of multi-day adult medical and surgical patients associated with nurse workloads and nursing workforce models. | 9 |
| 27 | Esposito et al. (2016) | patient’s engagement in their care | 1 |
| 28 | Mastal et al. (2016) | to set the stage for a series of articles to discuss the efforts the American Academy of Ambulatory Care Nursing (AAACN) has instituted to identify, define, and test nurse-sensitive indicators (NSIs) t | 7 |
| 29 | Stalpers et al. (2015) | review the literature on relationships between characteristics of the nurse work environment and five nurse-sensitive patient outcomes in hospitals. | 5 |
| 30 | Burston et al. (2014) | To review nurse-sensitive indicators that may be suitable to assess nursing care quality. | 43 |
| 31 | Wical et al. (2013) | to develop Nursing Sensitive Quality Indicators in the Perinatal Setting | 9 |
| 32 | Stevie et al. (2013) | To develop and define quality measures that are sensitive to obstetric nursing care and can be replicated across institutions. | 1 |
Table 1 provides the literature review of 16 articles that have discussed NSI from 2018 to 2021, as well as represents the numbers of NSI cited in each article and their study aim. Table 2 provides the literature review of 16 articles that have discussed NSI from 2013 to 2017, as well as details the numbers of NSI cited in each article, their study aim and research methods.
The review studies published between 2013 – 2021 cover nurse-sensitive indicators. Through a comprehensive review and combining similar NSIs, a total of 106 nurse-sensitive indicators met the review criteria. The researcher followed Donabedian’s (1988) framework in classifying the NSIs. Donabedian’s (1988) quality assessment framework includes structure, process, and outcome.
To answer the question of which NSIs effectively measure the quality of nursing care globally and locally, a comprehensive review was performed by screening all included studies that listed NSIs, collecting the result in one spreadsheet, removing duplication, and combining similar NSIs.
4.1. Nurse-sensitive Indicators Measuring the Quality of Nursing Care
The result showed that NSIs are used to measure the quality of nursing care. Patient falls, medication errors, patient satisfaction, catheter-associated infection, pain, and pressure ulcers are the most frequently cited indicators. The result showed the NSIs with low citations frequency include arrest/ shock rate, the incidence of deep vein thrombosis or pulmonary embolism, educational level, wound infection, working conditions (employment conditions, workload), adverse incident rates, appropriate levels of nursing skill mix, the incidence of complication, duration of care, and nursing initial and needs assessment.
Rare cited NSIs were reported in studies published between 2019-2021, such as puncture access monitoring, mechanical prophylaxis, self-dependence assessment, postoperative complications, absenteeism, work-related accidents, working conditions, patient empowerment, documentation, assessment of the patient’s fluid/hydration status, and rates of recorded needle dislodgement.
Table 3.
| S.No. | Nurse-sensitive Indicators | Applied (%) | Importance (%) |
| 1 | Appropriate levels of nursing skill mix | 98 | 100 |
| 2 | Pain assessment compliance rate | 98 | 100 |
| 3 | Record of vital signs and fluid intake/output at least four times daily. | 98 | 100 |
| 4 | Allergy history checking rate | 95 | 100 |
| 5 | Hand hygiene compliance | 95 | 100 |
| 6 | Nurse-patient communication and collaboration | 95 | 100 |
| 7 | Patient education compliance rate | 95 | 100 |
| 8 | Daily life care | 93 | 100 |
| 9 | Incidence of deep vein thrombosis or pulmonary embolism | 93 | 100 |
| 10 | Nurse satisfaction rate | 93 | 100 |
| 11 | Physical restraint | 90 | 100 |
| 12 | Patient hygiene and comfort | 98 | 98 |
| 13 | Patient satisfaction rate | 98 | 98 |
| 14 | Nursing care plan in all records | 95 | 98 |
| 15 | Patients’ identification rate | 93 | 98 |
| 16 | Patient involvement in the nursing care delivery process | 93 | 98 |
| 17 | Record of present admission | 93 | 98 |
| 18 | Wound infection | 93 | 98 |
| 19 | Clean environment (bed, fan, and furniture) | 90 | 98 |
| 20 | Self-dependence assessment | 90 | 98 |
| 21 | Comprehensive nursing care plan with patient-centeredness | 95 | 95 |
| 22 | Incidence of pressure ulcers | 95 | 95 |
| 23 | Patient falls | 95 | 95 |
| 24 | Incidence of catheter-associated urinary tract infections rate | 93 | 95 |
| 25 | Peripheral catheters were placed for no longer than 72 hours | 93 | 95 |
| 26 | Rate of errors in medication administration | 93 | 95 |
| 27 | Rates of infected vascular access (Rates of infected\ complications) | 93 | 95 |
| 28 | Responsiveness to patients ‘needs and expectations | 93 | 95 |
| 29 | Blood sugar regulation | 90 | 95 |
| 30 | Incidence of needle punctures among medical personnel | 90 | 95 |
| 31 | Record of physical examination performed by the nurse | 90 | 95 |
| 32 | Incidence of catheter-related bloodstream | 90 | 93 |
| 33 | Nursing initial and needs assessment | 90 | 93 |
| This table describes the percentage of agreement that these NSIs applied with a high level of importance. | |||
4.2. Nurse-sensitive Indicators Applicable in KSA
Table 3 describes the result of round I of the Delphi consultation. The survey was distributed to 41 nursing quality experts and patient safety in KFMC, including 106 NSI. According to the voting, 33 indicators got a high vote based on the application of indicators and the importance of the quality of nursing care and patient safety. The importance of NSIs depends on their impact on the quality of care, fulfilling strategic goals and maintaining patient safety [29].
Nurse-sensitive indicators that address the level of skill mix, pain assessment, patient hygiene, patient satisfaction, and vital signs documentation scored 98%, which is the highest percentage of agreement that these NSIs applied, indicating a high level of importance.
4.3. Research Domains based on Nurse-sensitive Indicators
The interview was conducted individually with eight experts in nursing research. The list of 33 NSIs, along with their dimensions, was explained and discussed during the interviews. The dimensions of research were based on a literature review, and four of them were selected based on expert consensus: patient-centeredness, patient safety, work environment, and informatics nursing. As reported in Table 4, four research dimensions were suggested: a healthy work environment, a nursing informatics system, patient safety, and patient-centeredness. The agreement percentage of nurse satisfaction among different areas of research was 100, patient satisfaction, pressure ulcers, patient falls, nurse-patient communication, and pain management was 88, and patient engagement was 75.
Table 4.
| Research Domain | NSI Name | Area of Research |
|---|---|---|
| Healthy work environment | Nurse satisfaction rate. | 100 |
| Incidence of needle punctures among medical personnel. | 75 | |
| Appropriate levels of nursing skill mix. | 38 | |
| Clean environment (bed, fan, and furniture). | 38 | |
| Nursing informatics system | Record of physical examination performed by the nurse. | 63 |
| Nursing care plan in all records. | 50 | |
| Record of vital signs and fluid intake/output at least four \daily. | 38 | |
| Record of present admission. | 13 | |
| Patient centeredness | Patient satisfaction rate. | 88 |
| Nurse - Patient communication and collaboration. | 88 | |
| Pain assessment compliance rate. | 88 | |
| Patient education compliance rate. | 75 | |
| Patient involvement in the nursing care delivery process. | 75 | |
| Responsiveness to patients ‘needs and expectations. | 63 | |
| Comprehensive nursing care plan with patient-centeredness. | 50 | |
| Patient hygiene and comfort. | 50 | |
| Nursing initial and needs assessment. | 38 | |
| Daily life care. | 25 | |
| Self-dependence assessment. | 13 | |
| Patient safety | Incidence of pressure ulcers. | 88 |
| Patient falls incidence with \without injury. | 88 | |
| Wound infection. | 75 | |
| Hand hygiene compliance (%). | 63 | |
| Incidence of catheter-related bloodstream infection. | 63 | |
| Incidence of deep vein thrombosis or pulmonary embolism. | 63 | |
| Peripheral catheters were placed for no longer than 72 hours. | 63 | |
| Rate of errors in medication administration. | 63 | |
| Rates of infected\ complications vascular access. | 63 | |
| Blood sugar regulation. | 50 | |
| Incidence of catheter-associated urinary tract infections rate. | 50 | |
| Patients’ identification rate. | 50 | |
| Allergy history checking rate. | 25 | |
| Physical restraint (). | 25 | |
| This table describes the research expert’s opinion on NSI as an area of research with the percentage of agreement. | ||
5. DISCUSSION
Based on the review, we prepared a comprehensive list of nursing-sensitive indicators that measure nursing care quality. The most frequently cited indicators were patient falls, medication error, patient satisfaction, catheter-associated infection, pain, pressure ulcer, arrest/ shock rate, incidence of deep vein thrombosis or pulmonary embolism, educational level, wound infection, working conditions (employment conditions, workload), adverse incident rates, appropriate levels of nursing skill mix, incidence of complication, duration of care, postoperative complications, and nursing initial and need assessment.
In terms of expertise at the advanced nursing level, the skill mix was reported to be a nurse-sensitive indicator applicable to KSA. The nursing profession’s development of competencies and skills should be studied more extensively [25]. In addition, professional issues, such as nurses’ skills and knowledge, are considered the most crucial research areas [27].
In terms of implementation, it is important to pay more attention to translating research evidence into clinical nursing practice [25]. Relevant studies focus on the following clinical areas: critical care, emergency nursing, mental health, oncology nursing, nephrology, medical-surgical nursing, as well as pediatric nursing [25]. In this study, in terms of the informatics system, the NSIs, such as initial nursing assessment, nursing care plan, and documentation, consider research topics. Researchers should use large health registers of data and patient-reported outcomes in nursing research because this data set analysis from the nursing perspective gives apparent consideration to patient interventions [25].
Patient-centeredness is a vital area that needs to study further. Based on the finding of this study, the NSIs can cover the following topics: patient satisfaction rate, patient involvement, nurse-patient communication and collaboration, patient education compliance rate, responsiveness to patients’ needs and expectations, self-dependence assessment, patient hygiene, and comfort in daily life care. It has been suggested that further studies will increase awareness and expand knowledge of evidence-based nursing care by addressing essential nursing areas, such as bathing and dressing, communication, mobility, nutrition, and patient self-management [26]. In addition, it is crucial to study pain assessment, management, and associated outcomes [26].
In terms of patient safety, the patient’s identification, the incidence of pressure ulcers, patient falls, medication errors, physical restraint, hand hygiene compliance, incidence of catheter-related bloodstream infection, the incidence of catheter-associated urinary tract infections rate, rates of infected vascular access, wound infection and incidence of deep vein thrombosis are clinical indicators and have an impact on the quality of patients care and outcome.
Reassessing these essential nursing activities will positively influence patient, nurse, and organizational outcomes [26]. However, some areas require more research from the nursing perspective, such as stroke, wound management, and pressure injury [25].
In terms of a healthy working environment, nurse job satisfaction and occupational health indicators are considered important research areas [27]. In general, it can be observed that most of the studies focused on outcome indicators, and there is a need to study patient-reported indicators as a significant patient-centered concept [28]. However, an association between the quality of nursing care provided and its direct impact on patient outcomes was reported in a study [29-32]. An improvement in nurse-sensitive indicators and patient outcomes measures was also observed after applying the nursing system framework that included the research as the main element [33].
CONCLUSION
The most frequently cited indicators were patient fall, medication error, patient satisfaction, catheter-associated infection, pain, pressure ulcer, arrest/ shock rate, incidence of deep vein thrombosis or pulmonary embolism, educational level, wound infection, working conditions, adverse incident rates, appropriate levels of nursing skill mix, incidence of complication, duration of care, postoperative complications, and nursing initial and need assessment. The nursing research experts suggested four research dimensions: healthy work environment, nursing informatics system, patient safety, and patient-centeredness. In general, it can be observed that most of the studies focused on outcome indicators, and there is a need to study patient-reported indicators as a significant patient-centered concept
LIMITATIONS
The possibility of missing some relevant studies attributed to database selection, gray literature, time constraints, and the exclusion of studies published in a language other than English; the numbers of evidence-based nursing research in Saudi Arabia are challenging. Also, the sampling technique involving the Delphi technique is a purposive sample that may introduce bias. It is a procedure that depends on the quality of the feedback provided, and the researcher’s analysis of the responses is a big responsibility.
LIST OF ABBREVIATIONS
| EBP | = Evidence-based practice |
| NQF | = National Quality Forum |
ETHICAL STATEMENT
This research project was conducted following the ethical principles of the Declaration of Helsinki and the guidelines of the Research advisory council (RAC). The study provided anonymity of information collected; it did not collect any identifying or protected health information. The study was initiated after receiving the IRB approval (King Fahad Medical City IRB approval Log # 21-253E).
CONSENT FOR PUBLICATION
Not applicable.
STANDARD OF REPORTING
PRISMA guidelines and methodology were followed.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article. Supplementary material is available on the publisher’s website along with the published article.


