Application of Evidence-based Practice in Intensive and Critical Care Nursing
Abstract
Background:
Evidence-based solutions are the main point of high-quality and patient-centered care. Studies analyzing the implementation of evidence-based nursing are an integral part of quality improvement. The study aims to analyze the application of evidence-based practice in intensive and critical care nursing.
Methods:
This research was performed in the Hospital of Lithuanian University of Health Sciences Kaunas Clinics in intensive care units (ICU) departments in 2019. 202 critical care nurses participated in this survey (response rate 94.3%)—method of research – anonymous questionnaire. Research object – implementing evidence-based nursing practice among nurses working in intensive care units. Research instrument – questionnaire composed by McEvoy et al. (2010) [1]. Statistical analysis was performed with SPSS 24.0 and MS Excel 2016 software. Descriptive statistics were used to analyse our sample and presented in percentages. Quantitive data are presented as mean with standard deviation (m±SD). Among exploratory groups, a p-value <0.05 was considered statistically significant.
Results:
Nurses with higher university education claim to know evidence-based nursing terminology better with a statistical significance (p= 0.001) and to have higher self-confidence in evidence application (p= 0.001) compared to nurses with professional or higher non-university education. It has been determined that age directly correlates with the implementation of evidence-based nursing: compared to their older colleagues, younger nurses have statistically significantly more knowledge (p= 0.001), skills (p= 0.012) and self-confidence when applying evidence (p= 0.001) as well as a more positive approach to evidence-based nursing (p= 0.041). Nurses whose total work experience exceeds 20 years have statistically significantly less knowledge of evidence-based practice terminology than nurses whose work experience is 10 years or less (p= 0.001). It has been determined that Intensive and Critical Care Nurses (ICU Nurses) with 10 years or less experience under their belt know the terms related to evidence-based nursing statistically significantly better (p= 0.001) and applies evidence-based knowledge in clinical practice more often, compared to nurses who have worked in the ICU for longer, e.g., 11-20 years or more than 20 years (p= 0.006). Compared to the nurses working in the ICU for 11-20 years, 10 years or less, those working for more than 20 years encounter statistically significantly more problems when applying an evidence-based approach in clinical practice (p=0.017).
Conclusion:
Younger nurses with higher education and less general work experience tend to have more knowledge and a more positive approach to evidence-based nursing. Problems with an evidence-based approach in clinical practice more often occur in nurses who have worked in the ICU for more than 20 years. Most of the nurses who participated in the study claimed that the lack of time was one of the key problems when practicing evidence-based nursing.
1. INTRODUCTION
In light of the changes in the health care system and the increasing expectations of society, the attitude towards nursing science and the limits of nursing competencies also change, increasing autonomy and advancement of the science of nursing [2]. Scientists return to the holistic approach to human health, evidence-based clinical solutions and treatment and nursing methods more and more often [3]. Evidence-based nursing is a fair application of an evidence-based approach in clinical practice and making decisions that ensure the highest quality of patient care [4]. Evidence-based practice forms a system of clinical solutions to problems and allows nurses to improve continuously and seek only the best professional results [5, 6]. Efficient and high-quality care and patient safety are the most important aspects that are ensured by applying evidence-based nursing practice [7].
ICU Nurses make many clinical decisions in their work. According to the researchers, ICU nurses must make clinical decisions every five seconds [8]. Thus, it is especially important to base those decisions on scientific evidence. Systematic application of evidence in intensive and critical care has undisputable benefits both to the nurses and to the patients. Nurses get a boost in work satisfaction, gain autonomy and have higher self-confidence in making decisions directly related to their patients' health conditions [9]. Meanwhile, the patients and their relatives know that all performed manipulations are safe and efficient, as proven by scientific studies, their hospitalization is shorter, mistakes are avoided, and the individual wishes and needs of patients are taken into account [10, 11]. Evidence-based nursing practice significantly contributes to avoiding common complications in ICU, such as respiratory tract infection and sepsis [12-14].
When introducing evidence-based nursing in an institution, the preparedness and attitude of employees are very important. Studies analyzing the knowledge, predisposition and skills of nurses and the obstacles they face in implementing advanced nursing practice are an important and integral part of the healthcare service improvement chain [15, 16]. Analysis of organizational barriers to applying evidence-based practice is also important [17]. Courses, simulations and seminars initiated by the workplace notably contribute to nurses' capability to apply evidence-based practice [18]. However, not all healthcare professionals apply the evidence-based practice. There are various reasons for that. For example, nurses are not interested in scientific innovations; they value work experience based more on traditions due to tight working schedules, willingness to learn, lack of knowledge or other factors [19]. Timely correction of obstacles to applying evidence-based practice may significantly improve the quality of healthcare services [20]. Aspects related to evidence-based nursing are not widely researched in Lithuania, unlike in other countries worldwide. This is why a study was carried out to analyze the application of evidence-based practice in intensive and critical care nursing.
2. MATERIALS AND METHODS
The study was carried out at the ICU of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital in 2019. The Center of Bioethics of the Lithuanian University of Health Sciences issued a permit to carry out the study after the presentation of the annotation and the research instrument. Targeted sampling was applied. The respondents were the nurses working at the ICU of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital. A total of 202 nurses were questioned, with a response rate of 94.3%. Research method: an anonymous questionnaire-based survey. Research object: applying the evidence-based practice in intensive and critical care nursing. A total of 20 questionnaire examples were given to the ICU Nurses before the study. The pilot study results revealed that the questions given in the questionnaire were understandable. The nurses gave no comments, and thus no corrections were made. The research instrument was the questionnaire prepared by McEvoy et al. (2010) [1]. Cronbach’s alpha of the questionnaire is 0,954. It shows reliability and high internal consistency. The questionnaire was used with the permission of the authors. The questions could be categorized as follows:
1. Demographic questions determined the respondents' age, gender, education, professional experience, work experience at the current institution and work positions.
2. The respondents had to rate evidence-based nursing-related statements and terms from 1 to 5 based on the Likert scale, where 1 meant total disagreement and 5 meant total agreement. Factor analysis helped to sort the 58 statements into 5 areas: importance, obstacles, terminology, practice and self-confidence.
2.1. Statistical Data Analysis
Statistical data analysis was conducted using the SPSS 24.0 (Statistical Package for the Social Sciences) software and MC Excel 2016. Descriptive statistics, i.e., absolute (n) and percentage (%) values, were applied to assess the distribution of the analyzed aspects in the sample. The quantitative data were presented as arithmetic means (m) with standard deviation (SD). The normalcy of the probability distribution of quantitative variables was assessed using the Kolmogorov–Smirnov test. The ANOVA test was used, the Fisher criterion (F) was calculated, and the Bonferroni adjustment was employed to compare the mean values of parametric variables of more than two independent samples. Tables of related aspects were made to assess the connections between aspects. The dependence of aspects was determined using the chi-square (χ2) test, and the pair comparisons were carried out via the z-test and Bonferroni adjustment. The Pearson correlation coefficient (r) was calculated to assess the strength of the aspect connection satisfying the normalcy assumption (r). In the case of 0<|r|≤0.3, the values were slightly dependent, in the case of 0.3<|r|≤0.8, the values were averagely dependent, and in the case of 0.8<|r|≤1, the values were strongly dependent [21]. The correlation coefficient was positive when a value increased with another value and negative when a value decreased with another value. Linear regression was used to assess variable dependence when the significance level was p<0.05, the difference of aspects in respondent groups was deemed statistically significant and when p<0.001, it was deemed highly statistically significant.
3. RESULTS
3.1. Knowledge and Attitude of Icu Nurses in Terms of Evidence-based Nursing
The study included comparing evidence-based nursing application areas based on the respondents' education. Nurses with higher university education claimed to know evidence-based nursing terminology better with a statistical significance than nurses with professional or higher non-university education. The research data also showed that nurses with higher university education had statistically significantly more self-confidence when applying scientific evidence than nurses with professional or higher non-university education. Detailed scores of evidence-based nursing application areas with standard deviations and their comparison are given in Table 1 below.
Linear regression was done to analyze the dependency of evidence-based nursing application areas on the age of the respondents. The results showed that all areas of evidence-based nursing application were statistically significantly dependent on the age of the respondents. Negative β coefficients in all four areas meant that as the age of the respondents increased, their agreement with the statements reflecting the analyzed areas decreased. Older nurses deemed evidence-based nursing to be less important than the younger ones. The terminology knowledge of older respondents was also poorer than that of their younger colleagues. Also, older nurses exhibited less evidence-based nursing-related practice and lower self-confidence (Table 2).
The application of evidence-based nursing in the ICU based on the work experience of the respondents was analyzed. The way the nurses with work experience in the ICU assessed evidence-based nursing areas was compared. It was determined that nurses who have worked in the ICU for 10 years or less knew the terminology related to evidence-based nursing statistically significantly better. Also, these nurses statistically significantly more often based their decisions in clinical practice on scientific evidence, compared to nurses who have worked in the ICU for longer, e.g., 11-20 years or over 20 years. Compared to respondents with over 20 years of work experience in the ICU, nurses with 10 years or less experience had statistically significantly high self-confidence in their knowledge and skills to apply evidence-based practice in nursing. Detailed information on the evidence-based nursing application area scores and standard deviations and their comparison with the work experience of the ICU Nurses are presented in Table 3.
| Education | Areas (maximum score), m±SD | |||
| Importance (70) | Terminology (85) | Practice (45) | Self-Confidence (55) | |
| Professional education (n=76) | 55.13±7.7 | 50.68±11.9 | 21±8.4 | 34.72±9.1 |
| Higher non-university education (n=52) | 56.19±7.5 | 54.42±12.8 | 23.46±9.1 | 36.79±8.2 |
| Higher education (n=74) | 57.55±8.1 | 62.92±11.2* | 23.93±7.9 | 40.57±7.7* |
| F (p) | 1.8 (0.167) | 20.4 (0.001) | 1.9 (0.152) | 9.3 (0.001) |
| Areas | Standardizedβ coefficient | p |
| Importance | -0.144 | 0.041 |
| Terminology | -0.270 | 0.001 |
| Practice | -0.177 | 0.012 |
| Self-Confidence | -0.226 | 0.001 |
| Work Experience in the ICU | Areas (maximum score), m±SD | |||
| Importance (70) | Terminology (85) | Practice (45) | Self-Confidence (55) | |
| ≤10 years (n=86) | 57.48±6.7 | 60.53±11.3* | 25.05±8.5* | 39.67±8.1 |
| 11-20 years (n=51) | 55.65±9.7 | 52.88±13.8 | 21.57±7.7 | 36.35±9.1 |
| >20 years (n=65) | 55.23±7.5 | 52.85±9.2 | 20.95±8.5 | 35.20±8.7** |
| F (p) | 1.8 (0.175) | 9.3 (0.001) | 5.3 (0.006) | 5.6 (0.004) |
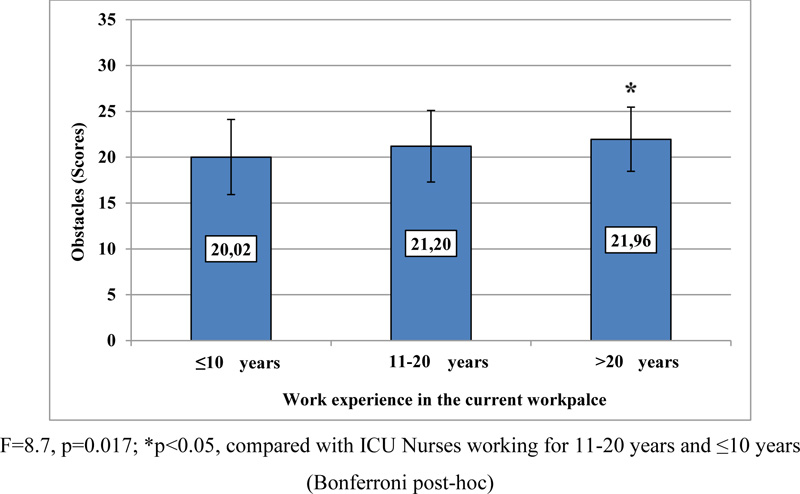
3.2. Obstacles That ICU Nurses Face When Applying Evidence-based Nursing
The comparison of the obstacles to evidence-based nursing based on the work experience of the nurses in the ICU was carried out. The maximum available score was 35. A statistically significant difference was found: compared to respondents who have worked for 11-20 years, 10 years or less, ICU Nurses with over 20 years of experience faced many obstacles when applying an evidence-based nursing approach. Thus, the longer the nurses work in the ICU, the more obstacles they face when applying an evidence-based nursing approach. Detailed information about the mean values of the scores and their comparison based on the work experience of the respondents in their current workplace is presented in Fig. (1).
3.3. Peculiarities Of Evidence-based Practice In Intensive And Critical Care Units Of Different Medical Fields
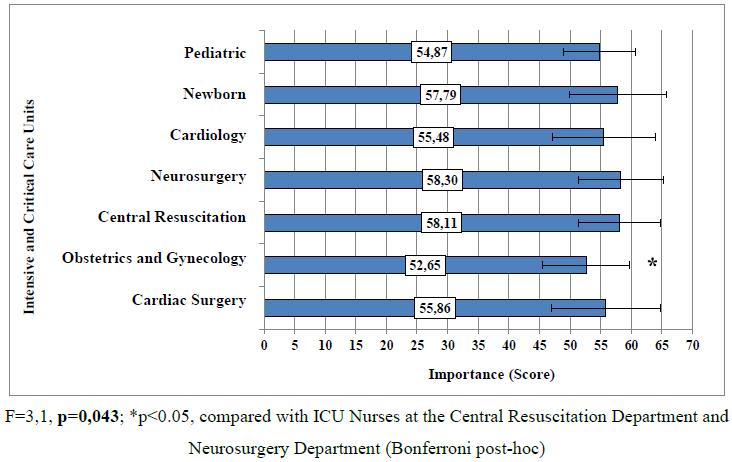
The study analyzed the peculiarities of applying the evidence-based practice in intensive and critical care units of different medical fields. It was determined that the ICU Nurses at the Department of Obstetrics and Gynecology considered evidence-based nursing to be less important than the Nurses working at the Central Resuscitation Department and the Neurosurgery Department. The difference was statistically significant. The importance of applying evidence in their work was rated highest by the ICU Nurses at the Neurosurgery Department and lowest by the ICU Nurses at the Department of Obstetrics and Gynecology. Detailed information about the importance of evidence-based nursing scores by the respondents from various departments and their comparison are presented in Fig. (2).
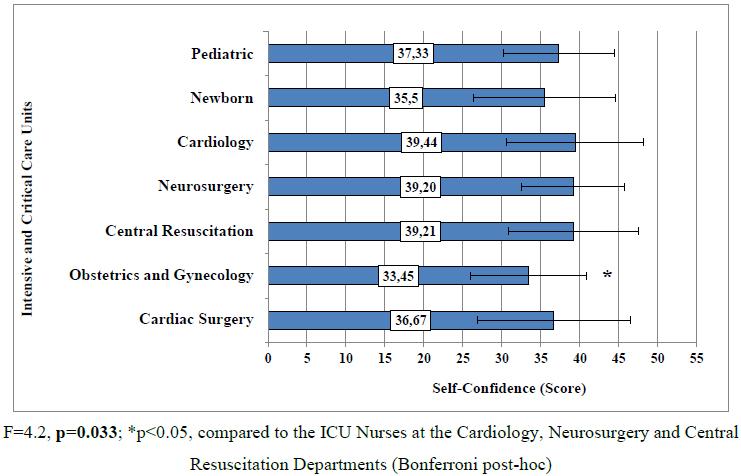
The study assessed the self-confidence of nurses when applying the evidence-based nursing approach and compared it among different departments. Self-confidence in evidence-based nursing and making evidence-based clinical decisions revealed statistically significant differences among the ICUs of the Obstetrics and Gynecology Department, Cardiology Department, Neurosurgery Department and Central Resuscitation Department. Compared to the nurses in other departments, the ICU Nurses in the Obstetrics and Gynecology Department had lower self-confidence when applying the evidence-based nursing approach (Fig. 3).
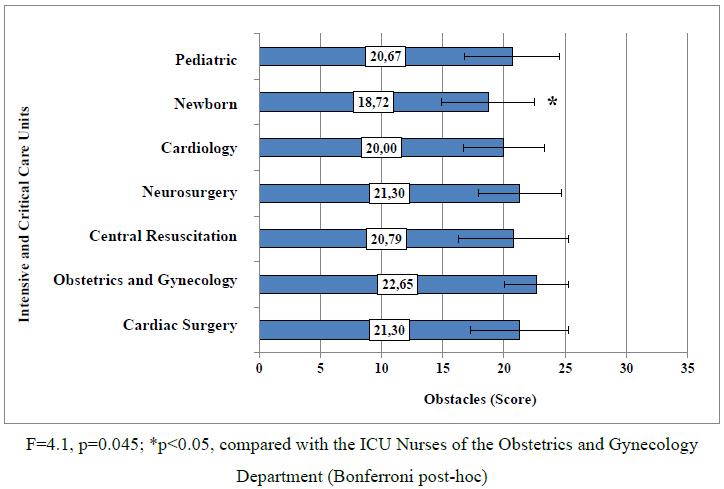
The study revealed that nurses applying the evidence-based approach faced certain barriers. The obstacles encountered in evidence-based nursing in the ICU of different medical fields were compared. The results revealed that the majority of problems in evidence-based nursing were experienced by the ICU Nurses of the Obstetrics and Gynecology Department. The Newborn ICU Nurses encountered the least problems. The difference was deemed statistically significant. Detailed information about the comparison of problems in evidence-based nursing based on the ICU profile is presented in Fig. (4).
4. DISCUSSION
The study analyzed the implementation of evidence-based nursing by the ICU Nurses at Kaunas Clinics in different aspects. The comparison of evidence-based nursing-related knowledge and attitude, the implementation of the evidence-based approach and self-confidence in its implementation was carried out in terms of the education of the respondents. The results revealed that nurses with higher university education had more knowledge and self-confidence when applying scientific evidence in clinical practice. Bovino et al. presented similar findings: according to their research of 2017, nurses with higher university education (bachelor’s or master’s degree) used evidence in their clinical practice more often and had higher self-confidence in their actions, compared to nurses with a lower level of education [22]. According to the study of Balakas et al. (2016), the implementation of evidence-based nursing was directly related to the education of the nurses, i.e., those with master’s or doctor’s degrees showed better results in formulating clinical questions, searching for the most reliable evidence and applying it in clinical practice [23]. Majid et al. research showed that nurses with higher education and participating in evidence-based training had fewer barriers to applying evidence-based practice [19]. According to Li et al., nurses with higher education and positions were more competent in applying evidence-based practice [24].
The age of the nurses also influenced the application of the evidence-based nursing approach. The study revealed that older nurses faced more obstacles when implementing evidence-based nursing. They had less knowledge and skills related to applying evidence in nursing. According to the study of Warren et al. (2016), younger nurses (22-29 years old) were statistically significantly better prepared to base their actions on evidence in clinical practice. Also, a statistically significantly higher number of younger nurses had a positive attitude toward evidence-based nursing and supported its importance [25].
Based on the opinion of many researchers, critical thinking is a key skill for ICU Nurses in making urgent clinical decisions, and the latter is integral to evidence-based practice. Ludin (2018) carried out a study with 113 ICU Nurses. It was determined that age and work experience in the ICU greatly affected the nurses' critical thinking and decision-making based on scientific evidence, e.g., older nurses with higher work experience had statistically significantly better skills in critical thinking and making clinical decisions [8]. Meanwhile, the results of this study were the opposite: the clinical decisions made by younger nurses with less work experience were more often based on scientific evidence. The research conducted by Alqahtani and co-authors (2022) showed that nurses working in the intensive care unit and emergency department have more knowledge about evidence-based practice than nurses from general units. Their research also concluded that nurses who participated in evidence-based practice courses had better attitudes, knowledge, and leadership skills than nurses who did not participate [26].
The attitude of the nurses is very important in an evidence-based approach in clinical practice. This study revealed that older nurses deemed evidence-based nursing less important than younger nurses. Nurses with higher education showed a more positive attitude to the application of scientific evidence in nursing: the statement ‘I have had enough of evidence-based nursing’ gained the agreement of 34.2% of nurses with professional education, 11.5% of nurses with higher non-university education, and 14.9% of nurses with higher university education. The difference is statistically significant. Based on the study by Swiss researchers Pereira et al. (2018), nurses with a more positive attitude towards evidence-based nursing usually base their clinical decisions on evidence statistically significantly more often [27]. The same trend was seen in this study: younger nurses, who, as mentioned previously, deemed evidence-based practice more important than older nurses, based their clinical decisions on scientific evidence statistically significantly more often. 507 nurses participated in a study by Degu and co-authors (2022). 55% of participants had a positive attitude toward evidence-based practice. Research showed that higher-education nurses had more knowledge about evidence-based practice, which led to a more positive attitude to evidence-based practice [28].
The research data revealed that certain barriers existed when implementing evidence-based nursing. Stavor et al. (2017) indicated that the main obstacles to applying an evidence-based approach in nursing were the avoidance of change, negative attitude and lack of time [29]. According to a study by Chinese scientists (2020), the lack of knowledge was the main problem in applying evidence-based nursing [30]. O’Connell et al. (2018) distinguished the two barriers: insufficient knowledge and the lack of cooperation between the nurses and the doctors [31]. In this study, more than half of the respondents (55.4%) said that the lack of time was one of the largest obstacles to implementing evidence-based nursing in clinical practice. The study also revealed that compared to younger nurses and nurses with less experience in intensive and critical care, older nurses and nurses with more work experience in the ICU encountered more problems when applying the evidence-based approach in nursing. Al-Lenjawi et al. conducted a study with 278 nurses from ICU. The research revealed that the main barriers to applying evidence-based practice are lack of time and support from colleagues, inability to understand statistics, and negative attitude to evidence-based practice [32]. The mentorship program is one method to encourage nurses to use evidence-based practice. Nurses gained more knowledge and a more positive attitude; there were fewer obstacles to applying evidence-based practice after the mentorship program [33]. Following Patelarou et al., evidence-based practice training strongly contributes to more effective healthcare and should be the priority in establishing nursing education programs [34]. The benefits of evidence-based practice training were emphasized by Ruppel et al. based on the data of their study – nurses with a positive attitude towards evidence-based practice still indicated that training is necessary due to a lack of knowledge [35].
Thus, critical thinking, a holistic approach to a patient’s health condition, and the ability to work and plan patient care in a multidisciplinary team based on the most trustworthy scientific evidence for each individual case should be the daily duties and responsibilities of each nurse. Studies analyzing the implementation of evidence-based practice are important in attaining the best results in nursing and its practice [36]. Most of this study's results comply with the studies of foreign researchers. Younger nurses with higher education have better knowledge of applying evidence-based practice in nursing and have a more positive attitude toward it. Nurses with a lower level of education, and in this study, older nurses encounter more problems when applying evidence in clinical practice. The main obstacles to implementing evidence-based nursing are the lack of time, resources and knowledge.
CONCLUSION
1. The knowledge and attitude of the ICU Nurses related to evidence-based nursing and the implementation of this approach depend on such factors as education, age and work experience. Younger nurses with higher education and less work experience in the ICU tend to have more knowledge of evidence-based nursing and a more positive attitude toward it.
2. Older nurses and nurses whose work experience in the ICU is over 20 years encounter problems when applying scientific evidence in clinical practice more often. Most of the respondents believe the lack of time is one of the major obstacles to implementing evidence-based nursing in clinical practice.
3. The comparison of the peculiarities of employing evidence-based nursing in the ICUs of different medical fields revealed that the ICU Nurses of the Obstetrics and Gynecology Department deemed evidence-based nursing to be less important and thus had lower self-confidence and encountered more problems when applying an evidence-based approach in nursing.
LIST OF ABBREVIATIONS
| ICU | = Intensive Care Units |
| SD | = Standard Deviation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Center of Bioethics of the Lithuanian University of Health Sciences issued a permit to carry out the study after the presentation of the annotation and the research instrument (the approval number BEC-ISP(M)-14). Participants submitted informed consent.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were per the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study was funded by Lithuanian University of Health Sciences Kaunas Clinics Department of Cardiac, Thoracic and Vascular Surgery.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We would like to thank the ICU Nurses of Kaunas Clinics of the Lithuanian University of Health Sciences Hospital, who have consented to participate in the study.


