All published articles of this journal are available on ScienceDirect.
Towards Safe Patient Identification Practices: the Development of a Conceptual Framework from the Findings of a Ph.D. Project
Abstract
Patient identification errors are considered the root cause of other patient safety incidents. Despite the development, recommendation, and application of several initiatives to reduce and prevent misidentification in hospital settings, errors continue to occur. They directly impact the quality of care provided, resulting in delays in care, added costs, unnecessary injuries, misdiagnosis or wrong treatment, and other serious and irreversible types of harm and death. Furthermore, the certainty of the evidence of the effectiveness of interventions to reduce patient identification errors is considered very low.
This paper reports on the development of a conceptual framework for safe practices in the area of patient identification. The proposed conceptual framework was developed based on presuppositions regarding learning health systems and the available evidence from the published systematic reviews of the effectiveness of interventions in reducing patient identification errors in hospital settings. The core circle of the framework represents the partnership between managers, healthcare professionals, patients, and families working toward integrative and collaborative efforts for safe patient identification practices. The inner dimension states the recommendations for practice sustained by applying technological resources and educational strategies to raise awareness of the importance of accurate patient identification and interdisciplinarity, which works as an axis that supports integrated and collective work between healthcare professionals aiming for safe care. The outer dimension represents recommendations for teaching and research to develop effective patient identification practices that can enhance patient safety and the quality of care provided in hospital settings.
This framework provides a valuable method for engaging interdisciplinary teams to improve the safety of patient identification systems.
1. INTRODUCTION
Patient safety has become one of the main focuses of healthcare organisations worldwide over the last two decades. The production, dissemination, and implementation of policies, strategies, and procedures have been adapted to reduce errors and ensure the safety and quality of the delivery of care. However, failures continue to occur despite the initiatives undertaken over the past twenty years. Therefore, it is highly recommended that health organisations foster a consistent safety culture with an integrated approach to managing adverse events [1, 2].
For this integration to be effective, the learning health system (LHS) advocates for the need for alignment between science, information technology (IT), and organisational culture to ensure continuous quality and innovation through the implementation of best practices and new knowledge acquired across the experience derived from the care process [3]. The LHS was designed to guide the generation and application of evidence in providing collaborative, safe, and high-quality care that adds value to healthcare institutions [3, 4].
This collaboration must arise from the exchange of knowledge and evidence across various healthcare settings and types of care [2, 5]. The lack of integration between health services and suboptimal regulation in the private sector causes fragmentation, redundancy, and significant care failures [5, 6]. In several areas, evidence-based tools and strategies to improve patient safety have not yet been fully translated into practice, especially in terms of patient identification [7].
Patient identification errors affect healthcare delivery and are considered the root cause of several other types of incidents [1]. Such mistakes can result in surgeries or procedures being performed on the wrong patient, errors in the administration of medication and blood components, cancellations of examinations, delays in diagnosis, and breastfeeding of the wrong baby, among other issues [8-10].
Global interventions have been implemented to ensure correct and safe patient identification. The World Health Organization (WHO) recommends using standardised ID bands with at least two identifiers to verify the patient’s identity, which may include information such as name and date of birth, on admission; before transfer; and before care, treatments, or procedures administered [10]. In addition, the WHO suggests implementing IT and enhancing health professionals' education about identification protocols and promoting the awareness of service users and family members about the importance of correct patient identification and the use of patients’ wristbands [11]. The Joint Commission International (JCI) patient safety goals have patient identification as their first recommendation for safe practices and stress the need for a reliable identification system to prevent errors [12].
Several studies have illustrated the implementation of strategies to increase the safety of patient identification in hospital settings. A range of IT resources have been widely implemented, such as biometric identification systems, radio frequency identification devices, and barcode technology, to assist in the various stages of the patient identification process [13-15]. Educational strategies such as auditing, providing feedback, and holding training sessions have been employed to optimise staff’s adherence to safe practices and increase their awareness of the need to use the correct data to verify patients’ identities and ensure the correct use of identification bands [16, 17].
Despite the development of recommendations for, and applications of, these interventions, a literature review identified 7,613 incidents related to patient identification in 181 healthcare organisations worldwide [18]. The JCI reported 36 sentinel events between 2018 and 2020 associated with surgical and invasive procedures performed on the wrong patient [19]. Additionally, findings from the only systematic review of effectiveness published in this journal have added a level of uncertainty regarding the effectiveness of educational and technological interventions in reducing patient identification errors in hospital settings and the overall quality of evidence was considered very low [20].
The review included 12 articles published between 2002 and 2017 which were conducted in several adults, paediatric, and neonatal areas, such as inpatient wards, emergency services settings, operating rooms, and intensive care units [20]. The sample types were heterogeneous among the studies and included patients, ID bands, electronic orders, and medication rounds [20].
The review demonstrated that staff education about using correct patient identifiers when applied as a single intervention or combined with an IT resource may significantly reduce patient ID bands and patient bedside identity check errors. However, the level of evidence regarding this vital strategy was very low [20]. These findings resulted from six studies [21-26] that demonstrated imprecision, inconsistency, and indirectness. Moreover, the heterogeneity of the populations and interventions precluded a meta-analysis [20]. One single-group pre-post study [27] involved staff and patients in the identification process provided them with education to raise awareness of the importance of correct patient identification and the need to keep patients’ wristbands at all times. Despite the effectiveness of the intervention in reducing patient ID band errors, this analysis was limited to only one study.
Similarly, the use of healthcare IT methods such as barcodes, electronic prescribing, electronic health records, and computerised physician order entry which may be an essential resource for reducing patient identification errors and supporting the safety of the patient identification process, was demonstrated in the review [20]. However, this evidence came from five studies [28-32] that presented considerable methodological limitations, such as, for instance, a lack of control groups and varied populations, which also made meta-analysis unfeasible. Therefore, the results were insufficient to support decision-making regarding these interventions [20].
The findings highlighted above, combined with the authors’ experiences acquired during the doctoral course and the presuppositions of the LHS, which incorporates a continuous cycle of systematic improvement of services by combining the production and application of evidence to the provision of healthcare [33], resulted in the creation of a conceptual framework for safe patient identification practices (Fig. 1). The proposed framework was developed from a synthesis of the reviewed articles and the recommendations for practice and research of the published review, and it provides a valuable structure to identify the relevant dimensions and indicate the components’ relationships with each other.
This framework aids in the generation of a profile for patient identification in terms of relative strengths and challenges that may be used to provide focus to improvement strategies for patient identification in hospital settings. The core circle represents the need to generate and apply the best evidence for fostering a patient safety culture that engages managers, healthcare professionals, patients, and families in integrative and collaborative work to enhance safe patient identification practices.
The structure also has inner and outer dimensions that influence the safety of patient identification processes. The inner dimension is divided into two layers. The first layer includes the application of educational and technological resources. Innovative educational strategies are essential for raising awareness of the importance of patient identification for staff, patients, and their families, with everyone playing a key role in the identification process. Furthermore, tested and validated IT resources, such as barcode readers and secure computer systems for ordering and documenting items, should be implemented based on organisations’ realities and priorities. These tools can be more effective when combined with initiatives that educate professionals on the risks of patient misidentification and improve compliance with safe patient identification practices [34]. Nurses need to be informed about the patient safety culture and managers must guarantee the implementation of comprehensive patient identification protocols from hospital admission to discharge.
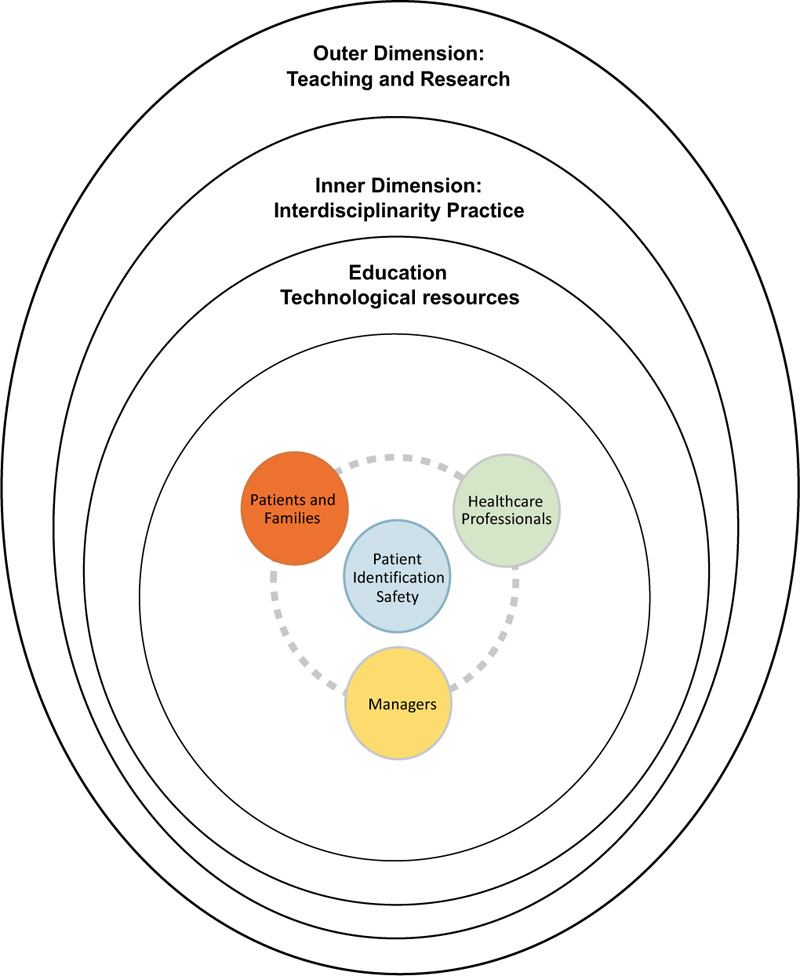
The second layer is the interdisciplinarity that permeates and influences the core circle and outer dimension. It works as an axis that supports integrated and collective work between various healthcare professionals in search of the construction and expansion of knowledge for shared interventions to mitigate patient identification errors and improve health outcomes [36, 37].
The outer dimension includes the relevance of teaching and research in developing a patient safety culture. It is paramount to introduce evidence-based and interdisciplinary teaching interventions throughout the academic pathway of healthcare students at all levels and in all disciplines to provide knowledge and cultivate the required skills, behaviours, and attitudes necessary for providing safe care [38-40]. From this perspective, it is recommended that patient identification be highlighted as the initial part of patient safety in various care processes.
Research with more robust methodologies is recommended to clarify the real impact of interventions to reduce patient identification errors [18, 20]. Furthermore, additional studies are needed to understand the effectiveness of educational strategies to improve professional practices and encourage family members and patients to act as partners in care with the aim of improving the quality of the patient identification process [20, 41]. Research is also suggested to assess the safety, efficacy, and cost-effectiveness of technologies that help reduce patient identification errors [10, 14, 20]. Lastly, qualitative studies exploring the perceptions of service users, health professionals, and managers in preventing and reducing patient identification errors could contribute to this body of evidence [20, 42].
CONCLUSION
To conclude, this paper contributes to the knowledge and integrates key meaningful dimensions for patient identification safety under a single conceptual framework. It stresses the recommendations for practice, teaching, and research to promote safe patient identification systems in hospital settings. The core circle of the model symbolises managers, staff, and service users’ collaboration and engagement in ensuring correct patient identification. The internal layer of the inner dimension includes recommendations for practice that can be attained by applying educational and technological resources to aid in promoting safer patient identification practices. The external layer reiterates the importance of multidisciplinary work to guarantee correct patient identification in all the care processes. The outer dimension includes recommendations for teaching and research focused on patient identification. Further studies will be required to measure the dimensions of this framework, evaluate their effect, and determine how they can be operationalised in practice. This will assist nurses and other healthcare professionals in a more cohesive engagement in multidisciplinary efforts to enhance patient safety culture and the quality of patient identification processes in hospital settings.
LIST OF ABBREVIATION
| LHS | = Learning Health System |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


