All published articles of this journal are available on ScienceDirect.
Effects of the COVID-19 Pandemic on the Mental Health of Pregnant and Puerperal Women: A Systematic Review
Abstract
Background:
The Coronavirus Disease 2019 (COVID-19) pandemic has caused negative impacts on the physical and mental health of the population worldwide. Pregnant and puerperal women comprise the population most vulnerable to impacts on mental health.
Objective:
To synthesize the scientific evidence on the effects of the COVID-19 pandemic on the mental health of pregnant and puerperal women.
Methods:
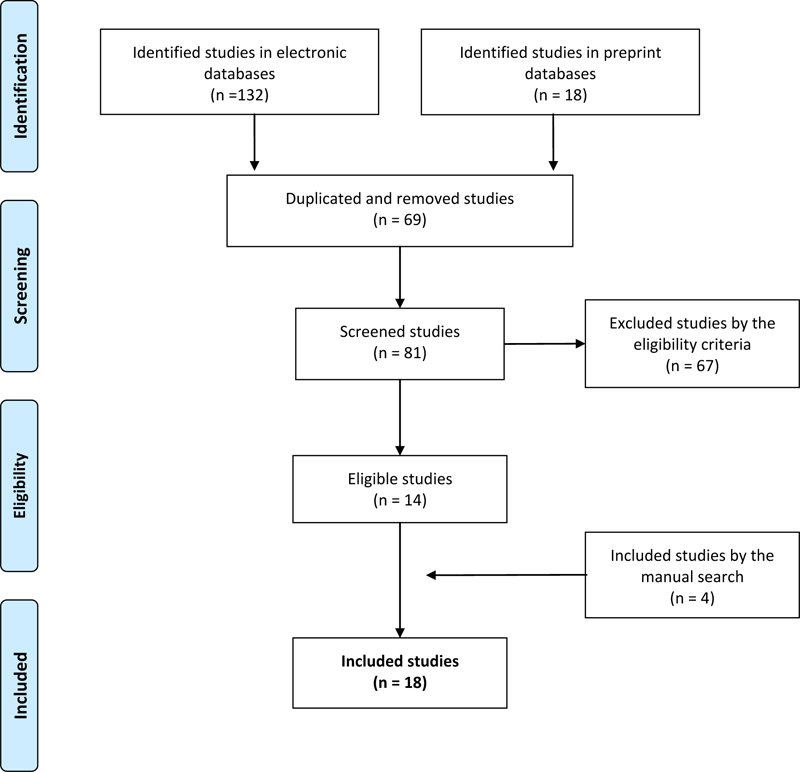
This systematic review focused on answering the question “what is the impact of the COVID-19 pandemic on the mental health of pregnant and puerperal women?” In order to perform the search of the studies, we used combinations of keywords: pregnant, puerperal, prenatal, perinatal, mental health, COVID-19, SARS-CoV-2. We identified 132 studies from the databases and 18 studies from preprints. In total, we elected 14 studies and another four studies by manual search, making up a total of 18 studies, to compose the final sample of this review.
Results:
Anxiety and depression were the main outcomes found, being shown in 15 and 11 studies, respectively. Other outcomes found in more than one study were: concerns related to several factors, loneliness, stress, and fear.
Conclusion:
From this review, we can infer that the COVID-19 pandemic has impacted the mental health of pregnant and puerperal women, with depression and anxiety being the most frequent changes. The social detachment, the media pressure, the fear of contracting the infection, the economic scenario, and the rupture of family rituals are shown as intensifying factors of psychological distress, thus causing changes in the mental health of these women.
1. INTRODUCTION
The onset of emerging infectious diseases has been considered a major public health problem worldwide. Atypical cases of pneumonia, severe respiratory disease, and sudden impairment of other organs appeared in the city of Wuhan, Hubei province, China, in December 2019, caused by Severe Acute Respiratory Syndrome Coronavirus 2, SARS-CoV-2, aetiological agent of Coronavirus Disease 2019 (COVID-19) [1].
With the exponential growth of COVID-19 on a transcontinental basis, the World Health Organization (WHO) declared, on March 11th, 2020, that COVID-19 qualified as a pandemic. Although the disease has low lethality, which ranges from 0.2% to 14.8%, its worsening is associated with an increase in the age group and the clinical impairment of pre-existing diseases. Its transmissibility is high, reaching about 80% of mild cases of the acute respiratory syndrome, where between 5% and 10% of cases progress to severe symptoms of respiratory failure [2]. Respiratory secretions are the main source of the spread of COVID-19 [3]. Moreover, COVID-19 is capable of causing neurological, hepatic, respiratory and enteric changes [4].
Since the WHO declaration, health agencies have adopted measures to protect and prevent the spread of the illness, such as social detachment, the use of personal protective equipment (PPE), and non-pharmaceutical strategies, such as hand washing [5]. The adoption of prevention and control measures are part of the strategic actions aimed at the population or groups with a higher risk of infection, and the adoption of measures to halt the spread of the virus has caused an impact on health results, mainly on the mental health of the population, especially pregnant and puerperal women [6].
Women in gestational and puerperal periods are groups considered to be at risk, given the greater chances for serious complications and lethality [7]. Accordingly, the primary and hospital health care services adopted the reorganization of care flows and specific strategies for the clinical-care management of these women, aiming at reducing the number of cases of COVID-19. In view of the above, the assistance during childbirth, birth, and follow-up of the parturient woman must comply with all technical recommendations in symptomatic, asymptomatic, or positive cases for COVID-19, aiming at protecting the health of women and newborns [8].
The rapid spread, lack of discovery of effective treatment, the unpredictability of the duration of the pandemic, the disclosure of false information, known as fake news, and the shortage of understanding of the population in complying with the recommendations of health authorities are characterized as risk factors for the impact on mental health [9].
The increase in fake news published on social media has also increased stress, fear and anxiety about the disease since the way some information is exposed has generated negative consequences on the mental health of the population, in some moments of this pandemic, especially in women during gestational and puerperal periods [10].
In view of the pandemic scenario, the disclosure of scientific knowledge worldwide has been happening in a skillful way about information concerning COVID-19. Nevertheless, studies associated with the impact of the pandemic on the mental health of pregnant and puerperal women are scarce, as the event is recent, but highlights negative factors. Thus, this study had the objective of synthesizing the scientific evidence on the effects of the COVID-19 pandemic on the mental health of pregnant and puerperal women.
2. METHOD
It is a systematic literature review [11] without registration of a protocol, with a framework based on the recommendations of The Joanna Briggs Institute (JBI), which consists of the systematic and orderly grouping of scientific evidence on a given topic in order to allow the association between factors and development of a condition (health outcome), based on a strictly structured process, thus ensuring that the results achieved are reliable and significant.
We performed six steps to develop this review, which include: 1) definition of the objective and construction of the guiding question; 2) definition of the search strategy; 3) definition of the inclusion and exclusion criteria and the data to be extracted from the studies; 4) selection of the studies; 5) characterization of the studies and synthesis of the pertinent data; 6) interpretation and presentation of the review.
The guiding question of this review “What is the impact of the COVID-19 pandemic on the mental health of pregnant and puerperal women?” was constructed with the aid of the PICOS strategy, as displayed in Table 1.
| Acronym | Definition | Description |
|---|---|---|
| P | Population or problem | Pregnant and/or puerperal women |
| I | Intervention or interest | COVID-19 pandemic |
| C | Comparison | Not applicable |
| O | Outcome | Impact on Mental Health |
| S | Study type | Original studies with a quantitative approach |
Source: authors.
The bibliographical survey was held during the month of July 2020, taking place in the following electronic databases: MEDLINE via PubMed portal of the US National Library of Medicine, Web of Science (WoS), Excerpta Medica dataBASE (EMBASE), SCOPUS and APA PsycNet, in addition to the MedRxiv and PsyArXiv preprint databases. In order to complement the present study with the other evidence regarding the topic, we performed a manual search.
For the MEDLINE, WoS, EMBASE, SCOPUS, APA PsycNet databases and for the PsyArXiv preprint database, we used the following combination of keywords and Boolean operators: (pregnan* OR puerper* OR prenatal OR perinatal) AND “mental health” AND (COVID-19 OR SARS-CoV-2). For the MedRxiv preprint database, we used the following search strategy: (pregnancy OR pregnant OR puerperium OR puerperal OR prenatal OR perinatal) AND mental health AND (COVID-19 OR SARS-CoV-2).
We should underline that no filters were added as to the language and period of publication of scientific studies, with a view to encompassing the largest possible amount of evidence related to the problem in question.
Accordingly, we identified a total of 150 scientific works in the databases and preprint. Table 2 shows the number of studies retrieved from each queried database.
We established as inclusion criteria, all primary studies that evaluated the mental health of pregnant and puerperal women during the COVID-19 pandemic. In turn, the adopted exclusion criteria were secondary studies, expert opinion articles, experience reports, and other scientific works that did not meet the scope of this review.
| Electronic databases and preprint | Number of identified studies |
|---|---|
| MEDLINE | 28 |
| WOS | 11 |
| EMBASE | 52 |
| SCOPUS | 34 |
| APA PsycNet | 7 |
| PsyArXiv | 2 |
| medRxiv | 16 |
| TOTAL | 150 |
Source: Authors.
Among the 150 identified studies, 69 were removed due to duplication in at least two databases. Thus, 81 screened studies were analyzed, according to the eligibility criteria, by two reviewers, independently and blindly. For any disagreements between the researchers during the analytic process, we called a third researcher for resolution. Accordingly, 14 studies were initially selected to compose the final sample of this review. Subsequently, four more studies were included in the final sample from a manual search based on the references of the secondary articles obtained from the search in the databases.
Thus, we selected 18 studies to compose the final sample of this systematic literature review, aiming at synthesizing the evidence on the impact of the COVID-19 pandemic on the mental health of pregnant and puerperal women. The studies selection process can be viewed at Fig. (1), according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [12].
In this study, we analyzed the quality of the evidence of the included studies using the classification of the Grading of Recommendations, Assessment, Development, and Evaluation Working Group (GRADE). The quality of the evidence obtained through the GRADE allows us to analyze the aggregated results, considering the design and the results of the included studies [13].
The data from the selected studies were extracted and grouped in a table (Table 3) containing specific information related to the research question, namely: author (s); year of publication; country where the research was held; component population and its main characteristics; study design; instruments and/or means used to evaluate mental health status; main outcomes related to the impact of the COVID-19 pandemic on the mental health of pregnant and puerperal women; level of evidence; and main limitations of the studies.
3. RESULTS
We analyzed 18 studies that identified the impact on the mental health of pregnant and puerperal women during the period of the COVID-19 pandemic. In order to perform the synthesis of the selected articles, we drew up a table that summarizes the main characteristics of the included studies [14-31], containing information regarding the reference, location and population, design, outcomes, level of evidence and limitations.
The analysis of the articles enabled us to observe the following characteristics: all articles were published in the year 2020, carried out in 12 different countries, including the United Kingdom [14, 20], Iran [15], India [16], China [17, 19, 25], Canada [18, 21, 30], Belgium [22], Japan [23], United States [24], Italy [26, 31], Australia [27], Ireland [28], and Israel [29].
A total of 10 studies adopted a descriptive cross-sectional design [14, 15, 18, 20, 22, 25, 27-29, 31], one multicenter cross-sectional [19], one analytical cross-sectional [23], one analytical and multicenter cross-sectional [30], three case reports [16, 17, 26], one from a prospective cohort [21] and one from a mixed exploratory method [24].
Anxiety and depression were the main identified outcomes, being shown in 15 [14, 16-22, 24, 25, 27-31] and 11 studies [14, 15, 17-24, 30], respectively. Other outcomes identified in more than one study were: concerns related to several factors [17, 18, 27, 28]; loneliness [18, 20, 24]; stress [24, 27], and fear [15, 16].
The studies evaluated anxiety using several scales: three studies using the Generalized Anxiety Disorder 7-Item Scale – GAD-7 [14, 22, 24], two using the State-Trait Anxiety Inventory – STAI) [30, 31], one using the Hospital Anxiety and Depression Scale – HADS [15], and one using the Hamilton Anxiety Rating Scale – HAM-A) [17]. Another study also used the Self-Rating Anxiety Scale – SAS [25], and another the Pregnancy-related Anxiety Questionnaire – PRAQ [18]. Moreover, two studies evaluated anxiety using specific instruments [20, 29].
Depression was evaluated in one study using the Patient Health Questionnaire-9 – PHQ-9 [14], one using the Hospital Anxiety and Depression Scale – HADS) [15], one using the Hamilton Depression Rating Scale for Depression – HAM-D-17 [17], one using the Montgomery-Åsberg Depression Rating Scale – MADRS [17], four studies using the Edinburgh Postnatal Depression Scale – EPDS [18, 19, 23, 30], two using the Patient Health Questionnaire-2 – PHQ-2 [17, 24] and another study using the Edinburgh Depression Scale (EDS) [22]. Another study also used its own instrument to evaluate depression [20].
Moreover, the fear of COVID-19 was evaluated in one study using the Fear of COVID-19 Scale – FCV-19S) [15]; mental well-being in one study using the Warwick-Edinburgh Mental Well-Being Scale – WEMWBS) [24]; quality of life in one study using the 12-Item Short-Form Health Survey – SF-12) [15]; preventive behavior in one study using the Preventive COVID-19 Behaviour Scale (PCV-19BS); psychological distress in one study using the 10-Item Kessler Psychological Distress Scale – K10) [21]; post-traumatic stress disorder in two studies, one using the Post-traumatic Stress Disorder Checklist 5 – PCL-5 [21] and the other using the Impact of Events Scale–Revised – IES-R) [31]; positive and negative effects in one study using the Positive and Negative Affect Schedule – PANAS) [21]; one study evaluated social support through the Social Skills, Behavior Problems and Academic Competence Inventory for Children (SSRS) [25], and two studies evaluated psychological stress and well-being through the Five-Item Mental Health Inventory – MHI-5 [29] and the Visual Analogue Scale – VAS [31], respectively.
| Code | Location/ Population | Study design | Evaluation instrument | Outcomes (impacts on mental health) | Quality of evidence | Limitations |
| [14] | London, United Kingdom. 11 mothers with confirmed diagnosis of COVID-19, age range between 18 and 39 years and deliveries between the 27th and 39th weeks of pregnancy. |
Descriptive cross-sectional study. | GAD-7 and PHQ-9. | Low levels of anxiety and depression. | Low. | - Small sample size. - Restricted to a single institution. - Without long-term follow-up. |
| [15] | Qazvin, Iran. 290 pregnant women, with an average age of 29 years and an average gestational age of 15 weeks. |
Descriptive cross-sectional study. | APIM, FCV-19S, HADS, SF-12, PHQ-9 and PCV-19BS. | The fear caused by COVID-19 in pregnant and puerperal women was related to the occurrence of depression, suicidal thoughts and worse mental health in this population. | Very low. | - Study design. - Data based on self-report measures. - Potential for social desirability bias. - Memory bias. - Without long-term follow-up. |
| [16] | Bangalore, India. A 24-year-old woman, two months postpartum, without family history or previous psychiatric disorder, and negative RT-PCR test for SARS-CoV-2. |
Case report. | Clinical evaluation. | Psychotic signs and symptoms: anxiety, agitation, irrelevant speech, crying spells, delusions of persecution, overvalued idea that she had contracted COVID-19 and was transmitting to his son, fear of contracting COVID-19, catatonic symptoms of mutism and facing. Medical diagnosis: acute polymorphic psychosis. Consequences during the psychotic break: refusal to breastfeed. |
Low. | - Small sample size. - Restricted to a single institution. |
| [17] | Hangzhou, China. A 30-year-old woman, 35 weeks and two days pregnant, RT-PCR positive test for SARS-CoV-2 and gave birth two days after her diagnosis. |
Case report. | Clinical interview, HAMD-17, MADRS and HAMA. | Signs and symptoms in the psychiatric clinic interview: bad mood, irritability, excessive health concerns, as well as with the newborn child, husband and close relatives, intense feeling of guilt, depression, sad facial expression, anxious emotion, occasional restlessness. Signs and symptoms measured during dialectical behavior therapy: -1st session: high scores for depression and anxiety; -2nd session: decreased scores, but symptoms of depression and anxiety present; -3rd session: low scores with relief of symptoms of depression and anxiety. |
Very low. | - Small sample size. - Restricted to a single institution. - Only one intervention. - Only three therapy sessions. - Without long-term follow-up. |
| [18] | Canada. 1987 pregnant women, with an average age of 32 years and a gestational age of less than 35 weeks. |
Descriptive cross-sectional study. | EPDS, PROMIS, PRAQ, SSEQ and ISEL |
Women reported feelings of loneliness, concerns with their lives and the babies. They presented high depression, general anxiety and pregnancy-related anxiety scores. | Low. | - Absence of interventions. - Without long-term follow-up and support. |
| [19] | China. 4124 pregnant women, in the 3rd trimester of pregnancy, 2839 of whom were evaluated between January 1st and 20th, 2020, and 1285 were evaluated between January 21st and February 9th, 2020. |
Multicenter cross-sectional study. | EPDS. | On January 20th, 2020, the WHO declared that SARS-CoV-2 has human-to-human transmission. Pregnant women evaluated after the SARS-CoV-2 pandemic declaration presented higher anxiety scores, as well as depressive symptoms, than those evaluated before the declaration, in addition to self-mutilation thoughts. | Low. | - Data based on self-report measures. - Scale used had the purpose of screening, and not making a diagnosis. - Absence of intervention. - Without long-term follow-up. |
| [20] | United Kingdom. 1365 women, aged over 18 and babies up to 12 months. |
Descriptive cross-sectional study. | The COVID-19 New Mum Survey. | 146 women reported that the lockdown in the United Kingdom, due to the COVID-19 pandemic, had affected their mental health, causing anxiety, depression, isolation and loneliness. | Low. | - Low diversity of participants. - Pre-existing inequality and social and health differences. - There is a need to encourage the use of health services. |
| [21] | Quebec, Canada. 1258 pregnant women, aged between 18 and 46 years and with an average gestational age of 24 weeks, with some history of psychiatric disorder. Pre-COVID group (April 2018 to March 1st, 2020) n=496. COVID Group (March 2nd to April 13th, 2020) n=1259. Public Health Emergency declared on March 13th, 2020. |
Prospective cohort study. | K10, PCL-5, DES ‐ II and PANAS. | The pregnant women presented an increase in depressive and anxiety symptoms, which can be defined as high psychological distress, high negative affectivity and low positive affectivity, in addition to symptoms of dissociation and post-traumatic stress disorder. | Low. | - Difference in recruitment methods between the two cohorts. - Impossibility of making comparisons between respondents with non-respondents. |
| [22] | Belgium. 5866 women, 2421 pregnant and 3445 postpartum. |
Descriptive cross-sectional study. | EDS and GAD-7. | Increased likelihood of depressive symptoms and anxiety among pregnant and puerperal women during the lockdown decreed in Belgium, due to the COVID-19 pandemic. | Low. | -Restricted to a single institution. - Data based on self-report measures. - Without long-term follow-up. - Little information regarding mental health care for pregnant and puerperal women. |
| [23] | Japan. 132 puerperal women before the pandemic (March 9th to April 11th, 2019) and 148 puerperal women during the pandemic (March 11th to April 13th, 2020). |
Analytical cross-sectional study. | EPDS and MIBS-J. | Depressive symptoms signalized a worse mother-baby connection during the pandemic period. | Very low. | -Small sample size. - Only puerperal women one month after the baby is born. - Without long-term follow-up. - Absence of support strategies for mental health. |
| [24] | Colorado, United States. 27 women, aged between 24 and 45 years, 14 pregnant and 13 puerperal women. |
Mixed, exploratory method. | Semi-structured interview, PHQ-2, GAD-7, BRS, WEMWBS and Solitude Scale. | Since the beginning of the COVID-19 pandemic, pregnant and puerperal women have became more likely to experience symptoms of stress, depression, anxiety, poor well-being, resilience and loneliness. | Very low. | - Small sample size. - Minimum diversity. -Lack of presentation of complications during pregnancy and childbirth. - Recruitment strategy. - Without long-term follow-up. - Absence of support strategies. |
| [25] | Qingdao, China. 308 pregnant women in the third trimester. |
Descriptive cross-sectional study. | SAS, SSRS and Self-made questionnaire. |
In the third trimester, pregnant women presented themselves as a population at high risk of developing anxiety. | Very low. | -Absence of a comparative study between pregnant women and the general population during the COVID-19 outbreak. - Only pregnant women in the third trimester of pregnancy. - Restricted to a single institution. - Data based on self-report measures. - Without long-term follow-up. - Absence of support strategies. |
| [26] | Verona, Italy. A 36-year-old woman, 35 weeks pregnant, hospitalized for severe COVID-19 and with a family history of bipolar disorder. |
Case report. | Not applicable. | The pregnant woman presented a manic episode with serious psychotic characteristics and grandiose delusions. | Very low. | - Small sample size. - Restricted to a single institution. - Absence of complete personal and family history. - Lack of similar studies on the occurrence of psychosis in pregnant and puerperal women. - Without long-term follow-up. |
| [27] | Australia. 147 mothers who sought The Australian Breastfeeding Association (ABA) because of concerns about COVID-19, from March 16th to May 18th, 2020. |
Descriptive cross-sectional study. | Not applicable. | ABA volunteers identified emotional well-being concerns related to COVID-19 and reported that 31 mothers were in difficult isolation by COVID-19, 53 mothers were anxious or stressed by COVID-19 and 63 mothers needed tranquility in the face of the COVID-19 situation. | Very low. | -Failure to use an instrument to evaluate levels of stress and anxiety. - Lack of information about the women described in the study. - Data based on the impressions of the volunteers themselves. - Absence of intervention. - Without long-term follow-up. |
| [28] | Ireland. 71 pregnant women in the second and third trimesters of pregnancy, evaluated between March 16th and 27th, 2020. |
Descriptive cross-sectional study. | Did not mention the instrument used. | Pregnant women showed greater concern with their own health after the onset of the pandemic than before the pandemic. 50.7% (36 out of 71) of the pregnant women reported frequent concerns about their own health, 66.7% (28 out of 42) concerns about their children and 63.4% (45 out of 71) about the unborn baby. Moreover, 83.3% (55 out of 66) reported increased anxiety about the health of their older relatives. |
Low. | -Absence of information about the women described in the study. - Absence of information about the institution. - Absence of information about the method of evaluation of the pregnant women. - Data based on self-report measures. - Without long-term follow-up. - Absence of support strategies. |
| [29] | Israel. 336 Israeli women, 225 of them Jewish and 111 Arabs, aged between 20 and 47 years and gestational age between four and 41 weeks, evaluated between March 18th and 28th, 2020, who were unaware of SARS-CoV-2 infection. |
Descriptive cross-sectional study. | Self-developed questionnaire and MHI-5. | The evaluated pregnant women showed high levels of anxiety due to COVID-19, being related to the use of public transport (87.5%), the potential for infection of other family members (71.7%), the permanence in public places (70%), concerns with the fetus (70%), the accomplishment of pregnancy tests (68.7%), the fear of becoming infected (59.2%), as well as concerns about childbirth (55.4%). Only 38.1% of the pregnant women reported being concerned about the economic damage of the pandemic. Arab women presented more anxiety related to COVID-19 than Jewish women. |
Low. | - Sample that cannot be considered representative of the population of pregnant women in Israel. - Language in which the instrument was presented (Hebrew only). - Differences in average age and schooling levels among participants. - Absence of intervention. - Without long-term follow-up. |
| [30] | Canada. 900 women, 520 pregnant and 380 in the first year after childbirth, aged between 17 and 49 years. 25 with a history of depression and 60 with a history of anxiety. |
Analytical and multicenter cross-sectional study. | EPDS and STAI. | 40.7% of the pregnant women presented high depression scores during the pandemic and moderate to high anxiety was identified in 72% of the women during the pandemic. Nevertheless, women involved in at least 150 minutes of moderate-intensity physical activity during the pandemic had lower scores for both anxiety and depression. |
Low. | - Possible sampling bias. -Data based on self-report measures. - Without long-term follow-up. - Absence of support strategies. |
| [31] | Napoli, Italy. 100 women in the first, second and third trimesters of pregnancy, without history of postpartum depression in a previous pregnancy or psychiatric disorders, evaluated from March 15th to April 1st, 2020. |
Descriptive cross-sectional study. | IES-R, STAI and VAS for anxiety. | Among the evaluated pregnant women, 53 classified the psychological impact of the COVID-19 outbreak as severe and 68 presented anxiety scores above normal. 46 pregnant women reported high anxiety with regard to vertical transmission of the disease. The psychological impact and the anxiety caused by the COVID-19 pandemic were more severe in women who are in the first trimester of pregnancy than in women who are in the second and third trimesters of pregnancy. |
Low. | -Restricted to a single institution. - Data based on self-report measures. - Without long-term follow-up. - Little information regarding mental health care for pregnant and puerperal women. |
RT-PCR - Reverse-Transcriptase Polymerase Chain Reaction
SARS-CoV-2 - Severe Acute Respiratory Syndrome Coronavirus 2
GAD-7 – Generalized Anxiety Disorder 7-Item Scale
PHQ-9 – Patient Health Questionnaire-9
APIM - Actor-Partner Interdependence Model
FCV-19S - Fear of COVID-19 Scale
HADS – Hospital Anxiety and Depression Scale SF-12 – 12-Item Short-Form Health Survey
PCV-19BS – Preventive COVID-19 Behavior Scale
HAMD-17 – Hamilton Depression Rating Scale for Depression MADRS – Montgomery-Åsberg Depression Rating Scale
HAM-A – Hamilton Anxiety Rating Scale
EPDS – Edinburgh Postnatal Depression Scale
PROMIS - Patient-Reported Outcomes Measurement Information System
PRAQ - Pregnancy-related anxiety questionnaire
SSEQ - Social Support Effectiveness Questionnaire
ISEL - Interpersonal Support Evaluation List
K10 – 10-Item Kessler Psychological Distress Scale
PCL-5 - Posttraumatic Stress Disorder Checklist 5
DES ‐ II - Dissociative Experiences Scale
PANAS - Positive and Negative Affect Schedule EDS - Edinburgh Depression Scale
MIBS-J - Mother-Infant Bonding Scale
PHQ-2 - Patient Health Questionnaire-2 BRS - Brief Resilience Scale
WEMWBS – Warwick-Edinburgh Mental Well-Being Scale
SAS – Self-Rating Anxiety Scale
SSRS - Social Support Rating Scale
MHI-5 – Five-Item Mental Health Inventory
STAI – State-Trait Anxiety Inventory
IES-R - The Impact of Events Scale - Revised
VAS - Visual Analogue Scale
Among the 18 analyzed studies, 11 signalized a low level of evidence [14, 16, 18-22, 28-31] and seven very low levels [15, 17, 23-27].
4. DISCUSSION
The results showed that the study population was mentally affected by the onset of symptoms of anxiety, depression, fear, suicidal thoughts, psychomotor agitation, irrelevant speech, crying spells, delusions of persecution and greatness, catatonic symptoms of muteness, bad mood, irritability, excessive concerns, self-harming thoughts, social isolation, loneliness, stress, resilience and poor well-being.
Depression, fear, anxiety, and other psychotic symptoms referred to are configured in the main psychological impacts that affect the mental health of pregnant and puerperal women during the pandemic period of COVID-19, thus reflecting the social, political, and cultural contexts in which we live and their challenging capacities. The current pandemic scenario triggered by COVID-19 and the consequent mitigation measures (social detachment, quarantine, and social isolation) have entailed the intensification of psychological distress for certain groups, which can include women in the pregnancy-puerperal cycle.
This is because pregnancy and postpartum, commonly, are already characterized as periods of hormonal, bodily, and psychological changes in women’s lives. In addition, in the current scenario, a pandemic disease with transmission routes still unclear, threatens maternal and child health. Thus, the current, continuous pandemic situation and the lack of certainty about the future at this moment can be factors causing stress, anxiety, fear, and other symptoms, since, without information, they do not know how to proceed to protect themselves and their babies. This situation has already been reported as recurrent in outbreaks related to other infectious diseases such as H1N1 Influenza, Ebola, Middle East Respiratory Syndrome (MERS), Severe Acute Respiratory Syndrome (SARS), and Zika Virus [32, 33].
Although the vertical transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is not clear, we cannot rule out concerns about the possibility of premature birth; the chances of a cesarean section in cases of an idealized vaginal birth; the lack of humanization during childbirth; the impossibility of breastfeeding; the newborn being isolated from the mother, or the mother and the newborn being isolated from family members and close acquaintances; besides the fear of being infected or the baby being infected by other people [32, 33].
The fear of being infected by COVID-19 is very distressing, mainly because it still does not have a scientifically proven treatment. Social detachment, a primary measure to contain the proliferation of the virus, made people physically isolate themselves from family members, friends, their tasks, and the community, a measure that affected the mental health and psychological well-being of pregnant and puerperal women [18].
In this sense, depressive symptoms were widely identified in studies [14, 15, 17-22], despite the limiting difference observed in culture studies, methods and instruments used, as well as in fear of being infected by infectious diseases, which was significantly associated with depression, stress and anxiety [15, 17-22, 27-31], where only one study performed in the United Kingdom [14] with women aged 18 to 39 years, from the 27th to the 39th weeks of pregnancy, presented a difference in the results, and this was due to the increase in information available about COVID-19 and to the guarantee offered to the population in question with respect to primary care and health professionals.
Symptoms of stress, depression, and anxiety related to COVID-19 have shown a negative effect, thus impacting the mental health of the general population [34-36]. Research conducted at the beginning of the COVID-19 outbreak in Wuhan, China, found that 53.8% of the participants presented symptoms of anxiety and depression (moderate and severe), i.e., 17% and 29%, respectively [6].
Psychological disorders such as depression and anxiety, more present in the lives of pregnant and puerperal women in this pandemic period, have caused serious problems, with a consequent reduction in the quality of life of these individuals. Thus, there is a need to guarantee emotional support in order to mitigate the fear of this illness [18]. Increased social and emotional support contributes to the reduction of psychological distress and to the maintenance of physical well-being, and family and partner support is of utmost importance in this process of social detachment [15], in addition to the issue of resilience [14], which helps to cope well with difficult situations such as a pandemic period.
Conversely, women without a history of pre-existing mental illnesses who did not have support and suffered external pressure caused by third parties had psychotic breaks [16], others with a family history of bipolar disorder and, without support, also had psychotic characteristics [21, 26]. Given this situation, we should observe that the infection and the fear of COVID-19 go beyond the organic issue, pointing to mental and social issues by generating psychological exhaustion, especially for the most vulnerable people who feel unsupported.
One of the studies raised in this review pointed out that mental health problems are prevalent in women of younger ages, low family income, and lower schooling level [21]. Common Mental Disorders (CMD) are challenging for health services, as they have grown alarmingly in the last few years. In particular, the occurrence of these disorders has increased in women since they are twice as likely to develop the disorder as men, mainly when they are in the periods of pregnancy and puerperium [37].
Women in situations of risk of vulnerability, poverty, without a steady partner, young, with hereditary or congenital characteristics and low schooling levels have evolved with depressive and anxious symptoms not only in maternal health but also fetal, which highlights the importance of screening and following-up during pregnancy and puerperium [38-41].
Moreover, many women experienced increased psychological stress, as they did not have the necessary help in the service unit, as well as support when breastfeeding. After childbirth, women may feel helpless, where the lack of support is a factor that can directly affect the breastfeeding process [21].
Based on studies by Thomson, Ebisch-Burton, and Flacking [42], it is common for women to have the need to carry out breastfeeding so that those who do not can feel that they have failed. Nevertheless, according to the authors, both mothers who do not breastfeed and those who breastfeed may suffer from the absence of support and inconvenient judgment, which can even result in feelings of inadequacy and isolation [42]. Such notes show that the scenario related to COVID-19 may be the aggravating factor in the face of the issue that involves complications and the need for attention even outside the pandemic period.
Some limitations should be considered when interpreting the results of this systematic review. We noted heterogeneity in the studies, the use of different instruments for data collection, and distinct follow-up times.
CONCLUSION
From this review, we can infer that the COVID-19 pandemic has impacted the mental health of pregnant and puerperal women. The results have revealed the main changes in the mental health of this population, with depression and anxiety being the most frequent. Several concerns, loneliness, fear, stress, suicidal thoughts, psychosis, agitation, delusions of persecution, and overvalued ideas were also present.
The current pandemic scenario triggered by COVID-19 and the consequent social detachment, media pressure, fear of contracting the infection, economic scenario and rupture of family rituals resulted in observable intensifications of psychological distress, thus causing changes in the mental health of these women.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
Not applicable.
CONFLICT OF INTEREST
Not applicable.
ACKNOWLEDGEMENTS
Not applicable.


