RESEARCH ARTICLE
Burden and Depression among Jordanian Caregivers of Hemodialysis Patients: A Cross-sectional Study
Eman Khamis Alnazly1, *
Article Information
Identifiers and Pagination:
Year: 2021Volume: 15
First Page: 29
Last Page: 37
Publisher ID: TONURSJ-15-29
DOI: 10.2174/1874434602115010029
Article History:
Received Date: 31/8/2020Revision Received Date: 27/1/2021
Acceptance Date: 29/1/2021
Electronic publication date: 17/03/2021
Collection year: 2021

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
Caring for patients receiving hemodialysis places a burden on caregivers.
Objectives:
To examine caregiving burden and depression in the family caregivers of patients receiving hemodialysis and associated factors.
Methods:
A cross-sectional design was used. Participants were 204 adult caregivers of patients receiving hemodialysis. Questionnaires included sociodemographic characteristics, the Oberst Caregiving Burden Scale-Difficulty (OCBS-D) subscale, Bakas Caregiving Outcomes Scale (BCOS), and the Patient Health Questionnaire-9 to measure the burden and depression of caregivers. Descriptive statistics, two linear regression analyses, and multinomial logistic regression were used in data analysis.
Results:
The majority (59.0%, n = 120) of caregivers had a moderate level of depression with scores ranging from 11 to 16. The analysis showed that the mean score of OCBS-D was 42.0 (SD = 4.7) with scores ranging from 26.9 to 58.9 (range = 32.0), while the caregivers' mean score of BCOS was 52.1 (SD = 9.3) with scores ranging from 38.0 to 82.5 (range = 44.5). Given that the expected score of OCBS-D and BCOS ranged from 15 to 75 and 15 to 105, respectively, the analysis indicated a moderate to a high level of burden among caregivers. Age and travel time were associated with a higher likelihood of negative outcomes in the family caregivers, while higher patient age was associated with a greater caregiver burden.
Relevance to Clinical Practice:
It is important to assess and address the practical issues that caregivers experience, such as employment-related responsibilities, financial difficulties, and the need to learn specific skills related to patients’ chronic illnesses.
Conclusion:
Caregivers of patients receiving hemodialysis are likely to experience moderate depression and burden. Caregiver burden increases with patient age and travel time to the hemodialysis units.
1. INTRODUCTION
End-stage kidney disease (ESKD) is a serious medical condition wherein the kidneys are functioning at less than 15% of their capacity. Patients with ESKD require frequent hemodialysis treatments, which involve filtering waste, salt, and fluid from the blood to correct electrolyte imbalances [1]. Patients undergoing hemodialysis are likely to have other comorbidities, such as diabetes, cardiovascular disease, hypertension, multiple metabolic disturbances, and skeletal problems, which negatively affect their mobility and ability to complete self-care [2]. The treatment places a burden on patients receiving hemodialysis and family caregiver support is important for successfully adapting to the hemodialysis treatment and complying with the treatment regimen [3, 4]. Family caregivers provide unpaid care and devote considerable time to assisting patients with activities of daily living and medical tasks [5, 6]. Beanlands et al. [7] described family caregiving tasks such as traveling to the hemodialysis unit, preparing food, adhering to fluid restrictions, organizing supplies, managing symptoms, and arranging medical appointments. In addition, caregivers evaluate and monitor the patients' medical condition and response to treatment, manage all care activities, create daily routines, communicate with health professionals, and most importantly teach, enforce, and encourage self-care.
1.1. Background
Few studies have examined caregiver burden and depression in family caregivers [8]. Hoang et al. [8] literature review indicated that caregivers experience burden and social isolation and feel overwhelmed. Eirini and Gerogianni [9] reported that caregivers experience physical and psychological distress, including feelings of anger, depression, helplessness, fear, neglect, and tiredness. Burden occurs because caregivers often are limited in the degree to which they can offer care and assistance to patients, which negatively impacts their psychological well-being. Poor psychological well-being of caregivers may subsequently prevent proper care for the patients [10-12].
Various interrelated factors are associated with caregiver burden, including the patients’ and caregivers’ sociodemo- graphic variables [13, 14]. Spouses experience lower caregiving burdens compared to other family members [15], while female caregivers experience a higher burden than their male counterparts [16]. However, the level of burden varies from moderate [17-19] to severe [8, 19], as do the associated depression levels [14]. Predictors of family caregiver burden include caregivers’ health status, time spent caregiving, and task difficulty [8].
Hoang et al. [5] conducted a systematic review to evaluate studies on the experience of family members and friends who offer care to adults receiving either peritoneal dialysis or hemodialysis. The caregivers performed activities of daily living and a range of dialysis-specific tasks. The review showed that burden led to experiencing social isolation, feeling overwhelmed, and needing to consider their own health. However, this review also identified positive outcomes for caregivers. Family caregivers reported personal growth, which may positively impact caregiver burden and help caregivers to endure caregiving through hard times and throughout several years [5]. Positive outcomes of caregiving include rewarding and increased satisfaction with patient care and a stronger relationship with patients [20]; however, caregiving is often associated with a negative impact on emotional well-being, including an increased risk of depression [8, 21].
Caregivers of patients receiving hemodialysis have higher depression levels than caregivers of patients with other illnesses [22, 23] as demonstrated in a review of qualitative studies to examine the perspectives and experiences of family caregivers of patients receiving home hemodialysis. The findings indicated that the family caregiver’s burden and isolation from other support systems induced fear and anxiety. Family caregivers devote their effort, time, and energy to provide emotional, financial, and physical support to an ill family member [23]. In most cases, the caregiver’s emotional state is adversely affected because of the demanding nature of the caregiving role [24].
The difficulties of providing adequate care were examined by Welch et al. [25] and Alnazly and Samara [26]. Welch et al. [25] conducted a qualitative study on caregivers aged 65 years and older examining the needs and concerns of caregivers of patients on daily home dialysis. Caregiver concerns were treatment-related care, treatment complications, handling emergencies (physical care), providing transportation, going to appointments, managing finance (instrumental care), depression, negative behaviors (dealing with the emotions and behaviors of the patient), lifestyle changes, anger, fear, and not having enough time for self-care (personal responses to caregiving). The caregivers in this study were concerned due to the long-term care required for patients undergoing dialysis. Alnazly and Samara [26] identified three themes of caregiver burden. The first theme was social isolation, which encompasses the caregivers’ feeling of being distanced from close relatives and friends. The second theme was health-related problems, which impact the physical functioning of the caregiver, and psychological problems, such as low energy levels, little sleep, and fatigue. The last theme was finding less time for self-care due to the time spent with patients during hemodialysis and preparing a renal diet. Tong et al. [27] described these symptoms as intrapersonal issues, which involve the psychological and physical impact of caregiving.
There are currently no established caregiver statistics for patients receiving hemodialysis in Jordan. Nevertheless, it is estimated that 56.4% are under the age of 30, 30.2% are aged 30 – 45 [28], and total 63.0% are employed [17]. Research on caregiver burden can facilitate the provision of an improved understanding of the caregiver's psychological and physical health and associated adaptation outcomes. However, few studies have examined caregiving burden, outcomes, and depression among Jordanian family caregivers of patients receiving hemodialysis. The association of the caregivers’ and patients’ sociodemographic characteristics in this regard and caregiver role is still not recognized locally and internationally. This study aimed to examine caregiving burden and depression among family caregivers of patients receiving hemodialysis and to determine the extent to which caregiver burden and depression vary with respect to sociodemographic variables.
2. METHODS
2.1. Study Design
This cross-sectional study was conducted during the month of May 2020 in Amman, Jordan.
2.2. Study Population
A convenience sample of family caregivers was recruited from four private outpatient hemodialysis units in Amman. The research team approached 210 patients, who then contacted the patients’ respective caregivers. Consequently, 204 caregivers were selected for the study.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria were: (i) being an unpaid family caregiver(ii) aged over 20(iii) for at least one year prior to the study. Exclusion criteria were (i) paid family caregivers or (ii) a paid housekeeper to help with care.
2.4. Data Collection
After receiving permission to conduct the study, two staff members volunteered to assist with caregiver recruitment and approached individuals who were identified by patients as primary caregivers. Caregivers who agreed to participate were then contacted by the researcher and received the following four documents: a sociodemographic questionnaire, the Patient Health Questionnaire-9 (PHQ-9), the Oberst Caregiving Burden-Scale-Difficulty subscale (OCBS-D), and the Bakas Caregiving Outcomes Scale (BCOS). The questionnaires were completed during the caregivers’ first meeting with the researcher in the hemodialysis units’ waiting rooms or at home and then during the next visit to the hemodialysis unit. The caregivers were instructed to place the completed questionnaires in a box placed in the waiting room. The researcher also provided the participants with contact information to clarify any doubts regarding the study.
2.5. Caregiver Assessments
2.5.1. Sociodemographic Characteristics
The sociodemographic form, developed by the researcher, covered details including patient’s age and gender, caregiver’s age, gender, marital status, relationship with the patient, caregiver’s residence, economic status, employment status, one or more chronic illnesses, years of caregiving, and travel time to the hemodialysis unit.
2.5.2. Assessment of Caregiver Depression Symptoms
The PHQ-9 is a well-validated nine-item instrument used to measure depressive symptoms.Responses were given using a four-point Likert scale, (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day) [29]. This instrument yielded a total score and individual scores for four subscales. Depression severity was calculated by summing the scores for the nine assessed items. The severity index score was categorized as follows: none (0–4), mild (5–9), moderate (10–14), moderate to severe (15–19), and severe (20–27). The cut-off for the identification of major depressive disorder was > 10, and the tool had a sensitivity of 88%. Cronbach’s alpha in the original scale [29]and the current study were 0.88and 0.78, respectively.
2.5.3. Assessment of Caregiver Burden
The caregiver burden was assessed using the OCBS-D and the BCOS. The OCBS-D assessed the level of caregiver burden by considering the difficulty (both emotional and physical)of the caregiving tasks [30]. The OCBS-D contained 15 items, measured using a five-point Likert scale (1 = not difficult, 2 = slightly difficult, 3 = moderately difficult, 4 = very difficult, and 5 = extremely difficult). Higher scores indicated greater difficulty levels [30]. The scores for the 15 items were summed (total score of 15–75). The Cronbach’s alphas in the original [30]and the current study were 0.94 and 0.80, respectively.
The BCOS assessed caregiving's positive and negative aspects, including social function, subjective well-being, and physical health. On this 15-item questionnaire, rated on a seven-point Likert scale, scores ˂4 indicated a negative perception of caregiving outcomes, a score of 4indicated no change, and scores ˃4 indicated positive results. The scores were summed, and the total scores ranged from 15 to 105, where the lower score indicated a greater caregiving burden. Cronbach’s alphas in the original [31] and the current study were 0.90 and 0.82, respectively.
The three scales were translated from English into Arabic; the process involved translation, back-translation, committee review, pre-testing, and weighing of scores [32]. The instruments were pilot tested with 12 caregivers of patients receiving hemodialysis (excluded from the main study). Cronbach’s alphas were: PHQ-9 = 0.88, OCBS-D = 0.84, and BCOS = 0.80.
2.6. Statistical Analyses
Data analysis was performed using Stata MP 13 [33]. Initially, descriptive statistics were calculated; these consisted of frequency tables reporting the sample sizes and percentages of responses for the PHQ-9, and normality tests for continuous measures of interest. Additionally, regression analyses were conducted to examine the association of several factors with OCBS-D and BCOS scores, with multinomial logistic regression analysis conducted on the outcome of the PHQ-9. A p-value < 0.05 was considered significant.
2.7. Ethical Consideration
This study was conducted in compliance with the Declaration of Helsinki and with the approval of the Institutional Review Board at Al-Ahliyya Amman University, ID number 2020-2019/9/1 prior to data collection. The study's aims were explained to all participating caregivers, who were assured of the confidentiality and anonymity of their data. All participants provided written informed consent and were informed that they could withdraw from the study at any time without penalty.
3. RESULTS
3.1. Descriptive Statistics
A total of 204 family caregivers of patients receiving hemodialysis participated. Ages ranged from 21 to 70, with 50.4% of participants aged 41–50 (n = 103; 50.0%). Women represented 55%(n = 111) of participants,married participants were 74.5% (n = 149),and 51% were unemployed (n = 103). The leastcommon association was daughter/daughter-in-law of the patient (n = 57; 27.9%); 35.8% (n = 73) and 36.3% (n = 74) of caregivers were sons and spouses of the patients, respectively. Overall, duration of caregiving was 1–10 years; 50% (n = 103) of participants had been caregiving for 3–5 years. Over half of the caregivers (n = 120; 58.8%) lived with the patients and the rest lived close by. The remaining demographic data are presented in Table 1.
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Patient’s age (years) | 20–30 | 4 | 2.0 |
| 31–40 | 6 | 3.0 | |
| 41–50 | 12 | 6.0 | |
| 51–60 | 60 | 29.0 | |
| 61–70 | 89 | 44.0 | |
| > 70 | 33 | 16.0 | |
| Patient’s gender | Male | 127 | 62.0 |
| Female | 77 | 38.0 | |
| Caregiver’s age (years) | 21–30 | 10 | 5.0 |
| 31–40 | 37 | 18.0 | |
| 41–50 | 103 | 50.0 | |
| 51–60 | 44 | 20.0 | |
| 61–70 | 10 | 5.0 | |
| Caregiver’s gender | Male | 91 | 45.0 |
| Female | 111 | 55.0 | |
| Caregiver’s marital status | Single | 51 | 25.5 |
| Married | 149 | 74.5 | |
| Caregiver’s relationship to the patient | Daughter/daughter in-law | 57 | 27.9 |
| Son | 73 | 35.8 | |
| Spouse | 74 | 36.3 | |
| Caregiver’s residence | With the patient | 120 | 58.8 |
| Within walking distance (less than 10 minutes’ walk) | 84 | 41.2 | |
| Caregiver’s economic status | Not sufficient1 | 19 | 9.5 |
| Sufficient2 | 75 | 37.3 | |
| Comfortable3 | 107 | 53.2 | |
| Caregiver’s employment status | Employed | 99 | 49.0 |
| Unemployed | 103 | 51.0 | |
| Total | 202 | 100.0 | |
| One or more chronic illnesses | Yes | 57 | 28.6 |
| No | 142 | 71.4 | |
| Years of caregiving | 1-2 | 64 | 31.7 |
| 3–5 | 103 | 51.0 | |
| 6–10 | 35 | 17.3 | |
| Travel time to hemodialysis unit (round trip) (minutes) | > 45 | 34 | 17.0 |
| 45 - 60 | 60 | 30.0 | |
| < 60 | 106 | 53.0 |
| level of depression | Score range | n | % |
|---|---|---|---|
| None | 1-4 | 0 | 0.0 |
| Mild | 5-9 | 3 | 1.5 |
| Moderate | 10-14 | 120 | 58.8 |
| moderate to severe | 15-19 | 78 | 38.2 |
| Severe | 20-27 | 3 | 1.5 |
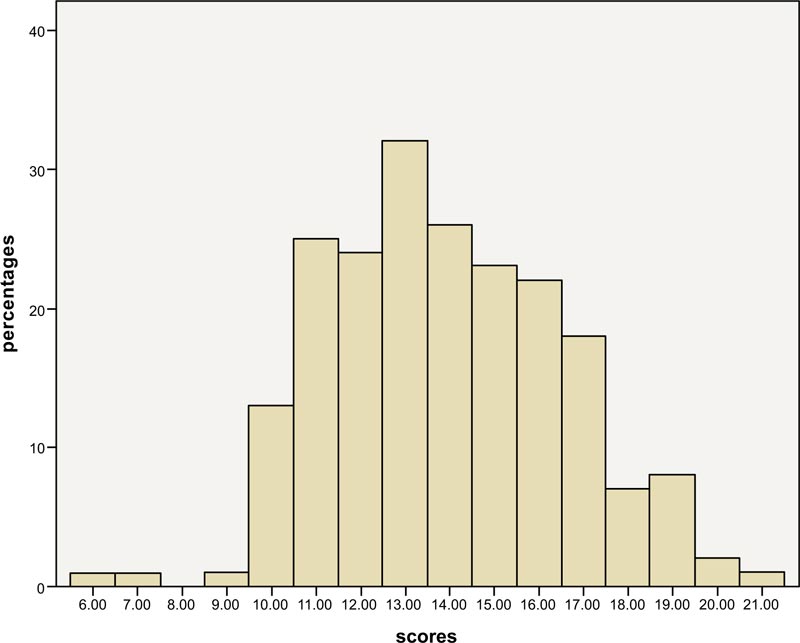 |
Fig. (1). PHQ-9 scores and percentage. |
Caregiver depression was measured using the PHQ-9. Fig. (1) shows scores obtained for the PHQ-9 across the sample and the percentage of participants who obtained each score. Almost 75% of the participants scored between 11 and 16, with each score in this range respectively representing over 10% of the respondents; in particular, the total score of 13 represented 15.7%. With respect to the recorded version of the PHQ-9 (Table 2), category three (scores of 10–14) represented 58.8% of the total sample, while category four (scores of 15–19) represented 38.2%. Two categories, mild (5–9) and severe (20–27), represented 1.5% of this sample, respectively. Thus, the recoded PHQ-9 scores indicated that 1.5% of the caregivers had mild depression, 58.8% had moderate depression, 38.2% had moderately severe depression, and 1.5% had severe depression.
3.2. Burden Scale
The analysis showed that the mean score of OCBS-D was 42.0 (SD = 4.7), with scores ranging from 26.9 to 58.9 (range = 32.0), while the caregivers' mean score of BCOS was 52.1 (SD = 9.3), with scores ranging from 38.0 to 82.5 (range = 44.5). Given that the expected score of OCBS-D and BCOS ranged from 15 to 75 and from 15 to 105, respectively, the analysis indicated a moderate to a high level of burden among caregivers.
3.3. Regression Analyses
Three regression analyses were conducted to examine the association between caregiving task difficulties, caregiving outcomes, and depression. The independent variables included patient age, years spent caregiving, travel time to hemodialysis units, and gender.
Table 3 presents the regression analysis results for the OCBS-D in relation to patient age, years spent caregiving, travel time to hemodialysis units, and gender. The only significant association concerned patient age; in this positive association, each additional year was associated with a predicted increase of 0.1 units in OCBS-D score. Higher patient age was associated with greater perceived difficulty of caregiver tasks. However, this regression model failed to reach statistical significance at the 0.05 alpha level, with the adjusted R-squared indicating that all factors explained 2.3% of the variance in the OCBS-D in this model.
| Measure | B (SE) | Beta | t | 95% confidence interval for B | |
|---|---|---|---|---|---|
| - | - | - | - | Lower | Upper |
| (Constant) | 32.587 (3.189) | 10.220*** | 26.298 | 38.876 | |
| Patient age | 0.115 (.042) | 0.194 | 2.708** | 0.031 | 0.199 |
| Years caregiving | 0.047 (.220) | 0.015 | 0.213 | −0.388 | 0.482 |
| Travel time to hemodialysis unit | 0.020 (.018) | 0.080 | 1.131 | −0.015 | 0.055 |
| Female | 0.320 (.658) | 0.034 | 0.486 | −0.978 | 1.618 |
| Measure | B (SE) | Beta | t | 95% confidence interval for B | |
|---|---|---|---|---|---|
| - | - | - | - | Lower | Upper |
| (Constant) | 32.706 (6.041) | 5.414*** | 20.791 | 44.621 | |
| Patient age | 0.179 (.080) | 0.158 | 2.225* | .020 | 0.338 |
| Years caregiving | 0.520 (.418) | 0.088 | 1.245 | −0.304 | 1.344 |
| Travel time to the hemodialysis unit | 0.071 (.034) | 0.148 | 2.095* | 0.004 | 0.137 |
| Female | 0.372 (1.247) | 0.021 | 0.298 | −2.087 | 2.830 |
| Measure | B (SE) | Wald χ2 (df) | OR | 95% confidence interval for OR | |
|---|---|---|---|---|---|
| - | - | - | - | Lower | Upper |
| PHQ-9: Category 4 | |||||
| Intercept | −1.405 (1.482) | 0.899 (1) | |||
| Patient age | 0.004 (.020) | 0.036 (1) | 1.004 | 0.966 | 1.043 |
| Years caregiving | 0.027 (.102) | 0.069 (1) | 1.027 | 0.841 | 1.254 |
| Travel time to the hemodialysis unit | 0.010 (.008) | 1.352 (1) | 1.010 | 0.993 | 1.026 |
| Female | −0.162 (.304) | 0.284 (1) | 0.850 | .469 | 1.543 |
| PHQ-9: Category 5 | |||||
| Intercept | −22.703 (10.990) | 4.267* (1) | |||
| Patient age | 0.241 (.146) | 2.716 (1) | 1.273 | 0.955 | 1.695 |
| Years caregiving | −0.331 (.576) | 0.331 (1) | 0.718 | 0.232 | 2.220 |
| Travel time to the hemodialysis unit | 0.047 (.042) | 1.210 (1) | 1.048 | 0.964 | 1.139 |
| Female | −0.402 (1.580) | 0.065 (1) | 0.669 | 0.030 | 14.804 |
Table 4 presents the results of the linear regression analysis conducted on the BCOS. Patient age and travel time were positively correlated. Specifically, a one-year increase in patient age was associated with a predicted 0.18 unit increase in BCOS score, while a one-hour increase in travel time was associated with a predicted 0.071 unit increase in BCOS score. This model was statistically significant with the adjusted R-squared indicating that 3.4% of the variance was explained by all included factors.
Multinomial logistic regression was conducted. In this analysis, categories two and three of the PHQ-9 were combined and omitted from the analysis, as they were used to represent the comparison category. Significance was not indicated in any case, with this regression model failing to achieve statistical significance, and the pseudo-R-squared measures were similar to the adjusted R-squared measures in the previous two linear regression analyses (Table 5).
These analyses showed that higher patient age was associated with higher predicted values for a burden for both the OCBS-D and BCOS and that increased travel time was also associated with increased BCOS score. None of the factors were associated with caregiver depression for the PHQ-9.
4. DISCUSSION
This study analyzed a sample of Jordanian family caregivers of patients receiving hemodialysis to estimate caregiver burden levels, depression, and the extent to which caregiver burden and depression are associated with a particular caregiver and patient sociodemographic variables. The results of this study show that caregivers experience burden and depression. Over half of the participants were moderately depressed, found caregiving tasks moderately difficult, and perceived their lives as worsened.
Nonetheless, they perceived caregiving tasks as having a slight to a moderate burden. It seems that the level of perceived burden in this study, which includes all changes and difficulties in the caregiver's life, arose from providing care to the patient, which is similar to the findings of studies conducted on caregivers of patients receiving hemodialysis in Pakistan [8], Saudi Arabia [13], Jordan [17], and Turkey [15]. The majority of caregivers had moderate to severe levels of burden. Hoang et al. [5] also reported a moderate to severe burden in family caregivers of Vietnamese patients. However [5], family caregivers' perceived caregiving tasks as being only slightly difficult. Nonetheless, although caregivers' level of task difficulties is vital to estimate burden level, determining which caregiving tasks are perceived as being the most difficult or as worsening caregivers' lives is more critical to determine the priority areas of intervention.
Caregivers of patients receiving hemodialysis perceived burden and depression. The finding of this study reported that 58.8% of caregivers were moderately depressed and none of the factors (caregiver burden, caregiver outcomes, and sociodemographic factors) were associated with caregiver depression according to the PHQ-9. This finding needs further investigation. For example, caregiver burden and depression were positively correlated in a population of caregivers of patients who had experienced a stroke [34]. Another study found a correlation between perceived task difficulty and depression in advanced cancer caregivers in Greece [35]. One study found that caregivers of patients with dementia experienced high burden, persisting depression, and worsened condition after 12 months compared to a group of caregivers with a lower level of burden [36]. Moreover, an increase in caregiver burden score was associated with an increase in the risk of reporting depression [37].
Determining the sociodemographic factors that worsened caregivers' lives is important because negative outcomes are associated with poorer mental health. There were significant positive associations between patient age and travel time. A one-year increase in patient age was also associated with an increase in BCOS score, while a one-hour increase in travel time was associated with increased BCOS scores. These findings emphasize the negative outcomes that providing care has on family caregivers of patients receiving hemodialysis. In Jordan, family caregivers volunteered to care for chronically ill patients at home [38]. Together with the demanding nature of caregiving, family caregivers must learn new skills to perform their roles effectively. However, the added responsibility and task difficulties negatively impact the caregivers’ lives. Previous studies found that the worse caregivers' outcomes changes were low energy and feeling tired, financial problems, emotional well-being, roles in life, social activities, and ability to cope with stress [39, 40].
The relationships between the study variables indicated that perception of task difficulty was associated with the patients' age. Some studies have examined how sociodemographic characteristics impact caregiver burden and emotional distress [11, 22]. It has been reported that a patients' functional status, being the primary caregiver, caregiving duration, employment status, perceived health, and impact of caregiving on social activities significantly correlated with caregiver burden and depression [11, 22]. The current study's key finding is the associations between the variables, which indicated significant associations between perceived burden (task difficulty and outcomes) and patient’s age: the older the patient, the greater the perceived task difficulty and the more negative the caregiver outcomes are. These findings should not be ignored as family caregivers need help at home caring for older patients and transporting patients to dialysis centers.
Approximately 44% of the patients were aged 61–70, and 16% were 71 or older. Along with having a chronic illness (ESKD), older patients were physically weaker and may have exhibited declining body functions, thus increasing caregiver burden [41]. However, approximately 50% of the caregivers were aged 41–50; this age group is usually part of Jordan's workforce. Therefore, patient and caregiver age must be considered when understanding caregivers' psychological health and supporting older caregivers. Additionally, travel time to the hemodialysis units was associated with negative caregiving outcomes. Many family caregivers are responsible for transporting patients to the hemodialysis unit, which is required three times a week on average. Using public transportation or driving across a busy town to a hemodialysis unit may also exacerbate a caregivers' burden. However, caregiving in Jordan is the responsibility of family members because of their cultural history of kinship-related support, which expects family members to care for older and ill family members. Family members have a high sense of obligation and commitment to providing such multifaceted care, which leads to increased caregiver burden and mental health issues like depression. Increased travel time was also associated with a greater likelihood of negative outcomes and caregiver burden.
This study has some limitations. First, owing to the cross-sectional design, it was not possible to make causal inferences. Second, time constraints prevented us from using a qualitative methodology, which would have deepened our understanding of family caregivers' experiences and reported caregiving burden more accurately. Studies in this field are limited to physical or psychological symptoms and concerns. Third, this study used self-reporting to identify depression in caregivers. Those with moderate to severe levels of depression were identified with a clinical follow-up interview. Another limitation was that this was a cross-sectional sample of participants. Using a longitudinal approach may allow for a better understanding of caregiving's impact on caregivers' health status.
5. IMPLICATIONS FOR CLINICAL PRACTICE
5.1. The Implication for Clinical Practice
Family caregivers assume numerous responsibilities. Thus, interventions to address caregiver burden should be preceded by a comprehensive assessment of the family caregiver. By identifying a caregiver’s risk areas and needs, such interventions can target the characteristics and functional limitations of the family, caregiver, patient, and the caregiving outcomes (such as physical and emotional burden). Interventions at this level should use community resources, such as educational support, healthcare, and psychological health services, which are generally available through kidney patient societies and respite services provided by social organizations. Furthermore, although most research has focused on reducing caregiver burden, it is imperative to assess and address the practical issues experienced by caregivers, such as employment-related responsibilities, financial difficulties, transportation to the dialysis unit, respite care, and the need to learn specific skills related to patients’ chronic illnesses.
These findings are important for nurses in planning care for caregivers by acknowledging and supporting caregivers’ roles.
CONCLUSION
This study shows that caregivers of patients receiving hemodialysis have a moderate to severe level of burden that is significantly associated with increases in the patient’s age and travel time to hemodialysis units. Further evaluation of the depression and burden experienced by caregivers by age group is recommended to improve the understanding of these findings and facilitate generalization to a larger population of caregivers.
LIST OF ABBREVIATION
| BCOS | = Bakas Caregiving Outcomes Scale. |
| ESKD | = End-stage kidney disease (ESKD) |
| OCBS-D | = Oberst Caregiving Burden-Scale-Difficulty subscale. |
| PHQ-9 | = Patient Health Questionnaire-9. |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by Institutional Review Board at Al-Ahliyya Amman University, ID number 2020-2019/9/1.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided written informed consent.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available from the corresponding author [E. K] on reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The author would like to thank all caregivers, nurses, and nurse managers for their support and participation in the study.
REFERENCES
| [1] | Al-Qaisi S, Asaad M. Non-communicable disease directorate, National Registry of End Stage Renal Disease Annual report 2016 2016. [https://www.moh.gov.jo/Echobusv3.0/ SystemAssets/debff26b-c6df-4244-b7f6-4244cdf58733.pdf,] |
| [2] | Rutkowski B, Rychlik I. Daily hemodialysis and caregivers burden. Nephrol Dial Transplant 2011; 26(7): 2074-6. |
| [3] | Roth DL, Fredman L, Haley WE. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist 2015; 55(2): 309-19. |
| [4] | Ayoub AM, Hijjazi KH. Quality of life in dialysis patients from the United Arab Emirates. J Family Community Med 2013; 20(2): 106-12. |
| [5] | Hoang VL, Green T, Bonner A. Informal caregivers of people undergoing haemodialysis: Associations between activities and burden. J Ren Care 2019; 45(3): 151-8. |
| [6] | Suri RS, Larive B, Garg AX, et al. Burden on caregivers as perceived by hemodialysis patients in the Frequent Hemodialysis Network (FHN) trials. Nephrol Dial Transplant 2011; 26(7): 2316-22. |
| [7] | Beanlands H, Horsburgh ME, Fox S, et al. Caregiving by family and friends of adults receiving dialysis. Nephrol Nurs J 2005; 32(6): 621-31. |
| [8] | Hoang VL, Green T, Bonner A. Informal caregivers’ experiences of caring for people receiving dialysis: A mixed-methods systematic review. J Ren Care 2018; 44(2): 82-95. |
| [9] | Eirini G, Gerogianne G. Caregivers of patients on haemodialysis. Caregiving and home care 2018; 14: 75. |
| [10] | Shah HU, Atif I, Rashed F, et al. Assessment of caregiver burden of patients receiving dialysis treatment in Rawalpindi 2017 . Available at: https://www.researchgate.net/publication/321937561_Caregiver_ Burden_for_Patients_Receiving_Dialysis |
| [11] | Alnazly E. Predictors of the burden on family carers of patients on haemodialysis in Jordan. East Mediterr Health J 2020; 26(5): 565-72. |
| [12] | Gray RS, Hahn L, Thapsuwan S, Thongcharoenchupong N. Strength and stress: Positive and negative impacts on caregivers for older adults in Thailand. Australas J Ageing 2016; 35(2): E7-E12. |
| [13] | Bayoumi MM. Subjective burden on family carers of hemodialysis patients 2014. Available at: https://file.scirp.org/Html/4-2070099_ 46689.htm |
| [14] | Mashayekhi F, Pilevarzadeh M, Rafati F. The assessment of caregiver burden in caregivers of hemodialysis patients. Mater Sociomed 2015; 27(5): 333-6. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC4639350/ |
| [15] | Mollaoğlu M, Kayataş M, Yürügen B. Effects on caregiver burden of education related to home care in patients undergoing hemodialysis. Hemodial Int 2013; 17(3): 413-20. |
| [16] | Papastavrou E, Tsangari H, Kalokerinou A. Gender issues in caring for demented relatives. Health Sci J 2009; 3(1): 41-53 . Available at: https://www. fisheriessciences.com/fisheries-aqua/gender-issues-in-caring-for-demented-relatives.pdf |
| [17] | Alnazly EK. Burden and coping strategies among Jordanian caregivers of patients undergoing hemodialysis. Hemodial Int 2016; 20(1): 84-93. |
| [18] | Griva K, Goh CS, Kang WCA, et al. Quality of life and emotional distress in patients and burden in caregivers: a comparison between assisted peritoneal dialysis and self-care peritoneal dialysis. Qual Life Res 2016; 25(2): 373-84. |
| [19] | Hamdi S, Deyab BA, Kamel N. Predictors of perceived caregiving burden among caregivers of hemodialysis patients. Sylwan 2020; 164(5) |
| [20] | National Opinion Research Center. Long term care in America: Expectations and realities 2014 . Available at: https://www. longtermcarepoll.org/wp-content/uploads/2017/11/AP-NORC-Long-term-Care-2014_Trend_Report.pdf |
| [21] | Lin E, Durbin J, Volpe T, et al. Measuring the family/friend caregiver experience in Ontario: Pilot study results 2016 . Available at: http://hsprn.ca/uploads /files/CGStudyPilotResults_HSPRNFinalReport.pdf |
| [22] | Zyada F, Sheta M, El Degwi H, et al. Anxiety, depression, and strain among caregivers of terminally ill patients. Egypt J Psychol 2013; 34(2): 77-84. |
| [23] | Walker RC, Hanson CS, Palmer SC, et al. Patient and caregiver perspectives on home hemodialysis: a systematic review. Am J Kidney Dis 2015; 65(3): 451-63. |
| [24] | Gerogianni G, Polikandrioti M, Babatsikou F, et al. Anxiety-Depression of Dialysis Patients and Their Caregivers 2019. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6572629/pdf/ medicina-55-00168.pdf |
| [25] | Welch JL, Thomas-Hawkins C, Bakas T, et al. Needs, concerns, strategies, and advice of daily home hemodialysis caregivers. Clin Nurs Res 2014; 23(6): 644-63. |
| [26] | Alnazly EK, Samara NA. The burdens on caregivers of patients above 65 years old receiving hemodialysis: A qualitative study. Health Care Curr Rev 2014; 2(1): 118. |
| [27] | Tong A, Sainsbury P, Craig JC. Support interventions for caregivers of people with chronic kidney disease: a systematic review. Nephrol Dial Transplant 2008; 23(12): 3960-5. |
| [28] | Alnazly E. Coping strategies and socio-demographic characteristics among Jordanian caregivers of patients receiving hemodialysis. Saudi J Kidney Dis Transpl 2016; 27(1): 101-106 .http://www.sjkdt. org/text.asp?2016/27/1/101/174088 |
| [29] | Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16(9): 606-13. Available at: 10.1046/j.1525-1497.2001.016009606.x |
| [30] | Bakas T, Austin JK, Jessup SL, Williams LS, Oberst MT. Time and difficulty of tasks provided by family caregivers of stroke survivors. J Neurosci Nurs 2004; 36(2): 95-106. |
| [31] | Bakas T, Champion V, Perkins SM, Farran CJ, Williams LS. Psychometric testing of the revised 15-item Bakas Caregiving Outcomes Scale. Nurs Res 2006; 55(5): 346-55. |
| [32] | Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993; 46(12): 1417-32. |
| [33] | Stata Statistical Software: Release 13 2013. |
| [34] | Denno MS, Gillard PJ, Graham GD, et al. Anxiety and depression associated with caregiver burden in caregivers of stroke survivors with spasticity. Arch Phys Med Rehabil 2013; 94(9): 1731-6. |
| [35] | Govina O, Vlachou E, Kavga-Papaglou A, et al. Exploring the factors influencing time and difficulty of tasks provided by family caregivers of patients with advanced cancer in Greece. Health Sci J 2014; 8(4): 438-51. |
| [36] | Epstein-Lubow G, Davis JD, Miller IW, Tremont G. Persisting burden predicts depressive symptoms in dementia caregivers. J Geriatr Psychiatry Neurol 2008; 21(3): 198-203. |
| [37] | Ho SC, Chan A, Woo J, Chong P, Sham A. Impact of caregiving on health and quality of life: a comparative population-based study of caregivers for elderly persons and noncaregivers. J Gerontol A Biol Sci Med Sci 2009; 64(8): 873-9. |
| [38] | Abu Kamel AM. Who are the elder’s caregivers in Jordan: A cross-sectional study. J Nurs Educ Pract 2016; 6(3): 116-21. |
| [39] | Bakas T, Kroenke K, Plue LD, Perkins SM, Williams LS. Outcomes among family caregivers of aphasic versus nonaphasic stroke survivors. Rehabil Nurs 2006; 31(1): 33-42. |
| [40] | Alnazly EK. The impact of an educational intervention in caregiving outcomes in Jordanian caregivers of patients receiving hemodialysis: A single group pre-and-post test. Int J Nurs Sci 2018; 30;5(2): 144-50. |
| [41] | Hunt GG, Reinhard S. Caregiving in the US American Association of Retired Persons [AARP] Public Policy Institute & National Alliance for Caregiving 2015. Available at: https://www.aarp.org/ content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf |









