All published articles of this journal are available on ScienceDirect.
The Prevention of Mother-to-Child HIV/AIDS Transmission at Public Health Centers: A Phenomenology Study
Abstract
Objective:
Mothers with HIV are likely to transmit the virus to their babies during pregnancy, delivery, or through breastfeeding. According to studies, the risk of mother-to-child HIV transmission among mothers that do not receive any form of treatment during pregnancy is approximately 15-45%. In Indonesia, the lack of a prevention program for HIV led to the provision of antiretroviral therapy (ART) for the prevention of mother-to-child transmission (PMTCT). The policies, financial facilities, the healthcare system, and human resources, including health workers, are factors that influence the PMTCT. This research discusses the perceptions of several doctors and midwives regarding the prevention of mother-to-child transmission at public health centers. Furthermore, information regarding policies and implementation of the PMTCT program at public health centers in Yogyakarta was qualitatively collected through semi-structured interviews.
Methods:
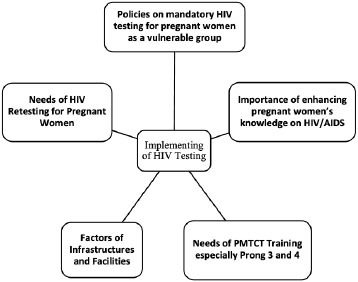
This research involved 6 participants, comprising of 3 heads of public health centers and 3 midwives as the HIV/AIDS program managers. A total of 5 themes were selected for the interview, namely policies of mandatory HIV testing for pregnant mothers, inadequate knowledge of the virus, need for PMTCT training, infrastructure and facilities, and HIV retesting.
Results:
Pregnant mothers are at potential risk of exposing health workers to HIV. They are also prone to contracting the virus due to poor educational background and less exposure to health information. Therefore, midwives need Prongs 3 and 4 to avoid contracting the virus while assisting pregnant mothers. Presently, there is a shortage of health promotion media for PMTCT, which include both electronic and print educational media. Therefore, the implementation of HIV testing in Indonesia is mandatory for pregnant mothers at their first antenatal care (ANC). However, despite the importance of conducting this test before labor, there is no regulation to ensure its implementation.
Conclusion:
The success of HIV mitigation is closely associated with the participation of academicians, policymakers, and community networks in providing collaborative planning strategies for the reduction of its spread, and evaluation of the mitigation result.
1. INTRODUCTION
The transmission of the Human Immunodeficiency Virus (HIV) from mother to child has become a significant challenge in developing countries [1, 2]. Despite the use of antiretroviral prophylaxis, safe obstetric practices and breastfeeding habits, there is still a high prevalence of mother-to-child transmission (MTCT) [3, 4]. The Prevention of Mother-to-Child Transmission of HIV/ AIDS (PMTCT) has been a mainstay for over 20 years, thereby optimizing prophylaxis implementation [5].
HIV-positive pregnant mothers are likely to transmit the virus to their babies during labor, delivery, or through breastfeeding [6, 7]. It is relatively 15 to 45% risky for those that do not receive any treatment [8, 9]. The risk associated with pregnancy and labor or delivery is approximately 15 to 30%, while that of breastfeeding and puerperal is 10 to 20%. The prevention of mother-to-child transmission (PMTCT) by providing antiretroviral (ART) therapy to HIV-positive pregnant mothers is an effective intervention [10]. In addition, when administered consistently, it reduces the risk of vertical HIV transmission [11] to less than 5% [8].
The Prevention of Mother-to-Child Transmission (PMTCT) has been a concern to the Indonesia's government since 2004. PMTCT including Maternal and Child Health (MCH) Service was carried out through integrated antenatal services at the first level health facilities [12, 13]. The government's concern for pregnant mothers is stipulated in the Regulation of Health Minister of Republic of Indonesia Number 52, year 2017. It is centered on the prevention of mother-to-child transmission of Human Immunodeficiency Virus, Syphilis, and Hepatitis B. This regulation aims to eliminate communication and reduce morbidity, disability, and mortality rates. It also offers the central and regional governments, health workers, and other stakeholders guidelines to implement transmission elimination [14]. Besides, one of the targets of the third SDG is to end the transmission of AIDS, tuberculosis, malaria, hepatitis, neglected tropical, water-borne, and other infectious diseases [15].
PMTCT has proven to be an extremely effective intervention mechanism to improve maternal and child health. Even in developed countries, the risk of mother-to-child transmission has reduced to less than 2% because it is readily available and optimally implemented. In contrast to developing countries, with minimal access to these services, the risk of transmission ranges from 25% to 45%. The common knowledge and information regarding mother-to-child transmission indicates that 1%, 39.0%, and 37.4% or 38% of the population are aware of the fact that HIV/AIDS is transmitted during pregnancy, childbirth, and while breastfeeding, respectively [16].
In Indonesia, efforts to combat the spread of HIV infection have also been encouraging, although several aspects still need to be addressed. These include 1) the need to create awareness concerning HIV infection, modes of transmission, and prevention, 2) increasing the number of tests in the community, 3) rendering integrated HIV services, rather than separate and exclusive programs, thereby reducing the risk of the stigma 4) ensuring that all health workers and scientific disciplines understand the efforts to combat this infection, 5) ascertaining the even distribution of HIV testing and ARV drugs in the entire community, 6) optimizing the private sector’s role in countermeasures.
Preliminary studies on obstacles encountered in the TB/HIV program stated that factors, such as policies, facilities, finance, level of the health care system, lack of awareness and human resources including clients and health workers, influence the Prevention of Mother-to-Child HIV Transmission application [17, 18]. However, 38.2%, 39.0%, and 37.4% of the population is aware that this virus is transmitted from mothers to babies during labor, delivery, and breastfeeding, respectively [19].
Negative labeling (stigma) is one of the common factors that instills fear in pregnant mothers in terms of determining their HIV status [20]. Furthermore, it has an adverse impact on treatment adherence and it decreases retention care [21, 22], as well as causes depression [23]. However, their perception of low risk is the most significant barrier to HIV testing [24]. The research carried out in India also stated that 85% of pregnant mothers objected to voluntary HIV testing due to fear of knowing their status, reaction from husbands, parents, and the society [25,26]. Therefore, the stigma related to HIV results in depression [23]. HIV testing is essential and needs to be performed on pregnant mothers in anticipation of its transmission. PMTCT needs to be encouraged irrespective of the several challenges and obstacles [17, 27].
Based on WHO's recommendation, one of the implementations of HIV transmission elimination is carried out through health promotion designed to encourage people to undergo HIV testing. Its significance in preventing mother-to-child HIV transmission affects the target group's behavior and attitudes [28]. Technology also facilitates the search for health information, which results in positive attitudes [29]; also, accompaniment is essential in terms of encouraging one to take HIV testing [30].
Several studies on Antenatal Service (ANS) standards are related to pregnant mothers' HIV counseling and testing participation. Moreover, some discuss the obstacles related to the prevention of mother-to-child HIV transmission programs during antenatal care examination at the public health center [31]. In Indonesia, it is called Pusat Kesehatan Masyarakat or Puskesmas. This research examines the implementation of the prevention of mother-to-child HIV/AIDS transmission programs carried out at the Public Health Centers based on the perspectives of several doctors and midwives.
2. MATERIALS AND METHODS
The phenomenology approach was used to carry out this qualitative research. The semi-structured interview was carried out to obtain information on policies and implemented programs to prevent mother-to-child HIV/AIDS transmission at public health centers, namely Kretek, Kalibawang, and Gamping, all in Yogyakarta, Indonesia. These three were determined by the Department of Health as those in the HIV vulnerable areas. They render services related to HIV to pregnant mothers.
This research involves 6 participants consisting of 3 heads of public health centers and 3 midwives responsible for managing the HIV/AIDS programs. The participants attended socialization or training initiatives related to the Prevention of Mother-to-child HIV transmission. A purposive sampling technique was applied in this study. A midwifery lecturer, who had attended qualitative research training and is currently pursuing a doctorate program at Gajah Mada University, was chiefly responsible for conducting the interview. The participants were properly informed about the research objectives. They were also informed about the interviewer’s background. Only participants that willingly gave their consent were interviewed. Although 6 of them were selected for the interview process, none refused to be interviewed.
Interviews were carried out face-to-face in one of the public health center rooms with only the participants and interviewers present; besides, the in-depth technique was adopted. Subsequently, an interview guide and a voice recorder were used and field notes concerning certain occurrences, expressions, and responses were taken. In-depth interviews were only carried out once for each participant, and this lasted for approximately 45 minutes.
Interviews with participants were stopped when there was data saturation. This simply implies when the informant repeatedly gives similar answers. Triangulation of midwives' sources and those of the public health centers was performed by analyzing the antenatal care examination form and HIV/ AIDS flow during pregnancy checks.
The demographic data of each participant was also collected, such as age, group, work duration, and the interviewing time. Table 1 shows the participants’ characteristics.
| Code | Age (Year) | Group | Education | Work Experience (Year) |
|---|---|---|---|---|
| P1 | 53 | Midwife | Diploma III of Midwifery | 3 |
| P2 | 44 | Midwife | Diploma III of Midwifery | 10 |
| P3 | 31 | Midwife | Diploma III of Midwifery | 9 |
| P4 | 42 | Head of PHC | Dentistry | 6 |
| P5 | 47 | Head of PHC | Dentistry | 8 |
| P6 | 52 | Head of PHC | Dentistry | 6 |
The doctors and midwives used in this research have been heads of public health center and HIV counselors for approximately 6 and 3 years, respectively. The questions for directors were related to the PMTCT program implementation. This was aimed to discover the midwife’s knowledge of this initiative from the doctor’s perspective, the training format, and the questions related to the recommended intervention scheme for pregnant mothers in the prevention of mother-to-child HIV/AIDS transmission. The purpose of midwives' interview was to identify the PMTCT program's implementation impact on the patients’ HIV knowledge based on their point of view in order to discover the training recommendations related to the program and advice on appropriate intervention for pregnant mothers.
The data was analyzed using Creswell's approach. This was carried out in 3 stages, namely by saving data in the folder file, transcribing, and analyzing it manually [32] using both the theme and sub-theme, as shown in Fig. (1).
3. RESULTS AND DISCUSSION
3.1. Theme 1: Policies on Mandatory HIV Testing for Pregnant Mothers as a Vulnerable Group
Identifying HIV-positive pregnant mothers through routine screening is an essential step to initiate the PMTCT intervention. Therefore, it is recommended by the current guidelines related to HIV transmission [33, 34]. According to preliminary studies, HIV testing is mandatory for pregnant mothers, hence the probability of refusal is beyond question [35]. It simply means that HIV testing is a mandatory program in pregnancy examination. The following are excerpts from participants 3, 4 and 5.
Participant 3, midwife- (…presently HIV testing service for pregnant mothers is a mandatory priority. This is based on the fact that they are all categorized in the vulnerable group…)
Participant 5, head of the public health center- (…all pregnant mothers take HIV testing and its services are smoothly run. During their work experiences, no one tested positive)
Participant 4, head of the public health center- (... Everyone exposed to the risk of being infected with HIV gets health services after being referred to the standards provided by the Regency or City Government in their working area within a year according to Regulation of the Minister of Health Number 4 of 2019 concerning Technical Standards for Fulfilling Basic Service Quality in the Minimum Service Standards in Health Sector...).
Further, it was stated that every pregnant woman needs to be screened because they are exposed to HIV risk. This understanding was not thoroughly agreed upon by the health personnel. However, the informant from the Bantul District Health Center considered the fact that every pregnant woman is highly exposed to the risk of contracting HIV. A representative of the head of Public Health Division of the Sleman Health Office further explained that it was not entirely ascertained that pregnant mothers belonged to the group of those at high risk of HIV, therefore it was still dualism, although when referred to the Ministry of Health Regulation (MOHR) No. 4 Year 2019, they have been included in this category. The difference in defining pregnant mothers as a risk group among health workers is pursued by socializing MOHR No. 4 Year 2019. This is to create a common perception that they are among those at risk of HIV and early detection through blood tests needs to be performed at least once during pregnancy; this reinforces the importance of re-testing.
The participants further explained that the implementation of HIV testing for pregnant mothers is part of a government program, as reported in the following excerpt.
Participant 1, midwife (…HIV testing service, especially for pregnant mothers, is integrated into ANC (pauses), almost all are approved, and until date, no one has ever refused to undergo such tests. However, assuming the patients have already taken the HIV testing at another place, there is no need for retesting…).
Participant 2, midwife (... this HIV test is included in the antenatal care program with 10T services, one of which is the screening aspect).
Participant 3, midwife (…HIV testing services for pregnant mothers use the PMTCT method, which is based on health workers' initiatives. Screening is carried out because it is included in the integrated ANC, therefore all pregnant mothers are mandated to take HIV testing...).
PMTCT is a global public health priority [35] because Mother-to-child HIV Transmission (MTCT) occurs in at least 1 out of every 10 pregnant mothers that are positive irrespective of the optimized programs such as prophylaxis for prevention [36]. The success of HIV/AIDS mitigation is inseparable from academicians, policymakers, and community networks, collaborating in terms of adopting strategies for cubing the spread of this infection, and evaluating the mitigation result [37, 38]. The government needs to strengthen the health care system by creating competent human resources to ensure that every pregnant woman is screened for HIV. The 12.5% increase requires at least 4 ANC visits at the appropriate schedule [39].
3.2. Theme 2: Importance of Enhancing Pregnant Mother’s Knowledge of HIV/AIDS
Awareness empowers individuals and couples to access information concerning HIV prevention [33, 40, 41]. Knowledge of their status enables them to access the prevention of mother-to-child transmission (PMTCT) [33]. Someone with primary education finds it difficult to read articles or understanding scientific terms, which leads to inadequate information regarding MTCT [42]. A literate with good knowledge of HIV is associated with better health outcomes [43]. This also affects the implementation of Voluntary Counseling and Testing (VCT). A study carried out in India also reported that 85% of pregnant mothers objected to voluntary HIV testing because of fear of disclosing their status and reactions from their husbands, parents, and society [25, 26]. Knowledge and awareness of HIV/ AIDS are the main factors influencing risk perception, and behavior, preventive methods, testing, treatment-seeking and after diagnosis attitudes, as well as an enabling environment for victims [44].
Several factors influence knowledge related to HIV; for example, socio-demographic characteristics, such as age, education, and religion, are closely related to mothers’ comprehensive awareness of HIV [45]. Higher income and education lead to extensive HIV experience compared to a poor means of livelihood [46]. The midwives explained that internal factors, such as educational background and less exposure to health information, cause ignorance as reported in the following excerpt.
Participant 1, midwife (…In relation to this, patients with senior high school educational background or lesser were initially asked about their HIV/AIDS knowledge. However, assuming they lacked understanding about this disease, then it was further explained…).
Participant 2, midwife (…many people do not understand this virus. They only know that HIV is an infectious disease and they need to get tested, in order to know their status…).
Participant 3, midwife (... pregnant mothers’ knowledge of HIV has never been measured by a questionnaire, however during counseling, it was described as a deadly and frightening disease...).
Inner perception is the process of organizing and interpreting sensory information to make it meaningful [47]. This factor causes mothers not to take an HIV test [26, 48-50].
Personal attitudes and subjective norms play a role in a person's health behavior, especially HIV testing. Overall, the majority of mothers with good intentions showed a positive response towards PMTCT [51]. Also, knowledge is related to pregnant mothers’ behavior in using these services [52-54].
Younger mothers are often inexperienced and have less knowledge of PMTCT, therefore they need more support and instruction regarding Provider-initiated HIV Testing and Counseling (PITC) [55]. Health promotion provides insight into the importance of preventing HIV transmission in pregnant mothers [56]. The participants further stated that external factors negatively influence pregnant mother’s knowledge, such as limited health promotion media and the midwives inability to handle many patients, in terms of offering detailed information about HIV, as stated in the following excerpt:
Participant 1, midwife (…however, the highly educated patients, usually understand, through (pause) television, and other information media...).
Participant 3, midwife (…detailed knowledge of HIV is never offered to pregnant mothers, (pause) until there is feedback. They are only taught its definition…because there are too many factors that need to be considered, although (pause) high-risk patients are usually counseled…).
Health promotion methods used to improve PMTCT service delivery include peer mentoring, text messages, and invitation cards during pregnancy to allow expectant mothers and their partners to take an HIV test as well as home visits [57-60]. It is evident that mothers are usually motivated to cope with health problems during the postpartum period, leading to behavioral changes during this transition [61]. The existence of technology supports the search for health information and also has a positive influence on the mothers’ behavior [29].
The widespread use of technology, such as smartphones, television, and the internet, and a higher literacy level at the antenatal clinics cause health awareness campaigns, HIV testing, and PMTCT services to become easily accessible to those in the cities compared to the villages [62]. Coverage service is an essential strategy adopted to reach out to mothers in the communities. Health education is also necessary to modify cultural norms and lessening the probability of avoiding HIV testing by pregnant mothers [33].
Mothers’ immense knowledge influences their attitudes towards accessing information concerning HIV prevention [41]. Meanwhile, those with only elementary education find it difficult to read articles or understand scientific terms, thereby resulting in a lack of adequate information regarding MTCT [42]. The ones with functional literacy or HIV knowledge are related to a better health outcome [43]. It also influences the implementation of Voluntary Counseling and Testing (VCT). Another factor that prohibits pregnant mothers from taking VCT is stigma [21]. Its adverse effects influence obedience to HIV treatment and reduce retention [22]. This is because certain internal and external factors tend to affect one's knowledge. Therefore, it is important to enhance pregnant mothers’ knowledge of HIV/AIDS.
3.3. Theme 3: Need for PMTCT Training Especially Prongs 3 and 4
According to WHO, PMTCT materials comprise of 4 prongs. Some tend to prevent mother-to-child HIV transmission and offer care and support to the victims and their families [17, 63]. This theme further illustrates the need for PMTCT training with respect to Prongs 3 and 4. The midwife explains the materials related to HIV/AIDS prevention during labor or delivery. Health professionals who attend PMTCT training become highly skilled and confident after the practice [64].
Participant 3, midwife (…training materials associated with preventing mother-to-child transmission (PMTCT), during labor or delivery, (pause) are explained using prong…).
Participant 5, head of the public health center (…thinks impressive HIV materials are similar and need to be delivered quickly, although there is also a need for the most recent data on PMTCT…).
Participant 6, head of the public health center (... the midwives have been trained on HIV, however to deepen their understanding of the materials on preventing its transmission from the mother to the fetus, it is necessary to ensure they are updated especially in terms of the psychological support, due to the stigma associated with the victims...).
The participants also need materials and training on stigma and family support, as reported in the following excerpt.
Participant 1, midwife (...training materials about HIV/AIDS are (pause) based on the fact that this disease is horrifying, initially people are scared, and it gets harder supposing the patient does not want to open up to her family, which is easy...).
Participant 6, head of the public health center (…in a region with certain cultural specificity, people need to be aware of such social culture, therefore it is important to be caring...).
Preliminary research carried out in Sub-Saharan Africa revealed that psychosocial factors are related to depression signs, poor social support [17], and stigma, even though these are moderate for HIV-positive pregnant mothers [23]. However, at least 30 days after the diagnosis, 11.9% of mothers were ignorant of their HIV status. They consider societal gossip and stigma as barriers to the disclosure of their serostatus [65]. HIV-positive mothers are affected by different social implications, including stigma from within the family [66]. Also, assuming it occurs in adolescents or young people, they tend to cover up their health problems for privacy reasons [67].
Besides, for health workers to meet societal needs, they have to possess good communication skills as well as be properly informed to reduce this stigma [68]. The acceptance rate of HIV testing and counseling is relatively high. Therefore, the active use of a case-finding model and advices sufficiently increases testing [69]. Peer-intervention is a primary preventive measure in resolving adolescents’ problems [70].
3.4. Theme 4: Factors of Infrastructure and Facilities
The infrastructure and facilities are associated with the regional government policies on reagent procurement and need support of the Department of Health or local government. This was supported by the data obtained from the participants.
Participant 4, head of the public health center (…for the implementation of HIV testing, public health centers in the regency used the regional government budget...).
Participant 6, head of the public health center (…they were all prepared for implementing HIV testing because it is one part of their daily routine. The department of health further stated that it is vital, although the reagent needs to be ready. This has not been implemented to the Minimum Service Standard yet because it involves all community members. The public health center is undoubtedly not capable of rendering that service. Therefore, it needs supports from the department of health…).
Some other comments from the participants on competent human resources factor reported that a qualified counselor is one that is able to cope with social-cultural aspects as well as handle HIV prevention in societies.
Participant 5, head of the public health center (…according to midwife Y (pause), the capability of a counselor (pause), in my opinion, is competently creating awareness, such as handling previous HIV-negative cases…).
Participant 6, head of the public health center (…the capability of a counselor (pause) in their opinion, is competency because they have been trained severely, and as (pause) a worker and trained personnel for HIV related activities, midwife S is good at social-cultural stuff, which involves ritual area spots such as those on Tuesday. They indirectly influence the sex workers’ transactions...).
During antenatal and postpartum care, routine counseling is an important way of delivering HIV/AIDS related information to the mothers and encouraging them to go for tests [30]. This helps expectant mothers to make informed choices and adopt appropriate preventive methods [71]. The counselor's roles in relieving patients' fear of taking HIV testing as well as offering psychological support, before and after the examination, aids to sustain the patients’ emotional stability even after receiving positive results [72, 73]. The interview also revealed that lack of PMTCT promotion is related to electronic and printed educative media, as reported in the following excerpt [33].
Participant 1, midwife (…for health promotion media, leaflet, don’t make it too big. The insertion of several pictures makes it attractive. Even till date, patients are educated with an LCD projector. Sometimes the person responsible for its setup finds it challenging. Using a leaflet helps a lot...).
Participant 3, midwife (… for health promotion media, leaflets are usually used, although these are seldom given to the pregnant mothers …).
Participant 6, head of the public health center (… animation videos are promoted by installing the app on the patients’ tablets or handphones...).
Support for HIV prevention needs to be carried out with a holistic approach encompassing behavioral, biomedical, and structural interventions [74]. UNAIDS (Joint United Nations Programme on HIV and AIDS) defines this combination as right-based, evidence-informed, and community-owned priority to meet the current preventive measures of particular individuals and regions. In addition, it offers the most significant sustained impacts in terms of reducing new cases of infection [74]. Donors primarily fund HIV programs and are supported by communities [68]. This funding type is temporary, therefore its sustainability requires the attention of the policymakers. Previous research stated that funding tends to be a severe problem or obstacle in utilizing these services [72]. This theme is also centered on the comments about the education room that is not yet optimal.
Participant 4, head of the public health center (…is it because the room is inadequate, or only 2 persons are in charge of the services? 1 of them is responsible for dealing with Family Planning, while the other is in charge of ANC. The ground floor is reorganized into 3 rooms, thereby providing privacy for high-risk counseling...).
Participant 5, head of the public health center (…Patients receive an explanation of HIV in the same room used for pregnancy examination because it is integrated with ANC…).
Health service providers reported that counseling is essential for HIV-positive pregnant mothers. On the contrary, it is not prioritized for most people that test negative because primary preventive opportunities are missed. Counseling pretest is essential for pregnant mothers to ensure that they understand the implications of negative or positive test results on themselves, their spouses, and unborn children.
3.5. Theme 5: Need for HIV Retesting for Pregnant Mothers
HIV testing is essential because it offers intervention access in terms of preventing mother-to-child transmission, especially in high-risk communities [75]. It is transmitted from mother to child assuming the service providers are not aware of the pregnant mothers’ status and do not recommend antiretroviral therapy for HIV-positive patients [76]. However, in Indonesia, HIV retesting has not been carried out because the enacted regulations have not explicitly stated its testing during pregnancy. The following are some statements from the participants regarding HIV retesting.
Participant 1, midwife (... there is no HIV re-testing for pregnant mothers, except for those with risky behavior, however it is considered necessary. Miss ... because there is a phase known as the window period at which sometimes the test results tend to be negative, when in the actual sense, the patient is HIV positive...).
Participant 3, midwife (…HIV retesting for pregnant mothers is not implemented yet, Miss; they need to be retested before labor or delivery, Miss…).
Participant 5, head of the public health center (…HIV retesting for pregnant mothers has not been implemented (pause), despite being necessary…).
The implementation of PMTCT in Indonesia is mandatory and has to be performed only once at the first ANC. Even though in the flowchart of counseling and HIV testing from the Ministry of Health (MoH), Republic of Indonesia, there are procedures mandating health workers to encourage patients to go for retesting, particularly those with high-risk behaviors, including pregnant mothers. However, this system is yet to be implemented, probably because the regulation is not specific to HIV examination during pregnancy. The data shows that HIV testing on pregnant mothers is only carried out once. Moreover, there is no specific form of screening high-risk behaviors such as those associated with taking VCT. Conversely, HIV retesting and initiation of early ART are essential components in ANC in terms of identifying and managing high HIV incidents as well as initiating treatment for infected pregnant mothers to prevent prenatal transmission and keep the mothers alive [18]. Moreover, HIV retesting aims to ensure the sustainability and success of the PMTCT program [77].
Based on preliminary research carried out in India, HIV retesting is 8.2 times more cost-effective compared to the quality-adjusted life-year (QALY). This is a general measurement of illness burden and life quality [78]. Preliminary research carried out in Uganda shows that it is highly acceptable and visible, with 82% of the respondents taking more than one HIV testing during pregnancy. Therefore, HIV retesting for pregnant mothers, particularly those at high risk, needs to be visibly implemented, especially when the expectant mothers have good knowledge of the virus [79].
Local governments with autonomy in budget spending are able to prioritize health programs. An example is the Sleman Regency which already has a regional government budget for handling HIV. However, HIV testing policy in this regency is still performed once for all expectant mothers, particularly during their first pregnancy visit. However, the regional government budget independently manages HIV treatment, and there is an opportunity that it is implemented twice during pregnancy considering its high rate of transmission in the Special Region of Yogyakarta, which is ranked as the second out of the 5 districts.
The results of this study are consistent with some research that reported the supporting factors for retesting HIV,including government policies, integration of HIV testing with ANC, and active roles of health workers in educating and reminding when to go for retesting. In addition, there are inhibiting factors, including the pregnant mothers’ perceptions, and failure to disclose their status to their partners [34].
CONCLUSION
The implementation of PMTCT in Indonesia is mandatory and only carried out once at the first ANC. The success of HIV/AIDS mitigation relates to academicians, policymakers, and community networks that collaborate in adopting strategies to reduce the infection, as well as evaluate the results. Even though HIV retesting seems necessary, at this time, presently, there is no regulation for its implementation.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was issued by the Medical and Health Research Ethics Committee (MHREC), Faculty of Medicine, Public Health and Nursing, Gadjah Mada University, Indonesia, under Ref. No. KE/ FK/ 1089/ EC /2019 on September 26, 2019. The amendment of this clearance was made due to a change in research location on April 3, 2019. It also obtained an extension of implementation through new ethical committee approval from the same institution as Ref. No. KE/ FK/ 1202/ EC/ 2020, dated 4th November 2020.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all study participants.
STANDARDS OF REPORTING
COREQ guidelines and methodology were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used during the current study can be obtained from the corresponding author [D.A], upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors are grateful to the Department of Health, Yogyakarta Province, and the Public Health Centers' management for facilitating this research.


