All published articles of this journal are available on ScienceDirect.
Pain Assessment and Management in Intensive Care Unit: Nurses' Practices, Perceived Influencing Factors, and Educational Needs
Abstract
Background:
Critically ill patients and those mechanically ventilated or unable to communicate may not be able to report any pain they experience. Consequently, pain assessment and management (PAM) is challenging and underestimated in intensive care units (ICUs), where patients suffer alteration of consciousness, sedation, invasive procedures and mechanical ventilation.
Aim:
This study aimed to investigate ICU nurses’ PAM practices, their perceptions of influencing factors, and their related educational needs.
Methods:
A descriptive cross-sectional design was employed, using a valid self-reported questionnaire.
Results:
Among the sample of 171 nurses, 55% were male and 83% held a bachelor’s degree. 60% reported performing pain assessment for patients able to report pain and 50% for those unable to do so. Almost 40% of participants reported that pain management plans and scores were not discussed in medical rounds. Workload and lack of guidelines were reported as the most common barriers to PAM, while the most common enablers were perceived to be prescribing analgesia and considering pain a priority. Nurses recognized the need for education regarding pain, especially the physiological (50%) and psychological (47%) consequences of untreated pain.
Conclusion:
Nurses’ reported performance of pain assessment for ICU patients remains suboptimal. Therefore, healthcare professionals, organizations, nursing schools, and policymakers should work together to improve nurses’ PAM knowledge and practices.
1. INTRODUCTION
Pain is one of the most common problems in Intensive Care Units (ICUs) and in treating critically ill patients, regardless of their underlying diseases [1]. It is also considered one of the most significant stressors of critically ill patients [2]. It is reported that almost half of critical care inpatients experienced pain during rest and procedural interventions [3], that 45% to 82% of patients in ICU experienced moderate to severe pain [4], and that more than half experienced untreated and persistent pain after discharge [5]. In Jordan, ICU patients were found to have moderate pain at rest and severe pain during nursing procedures [6].
Pain is purely a subjective measure, so patient self-report is the most reliable method to assess and explore it. However, critically ill patients and those mechanically ventilated or unable to communicate are not able to report any pain that they may be experiencing. Consequently, there is a challenging and underestimated problem in estimating pain resulting from alteration of consciousness, sedation, invasive procedures [7], and mechanical ventilation [8]. Undertreated pain can result in unfavorable complications in respiratory and cardiac functions, thus augmenting morbidity, mortality, and healthcare costs [6] and lengthening hospital stays [4]. In contrast, pain assessment systematically improves patients’ outcomes, thus reducing duration of mechanical ventilator support and length of hospital stay [8].
Elimination of patients’ pain and suffering is an important responsibility of healthcare professionals (HCPs) [9, 10]. In ICUs, nurses play a key role in assessing and treating patients’ pain, by systematically monitoring pain levels, choosing and administering the appropriate treatment including non-pharmacological pain management interventions, educating patients and their families about pain, and advocating for patients [11]. Critically ill and mechanically ventilated patients rely strongly on nurses to alleviate their suffering and symptoms by understanding undesirable experiences including pain, anxiety, and delirium and by identifying the symptoms associated with pain [12]. Therefore, a principal aspect of nurses’ execution of the treatment plan for non-communicating or mechanically ventilated patients is to use the appropriate tools to assess their pain levels [6]. Moreover, accurate pain assessment improves its management, making assessment a key element of pain management in ICU patients. In summary, the use of appropriate pain assessment tools and documentation of pain levels help to improve understanding of pain levels in ICU patients, to enhance pain management, and to reduce undesired effects and complications [13].
Despite the attention of many researchers and healthcare institutions globally, however, pain management remains deficient, as about 50% of ICU patients continue to experience pain [3]. Among the factors obstructing ICU nurses in assessing and managing pain adequately are barriers related to patients, to nurses themselves, and to hospital policies, such as the persistence of traditional conceptions of pain and suffering, nurses having no authority to administer analgesia, the absence of special forms for assessing pain in intubated patients, lack of knowledge, physicians’ mistrust of nurses’ assessment, and inadequate psychosocial support services [14].
ICU patients in Jordan have been found to suffer moderate to severe pain and not be well satisfied with pain management [15]. Meanwhile, given nurses’ role as the HCPs most closely involved in pain management, their practices are key to its success. Furthermore, obtaining baseline data regarding nurses’ practices in Pain Assessment and Management (PAM) for ICU patients is a significant step in managing their pain effectively, thus enhancing their Quality of Life (QoL) and reducing hospitalization periods and emergency visits [16, 17].
Pain assessment and management is a topic of wide interest to HCPs and healthcare institutions not only because of its significant effect on the QoL of patients and their families, but also because it is considered an accreditation requirement. Moreover, improving HCPs’ practices in this field, participating in scientific research, and keeping up to date with modern science are all required to achieve optimal patient care [18, 19]. Thus, there is value in obtaining information about nurses’ PAM practices—both generally and in ICUs—and in exploring the factors that affect their success in this process, in addition to identifying their educational needs.
Identifying the current PAM practices, barriers and enablers from nurses’ point of view would help in exploring areas of deficit in order to guide healthcare administrators and policymakers in their planning and in seeking solutions to any such obstacles. Recognizing the great importance of nurses’ curricula and educational programs [9, 20], it is also hoped that this study will encourage nursing schools and in-service education departments to sharpen the focus of their curricula on pain-related topics and that it will shed light on specific areas of educational need.
It must be borne in mind that pain perception is culturally sensitive and that nurses’ behaviors and practices in PAM are influenced by culture [21, 22]. Therefore, researchers recommend that exploring HCPs’ knowledge of and attitudes to pain in multiple countries is required in order for any conclusions to benefit from a variety of perspectives. In particular, this study addresses the perspective of Jordanian nurses on PAM in ICUs, by investigating their practices, their perceptions of barriers and enablers, and their related educational needs.
2. METHODOLOGY
2.1. Research Design
A descriptive cross-sectional design was used to evaluate ICU nurses’ PAM practices, their perceptions of influencing factors and their related educational needs.
2.2. Population
All Registered Nurses (RNs) meeting the inclusion criteria and working in an ICU at the time of data collection were considered to constitute the accessible population.
2.3. Sample and Sampling
The sample comprised RNs, being the HCPs who engage in assessing and managing pain in ICUs. Inclusion criteria included being an RN, being able to write and read English, and currently having worked in an ICU for at least three months, a period long enough to orient nurses well toward new work. The sample size was calculated using G-power V.3.1 with alpha = 0.05, moderate effect size (0.25), and power = 0.85, applying an ANOVA test among four groups, corresponding to the governmental, educational, private, and military sectors into which the Jordanian healthcare system is divided. This calculation yielded a sample size of 190, to which ten percent was added to compensate for participants’ attrition, increasing the sample to 210 participants.
2.4. Settings
All hospitals in the four main sectors of Jordanian healthcare have ICUs. From the governmental sector, Al-Basheer Hospital and Prince Hamzah Hospital were included as having the largest bed capacity. The Islami and Al-Khaldi hospitals were selected from the private sector for the same reason. Jordan has only two educational hospitals, Jordan University Hospital and King Abdullah University Hospital, both of which were also involved.
2.5. Instrument
The instrument used in this study consisted of two parts. The first was a demographic survey developed by the researcher and comprising 11 items on age, gender, level of education, hospital settings, length of experience as a nurse and in ICU work, any previous formal or informal training in pain management, and work experience in a pain team. It also sought information on the patient ratio and bed capacity of the participant’s current ICU.
The second section was a version of the Survey of Perceived Pain Assessment and Management Practices for Patients Able and Unable to Self-Report Pain developed by Rose and colleagues [7]. This questionnaire, designed to assess nurses’ practices in PAM for critically ill patients, consists of 36 items on pain assessment practices for patients both able and unable to self-report pain, the perceived importance and frequency of pain assessment, factors affecting the PAM process, enablers and barriers, and nurses’ PAM-related educational needs [7]. Permission to use the tool was obtained from the original author, who agreed to its modification to ensure relevance to the Jordanian settings. The internal consistency reliability and content validity of the modified tool were established by the original researchers. The item content validity index and scale-level content validity was 0.90 [7]. The present researcher conducted a pilot study to ensure that the culturally adapted instrument was valid for use. Thirty nurses from different settings, all meeting the inclusion criteria, were invited to complete the questionnaire after reading the cover letter carefully. The Cronbach’s alpha value of the modified tool was 0.84.
2.6. Data Collection Procedure
Once the necessary ethical approvals had been obtained, as detailed below, the primary researcher arranged a meeting with the nursing administration at each site to explain the purpose of the study and to determine the method of approaching potential participants most appropriate to each selected hospital. Accordingly, posters and flyers were displayed to encourage nurses to participate. In addition, the questionnaires were discussed with the head nurse of each ICU, then the research assistant invited nurses meeting the inclusion criteria to participate in this study by filling the questionnaire, which was returned in a closed envelope.
2.7. Ethical Considerations
Before the study began, ethical approval was sought first from the Ethical and Scientific Committee at the Faculty of Nursing in the University of Jordan, then from the Institutional Review Board of each participating hospital. Potential participants were informed that they had the right to accept or refuse to participate in the study and to withdraw at any time. Identification of individual participants was not a requirement of the study; therefore, anonymity was ensured. After receiving a full explanation of the study and assurances of their freedom to choose whether or not to participate in it, nurses who agreed to do so signed the consent form without the need to state their names. All data was handled confidentially and only the primary investigators had the authority to view it.
2.8. Data Analysis
The SPSS software package (version 23.0) was used to code and analyze the survey data. Descriptive statistics such as mean and frequency were used to analyze the demographic characteristics of the sample. Means and standard deviations were applied to answer the first research question, concerning the PAM practices of Jordanian ICU nurses, while frequency and percentage were used to address the questions about perceived barriers and enablers and nurses’ educational needs.
3. RESULTS
Of the 210 questionnaires distributed, 171 were returned and included in the analysis, a response rate of 81.4%. The age of the participants ranged from 23 to 45 years, with a mean of 30.3 (SD=4.7). Their general experience ranged between 3 months and 20 years with a mean of 6.8 (SD=4.2) and their ICU experience ranged from 3 months to 18 years with a mean of 4.8 (SD=3.6). There were slightly more males (n=94; 55%) than females. The majority of participants had bachelor’s degrees (n=142; 83%). Precisely two-thirds (n=114; 66.6%) had no PAM training and 151(88.3%) had no experience in a pain management team. More than half of participants (n=98; 57.3%) were recruited from public hospitals. Nearly two-thirds (n=106; 62%) were working in mixed ICUs and the most frequent (n=117; 68.4%) nurse-to-patient ratio in the participating units was 1:>2. Table 1 gives details of participants’ characteristics.
| Domain | n(%) |
| Hospital | |
| Public | 98(57.3) |
| University | 20(11.7) |
| Private | 53(31) |
| Gender | |
| Male | 94(55) |
| Female | 77(45) |
| Education level | |
| Bachelor | 142(83) |
| Postgraduate | 29(17) |
| Intensive care unit | |
| Medical | 15(8.8) |
| Surgical | 38(22.2) |
| Neuro | 7(4.1) |
| Mixed | 106(62) |
| Nurse-to-Patient ratio | |
| 1:01 | 8(4.7) |
| 1:02 | 46(26.9) |
| 1:>2 | 117(68.4) |
| Pain training | |
| Yes | 57(33.4) |
| No | 114(66.6) |
| Pain team experience | |
| Yes | 20(11.7) |
| No | 151(88.3) |
| M(SD) | |
| Age | 30.2(4.7) |
| General experience | 6.8(4.2) |
| ICU experience | 4.8(3.6) |
3.1. Pain Assessment and Management Practices
For patients able to report pain, only about half of participating nurses (n=92; 53.8%) believed that the person most accurately reporting its severity would be the patient, while the remainder wrongly believed that assessment by physicians, nurses, and relatives would be more accurate. Pain assessment tools were used by 103 nurses (60.2%) and the most commonly used was the numerical rating scale (n=49; 28.7%), while 102 participants (59.6%) had used more than one tool. Nurses reported that they frequently used pain assessment for these patients, with a mean score of 3.4 (SD=1.2) out of five. They perceived it to be important to use a tool for pain assessment, with a mean score of 3.8 (SD=1.1). As to the frequency of assessment, the highest percentage was the 28.1% (n=48) who reported assessing pain for stability every four hours; they perceived it to be important to assess and document patients’ pain, with a mean score of 3.7 (SD= 1.1).
Regarding patients unable to report their pain, three-quarters of nurses (n=129; 75.4%) believed that nurses could most accurately report a patient’s pain; nevertheless, about half of participants (n=85; 49.7%) reported not using a pain assessment tool for these patients. Where such tools were employed, the most commonly used were the FLACC scale (n=47; 27.5%) and the Critical-Care Pain Observation Tool (CPOT) (n=28; 16.4%); almost half of the nurses (n=84; 49.1%) reported using more than one tool. Furthermore, they reported frequently using a pain assessment tool for these patients, with a mean score of 3.3 (SD=1.2) out of five. Nurses perceived it as important to use such tools, with a mean of 3.6 (SD=1.2), and important to assess and document the pain, also with a mean score of 3.6 (SD=1.2), equivalent to 72%. Regarding frequency, 33 nurses (19.3%) reported assessing pain every eight hours and 26 (15.2%) every four hours. Table 2 shows more data on nurses’ pain assessment practice.
| Items | Mean (SD) |
| How frequently do you use a pain assessment tool for patients able to self-report pain? | 3.4(1.2) |
| How important is a pain assessment tool? | 3.7(1.1) |
| In your opinion, how important are frequent assessment and documentation of pain in patients able to communicate? | 3.7(1.1) |
| How frequently do you use a pain assessment tool for patients unable to self-report pain? | 3.3(1.2) |
| How important is a pain assessment tool for patients unable to self-report pain? | 3.6(1.2) |
| How important are frequent assessment and documentation of pain in patients unable to communicate? | 3.6(1.2) |
| How important is assessment of pain for the following classifications of ICU patient? | |
| Post-operative ICU patient | 4.1(1.1) |
| Medical (non-surgical) ICU patients | 3.5(1) |
| Patients with a GCS <8 | 3.4(1.1) |
| Trauma ICU patients | 4.1(1) |
| Burn ICU patients | 4.3(.95) |
| End-of-life ICU patients | 3.6(1.3) |
| Patients receiving sedatives | 3.3(1.3) |
| How important is assessment of the need for pre-emptive analgesia prior to the following procedures? | |
| Patient repositioning | 3.1(1.1) |
| Endotracheal suctioning | 3.1(1.2) |
| Wound care | 3.8(1) |
| Drain removal | 3.3(1.1) |
| Invasive line placement | 3.6(1.1) |
| Spontaneous breathing (weaning) trial | 2.9(1.2) |
| How frequently do you assess the need for pre-emptive analgesia prior to the following procedures? | |
| Patient repositioning | 3.0(1.1) |
| Endotracheal suctioning | 3.2(1.1) |
| Wound care | 3.5(1) |
| Drain removal | 3.2(1.1) |
| Invasive line placement | 3.4(1.1) |
| Spontaneous breathing (weaning) trial | 3.0(1.2) |
| How frequently is pain management plan discussed during nurse-to-nurse/ physicians-to-physician report (endorsement) | 3.3(1.1) |
| How frequently are pain scores discussed during nurse-to-nurse / physicians-to-physician report (endorsement)? | 3.3(1.1) |
| How frequently are pain management and pain scores discussed during medical rounds? | 3.1(1) |
| How frequently do physicians write orders for analgesia targeted to a pain score or other assessment parameters? | 3.4(1.1) |
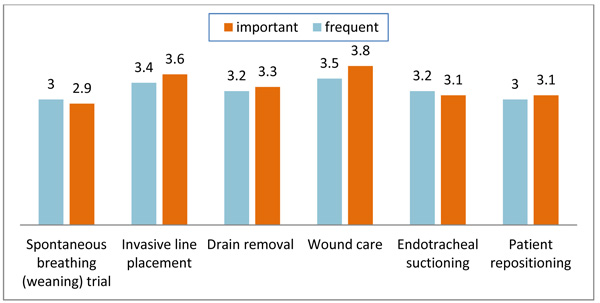
The data reveals that nurses perceived it to be most important to assess the pain of patients with burns, giving a mean score of 4.4 (SD=.95), followed by post-operative patients, scoring 4.2 (SD= 1.1). On the other hand, they accorded sedated patients the lowest priority, at 3.3 (SD=1.3). As to procedures, wound care was associated with the greatest need of assessment (mean=3.8; SD=1.0), whereas assessment was least important when weaning patients from mechanical ventilation (mean=2.9; SD 1.2). Responses to questions about nurses’ actual practices yielded similar results. They reported most frequently assessing pain when performing wound care (mean=3.6; SD=1.1) and least frequently when weaning from mechanical ventilation (mean=3; SD=.2). Fig. (1) compares nurses’ perceptions of the importance and frequency of pain assessment for the various procedures. Regarding pain management practices, the one reported as most frequent was the prescribing of analgesics by a physician in response to pain score (mean=3.4; SD=1.1) and the least frequent was discussing a pain management plan and the patient’s pain score during medical rounds (mean=3.1; SD=1.1).
3.2. Barriers to and Enablers of Pain Assessment and Management
Nurses perceived there to be marginally more enablers of PAM (mean=3.4; SD=.8) than barriers to it (mean=3.3; SD=.6). The two highest scores for enablers were for physicians’ prescribing of analgesics (mean=3.6; SD=1) and nurses’ belief about the priority of PAM (mean=4.5; SD=1.1), whereas the lowest were for hospital policy and services regarding pain consultation in the ICU (mean=3.1; SD=1.2) and using pain management guidelines (mean=3.2; SD=1.1). As to barriers, the highest scores were for high workload and time constraints (mean=3.6; SD=1), followed by unavailability of pain management guidelines (mean=3.5; SD=1.1), while the lowest were for the absence of a specific section for pain assessment in the nursing chart (mean=3.1; SD=1.3) and the fact that ICU professionals did not prioritize pain management (mean=3.1; SD=1.1). Table 3 gives details concerning PAM enablers and barriers.
| - | Mean(SD) |
| Enablers | - |
| Pain assessment and management is a unit priority | 3.5(1.1) |
| Enthusiastic and motivated staff | 3.4(1) |
| Standardized assessment tools are in use | 3.4(1.1) |
| Protocols and guidelines are in use | 3.2(1.1) |
| Physicians prescribe adequate doses of analgesia | 3.5(1) |
| Ongoing education on pain is provided | 3.3(1.2) |
| Advanced practice nurse(s) are employed by the ICU | 3.3(1.1) |
| Hospital pain service consults in the ICU | 3.1(1.2) |
| Barriers | - |
| Workload and lack time | 3.6(1) |
| Lack of availability of pain assessment tools | 3.2(1.1) |
| Lack of education/familiarity with assessment tools | 3.2(1) |
| Patient instability e.g. unstable hemodynamics | 3.3(.98) |
| Patient inability to communicate | 3.4(1.1) |
| Lack of protocols/guidelines for pain assessment | 3.3(1.1) |
| Low priority of pain management by ICU team | 3.1(1.1) |
| No designated area for charting pain | 3.1(1.3) |
| Sedation interfering with pain assessment | 3.4(1.1) |
| Poor documentation of pain assessment and management | 3.2(1) |
| Poor communication of pain and analgesic management priorities within ICU team | 3.2(1) |
| Lack of protocols/guidelines for pain management | 3.2(1.1) |
| Insufficient analgesia dosage prescribed | 3.2(1.2) |
3.3. Educational Needs Regarding Pain Assessment and Management
Participating nurses were generally satisfied with the professional education that they had received regarding PAM, awarding a mean score of 3.2 (SD=1.1), equivalent to 64%, despite almost half (n=79; 46.2%) stating that they had not read any clinical practice recommendations on PAM, while 70 nurses (40.9%) had not read any valid and reliable PAM guidelines and the same percentage had read no guidelines for using analgesia and sedation. Their responses also showed that many nurses had received no education in three other areas: physiological consequences of unrelieved pain (n=85; 49.7%), psychological consequences of unrelieved pain (n=80; 46.8%), and non-pharmacological pain management strategies (n=80; 46.8%). In contrast, the results suggest that nurses were overall well educated regarding pain assessment methods and tools (n=112; 65.5%) and the procedures that induce the most pain (n=109; 63.7%). Table 4 presents details on nurses’ educational needs.
| Question |
Nurses who answered No n(%) |
| Have you read any valid and reliable guidelines for the management of sedation and analgesia? | 70(40.9) |
| Have you read any valid and reliable practice guidelines about the assessment and management of pain? | 70(40.9) |
| Have you read clinical practice recommendations about of pain assessment and management in the non-verbal patient from any of pain management society? | 79(46.2) |
| Have you received education on the following topics during Your professional development? |
|
| Pain physiology mechanisms | 62(36.2) |
| Pain assessment methods and tools in the critically ill patient | 53(34.5) |
| Physiological consequences of unrelieved pain | 85(49.7) |
| Psychological consequences of unrelieved pain | 80(46.8) |
| Painful conditions and procedures | 65(38) |
| Pharmacological pain management principles/strategies | 67(39.2) |
| Non-pharmacological pain management principles/strategies | 80(46.8) |
| Practice recommendations/guidelines | 73(42.7) |
4. DISCUSSION
The aims of this study were to assess ICU nurses’ practices in pain assessment and management, to explore the factors that they perceived as hindering and enabling PAM, and to identify their PAM-related educational needs. Analysis of the data reveals that half of participating nurses wrongly believed that in the case of a patient able to self-report pain, the severity of that pain would be more accurately reported by physicians, nurses and relatives. This unfounded belief contradicts the fact that pain is purely subjective and can most reliably be reported by the patient, as indicated in the definition of McCaffery [23]. Participants in this study were more likely to hold this erroneous view than those in a recent study of Jordanian nurses working in an oncology unit, 74% of whom agreed that the patient would most accurately report pain [24]. Regarding patients unable to report their own pain, the proportion of participants (around three-quarters) who agreed that nurses offer the most accurate assessment was smaller than in two previous studies conducted among Jordanian [5] and Canadian [25] ICU nurses, of whom 84% and 94% respectively reported this belief. The percentage of nurses in the present study stating that they used pain assessment tools for patients able to report pain (60%) was higher than for those unable to report pain (50%), both figures being below the optimal level and much lower than the results of other studies [25-28]. All of these findings indicate the need to encourage nurses to improve their knowledge and skills and to be more expert in pain assessment.
The pain assessment tools most commonly reported as being used in this study were NRS and VAS when patients were able to report pain and CPOT and FLACC when they were unable to do so. These results are similar to those of previous studies [25, 26], indicating that nurses were using valid and reliable tools, so it is recommended that further studies be conducted to ensure their compliance in using these tools appropriately. In addition, it is recommended that these tools be added to nursing assessment charts in ICUs, because nurses in this study identified the absence of a pain tool from nursing charts as one of the most common barriers to assessing pain in ICU patients.
One of the inappropriate practices revealed by this study is the failure to routinely discuss pain scores and pain management plans during medical rounds. As generally understood, pain management is the responsibility of all healthcare professionals, all of whom, including nurses, should therefore be required to assign a higher priority to it; indeed, an earlier study identified the low priority given to pain management as an obstacle to successful pain management in ICUs [10]. It is further recommended that a study be conducted to assess physicians’ PAM practices for ICU patients, especially because such studies are missing from the Jordanian literature [9].
When factors affecting ICU nurses’ practice were assessed by asking them about barriers and enablers to PAM, they identified insufficient time and workload as the most common barrier. A previous qualitative study of the challenges facing ICU nurses in pain assessment identified workload as an organizational barrier and the inappropriate nurse-to-patient ratio was felt to be its main cause [27]. Similarly, the current study found nurse-to-patient ratios to be incompatible with international recommendations that each nurse should have care of no more than two patients [28]. The ratio of 1:>2 in most of the participating hospitals suggests that decision makers in Jordan should highlight this problem to improve the quality of care for ICU patients, as it has been proven that an improved nursing work environment, with reduced workload, impacts positively on the quality of patient care and reduces mortality [17]. As a first step, research is recommended into the impact of nursing workload on patients’ safety and quality of care in a Jordanian context. A final barrier identified by this study is the unavailability of PAM guidelines, which was also reported by Ugandan nurses, about 73% of whom perceived it to be a barrier [10]. Thus, it is important for hospitals to have valid and reliable PAM guidelines and to integrate them with a special practice policy in ICUs as a requirement for obtaining international accreditation.
It has been clearly demonstrated that Jordanian nurses are in need of further education regarding PAM in ICU settings. Results indicate that most participating nurses did not know any PAM guidelines and that they had not read any recommendations in this regard. Furthermore, they were found to need further education regarding the physiological and psychological consequences of untreated pain, a finding consistent with other studies. This could be explained by the failure to include the topic of pain in curricula, as reported by nursing students [27, 29] or by the inadequate attention given by hospitals’ in-service training units to this topic and the consequent insufficient training given to nurses [24]. Therefore, the inclusion of this topic in nursing school curricula and in training for nurses in hospitals is highly recommended.
CONCLUSION
Although participating ICU nurses in Jordan reported that they performed pain assessment for patients in ICU using proper pain assessment tools, their practice was found to be below the optimal level. Further attention is required to training nurses about how and when to assess pain in ICU patients. Priority should also be given to including discussion of PAM during nursing and medical rounds. Finally, healthcare professionals, organizations, schools of nursing, administrators, and policymakers should work together to take serious action to improve nurses’ knowledge and practices in PAM.
STRENGTHS AND LIMITATIONS
The validity and reliability of the tool which nurses were asked to complete, the Survey of Perceived Pain Assessment and Management Practices for Patients Able and Unable to Self-Report Pain, is considered a strength, whereas low sample size is considered a limitation of the study.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was sought first from the Ethical and Scientific Committee at the Faculty of Nursing in the University of Jordan and the Institutional Review Board (IRB) of the chosen settings.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The authors only used the primary data that was collected in order to this research.
FUNDING
This study has been funded by Deanship of Scientific Research in The University of Jordan, no. (2328/2018/19).
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The author expresses his appreciation to all nurses who participated in this study and thanks all of the participating healthcare institutions for their cooperation and contribution. In addition, the authors gratefully acknowledge the contribution of Dr. Muhammad Darawad for his great efforts in revising the manuscript and editing the English language.


