All published articles of this journal are available on ScienceDirect.
A Qualitative Study on Nursing Support for Patients with Hereditary Neuromuscular Disorders and their Families in Japan
Abstract
Background
Patients with hereditary neuromuscular disorders and their family members often experience emotions such as fear and shame toward the hereditary nature of those disorders.
Aim
This study aimed to examine the support provided by public health and visiting nurses to patients undergoing home-based treatment and their family members in Japan, focusing on how their needs were perceived prior to being connected with forms of support.
Methods
The Modified Grounded Theory Approach was employed. Semi-structured interviews were conducted with 10 participants working in nursing-related occupations, all of whom had given consent. The interview contents were included in the form of transcripts, and text excerpts related to support provided for the purpose of continuous home-based treatment were identified. Concepts were generated from these excerpts and organized into categories, which were used to create a diagram illustrating relationships among them.
Results
Support provided by those in nursing-related occupations involved a process using appropriate methods through the flexible adaptation of multiple roles. The central category was “Techniques for Opening Up”; grounded in this, nurses also took on the role of “Supporting Serious Decisions.” Through “Team Play,” nurses strengthened the social support available in regional areas. Nurses further assumed the role of “Advisor for Hereditary Problems” while continuing to engage in “Continueing to Connect across Generations.”
Conclusion
Individuals working in nursing-related occupations in Japan provided support to patients with hereditary neuromuscular disorders and their family members through flexible adaptation of multiple roles. These findings suggest the need for enhanced education and training in genetic nursing, particularly in community-based settings. These findings suggest the need for enhanced education and training in genetic nursing, particularly in community-based settings.
1. INTRODUCTION
Neuromuscular disorders affect the peripheral nervous system and muscles, causing impairments to voluntary movements. In extreme cases, significant impairments to motor function may occur; for example, patients may enter a state approaching total paralysis [1]. The time of onset varies, ranging from the fetal stage to old age. As many of these disorders are hereditary, family members are often pressured to decide whether to undergo presymptomatic testing [2]. Those at high genetic risk may also face pressure when deciding whether to conceive [3]. Hereditary neuromuscular disorders include Huntington’s disease, spinocerebellar ataxia, myotonic dystrophy, Duchenne/Becker muscular dystrophy, and spinal muscular atrophy. Although oligonucleotide therapeutics and gene therapy methods have been developed for some of these disorders [4], no curative treatment is currently available for many other disorders, and treatment is mainly conducted in the form of symptomatic therapy. In addition, most hereditary neuromuscular disorders are progressive, requiring patients to undergo chronic home-based treatment. Nursing care for hereditary neuromuscular disorders can be categorized into physical, psychosocial, spiritual, and social care [5, 6]; there are also reports that such care has been clearly proposed as a form of caregiver support [7]. Many patients with hereditary neuromuscular disorders receive assistance from informal caregivers in their daily lives. Informal caregivers for individuals with spinal muscular atrophy spend an average of 10 hours per day providing care [8]. These disorders evoke various emotions in family members, including fear, shame, and self-blame. In rare cases, informal caregivers may also experience emotional burdens related to carrier status and inherited risks. Furthermore, the support required by caregivers is diverse and includes emotional support as well as support from partners and the broader community [9]. Family members of patients with familial amyloidotic polyneuropathy have experienced “difficulties with coming to terms with the disease” [10]. In Japan, there are strong cultural tendencies to feel shame regarding characteristics that distinguish one from others, in contrast to Western countries. As a result, families may be conservative and secretive about having relatives with hereditary neuromuscular disorders, which can lead to delays in receiving supportive interventions. In families with a history of Huntington’s disease, members may become preoccupied with the hereditary nature of the disease and live in fear of seeing the onset of symptoms in themselves; in some cases, both patients and family members have experienced isolation [11]. Studies focusing on the experiences of spouses showed that spouses experienced distress at the prospect of becoming family members of individuals with hereditary neuromuscular disorders, and spouses attempted to find ways to live as parents of children who may display an onset of symptoms [12]. In recent years, changes in Japan’s healthcare policy have encouraged greater community integration for patients. There is a growing need to acquire new, specialized knowledge and technologies that aid in managing the severe mental and physical challenges faced by patients in regional areas. The role of public health nurses in Japan has been redefined, and programs are being developed to address emerging issues [13]. As a part of this initiative, there is a need to provide psychosocial support to patients with hereditary neuromuscular disorders residing in regional areas. However, it has been reported that public health nurses in Japan find it challenging to identify genetic issues [14]. Hereditary neuromuscular disorders affect patients from infancy to old age and their family members also require psychosocial support. How do nurses approach patients with hereditary neuromuscular disorders and their family members? How do nurses perceive the needs of family members and patients prior to connecting them with support? In light of the new roles expected of public health and visiting nurses in Japan, this study aimed to clarify the types of support provided by nurses to individuals under their care, namely patients with hereditary neuromuscular disorders residing in regional areas and their family members.
2. MATERIALS AND METHODS
2.1. Participants
The study’s participants were individuals working in nursing-related occupations (public health nurses, visiting nurses, nurses) with experience in providing nursing care to patients with hereditary neuromuscular disorders undergoing home-based treatment and their family members in Japan. Participants were recruited through purposeful sampling. Specifically, the snowball sampling method was used: one home-visiting nursing station, three hospitals, and one academic society were selected, through which suitable individuals were recommended to the researchers. A document outlining details of the study was sent to the ten recommended individuals. Those who agreed to participate were asked to respond voluntarily. The researcher provided a verbal explanation of the study’s content to the ten respondents, and written informed participant consent was obtained from all participants.
2.2. Methods of Data Collection
In the present study, interviews were conducted with 10 participants, all of whom were nursing professionals. No participants declined to participate. Semi-structured, one-on-one interviews were conducted once with each participant, following an interview guide.In addition to collecting basic demographic data, semi-structured interview questions included items such as: “What types of genetics-related nursing care have you provided to patients with hereditary neuromuscular disorders and their families living in the community?” and “What types of genetics-related nursing care do you consider necessary for patients with hereditary neuromuscular disorders and their families living in the community?” Each interview lasted 30–60 minutes and was conducted by the same researcher between February 2020 and December 2024. All interviews were conducted by the first author, a female researcher.As a token of appreciation, each participant received a prepaid card worth approximately USD 14. Participants were encouraged to speak freely about these topics. In response to the COVID-19 pandemic, participants were offered the option to attend the interviews face-to-face, online, or via phone. One interview was conducted by telephone and nine were conducted via online platforms. Interviews took place either in the participants’ homes or in a private room at the researcher's workplace. No one else was present during the interviews.Interviews were recorded and transcribed for analysis. Data collection concluded upon reaching theoretical saturation. The interview transcripts were not returned to the participants for checking; however, clarification of interview content was sought as needed during the research process.
2.3. Theories and Methods Used in Analysis
In accordance with COREQ guidelines, a modified grounded theory approach (hereinafter referred to as M-GTA) [15], based on Glaser and Strauss’s grounded theory methodology [16], was employed in this qualitative study. Both methods share fundamental principles: theoretical development based on empirical data, deep interpretation, and validation through application. However, the M-GTA introduces two key distinctions that improve its practical applicability. First, M-GTA emphasizes analytical themes derived from the perspective of “individuals who have been the focus of analysis.” Consequently, the analysis focuses on specific actions, emotions, and influencing factors, making the results applicable to real-world contexts. Second, the M-GTA does not use the rigorous coding method where data are finely fragmented as proposed by Strauss. Instead, a worksheet was utilized during analysis for the direct formation of concepts; therefore, avoiding the loss of context related to the speech and actions of participants. This approach helped preserve the comprehensive meaning of the data, thus granting the method increased practical applicability [15-17]. Therefore, as this study examined and recorded the process behind the experiences of individuals in nursing-related occupations when providing support to patients with hereditary neuromuscular disorders living in regional areas and their family members, the M-GTA was deemed an appropriate method of analysis. The analytical procedure was as follows:
1. Verbatim transcripts were created based on recorded interview data.
2. Text excerpts related to support provided by individuals working in nursing-related occupations in regional areas to patients with hereditary neuromuscular disorders and their family members for the purpose of continuous home-based treatment were identified. These excerpts were interpreted for meaning and identified as concepts, each of which was defined.
3. The interview transcripts were analyzed and compared to identify additional variations, which were used as supplementary data. Conceptually-related data, whether similar or contrasting, were also investigated. Where necessary, amendments were made to concept titles.
4. As analysis progressed, relationships between identified concepts were studied. Categories were derived from related concepts, and data comparison was repeated.
5. Finally, a diagram was created to illustrate the relationships among the derived categories.
This study was supervised by the co-authors, specializing in qualitative research and by individuals with experience in nursing care for patients with hereditary neuromuscular disorders and their family members. The results of the analysis were presented to the participants for feedback and confirmation, ensuring the validity of the findings. The analysis was conducted manually, without the use of analytical software. All data were originally obtained in Japanese and subsequently translated into English.
2.4. Study Period
The present study was conducted between February 2020 and May 2025. Data were collected from February 2020 to December 2024, followed by data analysis and manuscript preparation.
2.5. Ethical Considerations
This study was conducted with the approval of the ethics review committee at Niigata University (approval number: 2020-0257). The study’s objectives and the disclaimer that participation was entirely voluntary were documented in the ethics approval document. Additionally, participants were informed of their right to decline participation at any time and to withdraw from the study without experiencing any negative consequences. Participants were also assured that all data would remain confidential and that their personal information would be protected. The researchers provided a detailed explanation of the data protection measures, including procedures for data destruction following the study's completion, the publication of findings, and the rigorous protocols governing data management.
3. RESULTS
3.1. Participant Characteristics
The demographic information for the 10 participants (all females) is presented in Table 1. Participants’ ages were as follows: 30–39 years (1), 40–49 years (5), 50–59 years (2), and 60–69 years (2). The participant with the least nursing experience had worked for 19 years, while the most experienced participant had worked for 40 years. The average number of nursing experience was 27.5 (±6.7). Participants’ occupations were as follows: public health nurses (3), visiting nurses (pediatric nursing) (3), and nurses (4). The patients under care were diagnosed with conditions such as spinocerebellar ataxia, Duchenne muscular dystrophy, Huntington’s disease, spinal muscular atrophy, and spinal and bulbar muscular atrophy.
| - | Gender | Age Group | Nursing Experience (years) | Years of Working with Intractable Disease Patients |
Occupation |
|---|---|---|---|---|---|
| A | Female | 40s | 21 | 8 | Nurse |
| B | Female | 30s | 19 | 5 | Public health nurse |
| C | Female | 40s | 28 | 10 | Nurse |
| D | Female | 60s | 38 | 19 | Public health nurse |
| E | Female | 50s | 30 | 17 | Visiting nurse (for children) |
| F | Female | 40s | 20 | 3 | Visiting nurse (for children) |
| G | Female | 60s | 40 | 30 | Public health nurse |
| H | Female | 50s | 27 | 21 | Visiting nurse (for children) |
| I | Female | 40s | 26 | 18 | Nurse |
| J | Female | 40s | 26 | 10 | Nurse |
| Average | - | - | 27.5 | 14.1 | - |
| SD | - | - | 6.7 | 7.9 | - |
3.2. Results of Analysis
When providing care to patients with hereditary neuromuscular disorders and their family members living in regional areas with the purpose of continuous home-based treatment, individuals in nursing-related occupations followed a situation-appropriate process. This involved actively eliciting the needs of both patients and family members while demonstrating flexibility in adapting to multiple roles. Participants also employed professional techniques characteristic of genetic nurses. The process that emerged from the flexible adaptation of these multiple nursing roles in supporting patients with hereditary neuromuscular diseases is shown in Fig. (1). The four category titles are enclosed in quotation marks, as there are eight subcategory titles. The narrative description of the process is presented below. The category central to the flexible adaptation of roles by nursing professionals was titled “techniques for opening up.” Participants employed “empathetic techniques” while showing “consideration of sentiments where it is hard to come to terms with the disease.” At times, they assumed the role of “supporting serious decisions,” “listening to patients and family members regarding decisions about future pregnancies and birth,” while also “facing serious issues head on.” Through “team play,” participants strengthened social support systems in regional areas. As depicted in the circular process indicated by the white arrows in Fig. (1), participants assumed the role of “advisor related to genetic challenges” while “continueing to connect across generations,” including paying attention to the onset of symptoms among blood relatives.
3.3. Explanation of four Categories and one Subcategory
3.3.1. Supporting Serious Decisions
This category was constructed from two subcategories: “listened to patients and family members regarding decisions about future pregnancies and birth” and “faced serious issues head on.” This was a category where participants listened to decisions regarding the most delicate issue related to hereditary disorders, namely future pregnancies and births. Participants engaged in serious discussions about who would provide end-of-life care and how such care would be delivered. They also offered psychological support to assist patients and family members in navigating these emotionally difficult decisions.
3.3.2. Techniques for Opening Up
This category was identified as a core category within the process examined in this study. It was constructed from two subcategories: “empathetic techniques” and “consideration of sentiments where it is hard to come to terms with the disease.” A relevant account was provided by Participant I: “Even when they (a patient with Huntington’s disease) flew into a rage, I still visited them (to check up on them). They (the patient) would say things like, what are you here for, but when they saw (my face), I felt as if they remembered me.”
A cultural characteristic in Japan is that silence is often the norm; hereditary disorders are typically kept secret, making it difficult even for medical professionals to elicit the true wishes and thoughts of patients and their families. To exacerbate the matter, feelings of distrust may cause patients and family members to refuse to open up to medical professionals any further. Since care was provided not in hospitals but within the familial setting of patients' homes, it was necessary to employ “empathetic techniques” while showing “consideration for the emotional difficulty of accepting the disease.” This category was constructed from these two advanced techniques.
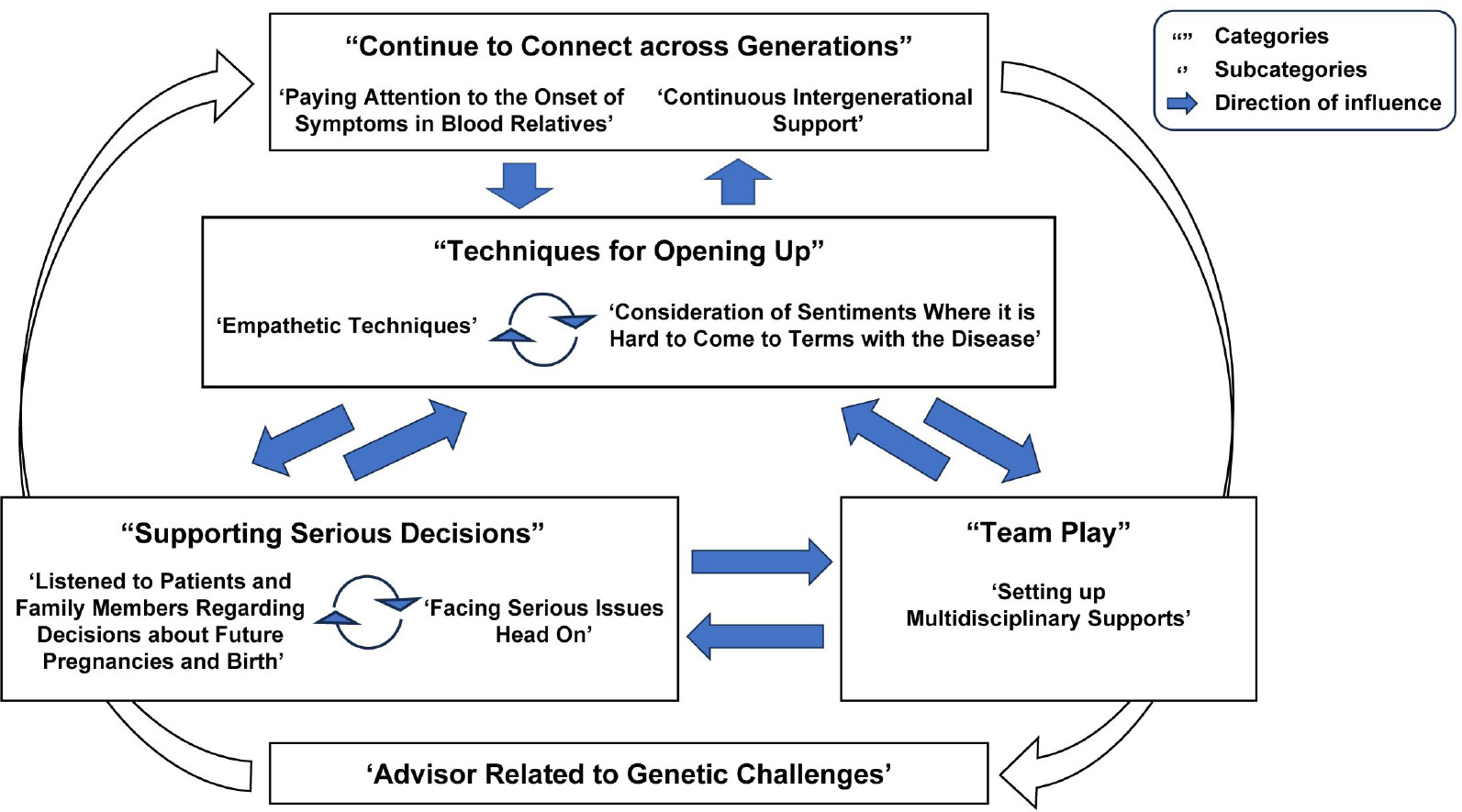
Processes undertaken by individuals in nursing-related occupations in providing support to family members of, and patients with hereditary neuromuscular disorders with the purpose of continuous home-based treatment.
3.3.3. Continue to Connect across Generations
This category was constructed from two subcategories: “paying attention to the onset of symptoms in blood relatives” and “continuous intergenerational support.” After the death of patients with hereditary neuromuscular diseases, symptoms may appear in their siblings or children. This category highlights how nurses not only cared for patients but also monitored the health of their blood relatives-in other words, the next generation. One account illustrates this: “When I was in charge of a patient with Machado-Joseph disease, their younger brother started displaying symptoms, but the symptoms were still mild. The older sister had passed away as her symptoms were severe, but when we implemented a regional support system for her, we quietly kept track of the younger brother’s condition. As his symptoms worsened, the individuals who had supported the older sister were able to intervene before the situation became unmanageable” (Participant A).
3.4. Team Play
This category, consisting of a single subcategory-“setting up multidisciplinary support”-describes how social support structures were reinforced. It focuses on the collaborative roles undertaken by participants, who worked together with professionals from various disciplines to address emerging challenges through coordinated teamwork.
3.5. Advisor related to Genetic Challenges
This category was generated as a subcategory but has a bearing that is equivalent to that of a main category. It encompasses support provided in response to genetic concerns raised by family members, as well as advice on how to communicate genetic risk information to family members. One specific account follows: “When individuals have a parent with a hereditary disorder, they worry about whether they have inherited it. When these individuals get married, many of them request presymptomatic testing. I often receive questions about how to undergo such testing” (Participant J).
4. DISCUSSION
4.1. The Unique Support provided by Genetic Nurses in Japan
This study was the first to shed light on the content of support provided by nurses in Japan to patients with hereditary neuromuscular disorders and their family members undergoing at-home treatment. The findings revealed that nurses in Japan flexibly adapted to multiple roles in delivering support. Nurses were found to play a role in connecting professionals from various occupations specializing in genetics, while also taking on the role of advisor related to genetic challenges. Furthermore, their support often extended across generations–for instance, by identifying early symptoms in family members and facilitating access to care–reflecting a role uniquely held by individuals in nursing-related occupations. Given that many individuals in Japan tend to be secretive regarding genetics, it was noteworthy how nurses would employ techniques to build trust, enabling family members and patients to open up and express their true wishes and thoughts. These insights were extracted through the use of qualitative methods-specifically, an inductive and exploratory approach. Participants in this study held diverse roles: they were public health nurses, visiting nurses, or hospital-based nurses. Some provided care to adults, while others specialized in pediatric care. However, participants employed techniques that allowed patients and family members to open up while taking on the role of advisor regarding genetic challenges; participants also continued to connect across generations. It was possible to identify this common process using the modified grounded theory approach (M-GTA) in interpreting the obtained interview data, as well as continuous analysis. This analytical process confirmed the appropriateness and reliability of the chosen methodology. Prior studies have not gone further than listing the roles played by nurses [18]; nevertheless, it was possible to derive a conceptual model of the active support process conducted by nurses through the adaptation of multiple roles.
4.2. The Uniqueness of Nursing in relation to Hereditary Disorders
This study demonstrated that nurses played the role of advisors in relation to genetic challenges. In particular, many patients with children expressed concern that their illness might be inherited by the next generation [19]. Additionally, patients also voiced apprehension about the appropriate timing for informing their children of hereditary risks; family members who are carriers of a recessive genetic disorder may also experience self-blame [20]. Genetic counselling is recommended in the face of such genetic challenges. However, the number of genetic counsellors in Japan is approximately 400 [21], which is approximately 10% of the number of professionals in the same field in the United States. Moreover, genetic counsellors tend to be concentrated in urban areas, making them less accessible to those living in rural regions. In particular, in cases involving hereditary neuromuscular disorders that affect cognitive and motor abilities, patients often experience associated social impairments, such as social withdrawal [22]. Furthermore, family members of such patients may avoid discussing the disorder within the family [23]. As a result, accessing genetic counselling becomes more difficult, as individuals must voluntarily make appointments and leave their homes to receive these services. Given this background, individuals working in nursing-related occupations, who maintain regular contact with patients, naturally assume the role of advisors regarding genetic challenges while addressing the needs of patients and family members. Nurses also clearly engage in “team play” by facilitating coordination with relevant departments when more specialized genetic consultations are required.
In addition, nurses provided a unique form of support by “paying attention to the onset of symptoms in blood relatives.” They did not conduct genetic consultations purely in verbal form, but also conducted physical assessments through visual inspection. Nurses were able to detect early symptoms in at-risk individuals based on information shared by family members, while also guiding them toward appropriate treatment options. A prior study that identified the practical capabilities of genetic nurses in Japan suggested that nurses “made adjustments so that patients and family members were able to receive genetic counselling” (reiteration: 18). This study is the first to demonstrate support in which nurses proactively identified early symptom onset in at-risk individuals. Through early medical interventions for those showing initial symptoms, it becomes possible to begin the process of appropriate treatment methods and rehabilitation, which also contributes to the maintenance of QOL over a long period. In this study, individuals working in nursing-related professions paid attention to patients and blood relatives of patients; they exchanged information about blood relatives with professionals from other occupations even after patient death and provided support that “continue[d] to connect across generations.”
4.3. Clinical Applications
The results of this study should be applied to training programs provided for individuals working in nursing-related occupations in regional areas. Genetic nursing has been included in nursing fundamentals taught at the university level since 2025 [24]; however, most nurses who are currently practicing have not received education regarding genetic nursing. Thus, it is known that public health nurses in Japan find it difficult to identify genetic issues (reiteration: 12). Education related to techniques for opening up, supporting serious decisions, and becoming an advisor for hereditary problems is necessary for the identification of genetic issues. In Japan, more opportunities have arisen for genetic screening to be conducted under insurance coverage [25]. As gene therapies have also begun to be conducted [26], it is becoming increasingly important that nursing professionals receive education on genetic nursing. By incorporating the above into educational processes, it becomes possible to contribute to improved capabilities in nurses as well as provide increasingly appropriate support to patients with hereditary neuromuscular disorders and their family members.
4.4. Limitations of this Study
It should be noted that this study has several limitations. First, participants in this study were limited to individuals working in nursing-related occupations. The degree of satisfaction felt by patients and family members toward the support provided, as well as how the support provided was perceived, was not explored in this study. Second, as the participants targeted in this study provided care to patients undergoing treatment at home, care should be taken when applying this conceptual model to nursing care provided to individuals admitted to facilities or hospitals. Finally, the degree of severity of hereditary neuromuscular disorders was not taken into account. Moving forward, research targeting patients and family members should be conducted to assess the effectiveness of the support process demonstrated in this study.
CONCLUSION
The support process undertaken by nurses providing care to patients with hereditary neuromuscular disorders and their families in home care settings in Japan involved the flexible assumption of multiple roles and the application of context-specific approaches. Central to this process was the use of “Techniques for Opening Up,” through which nurses established rapport with patients and their families while simultaneously fulfilling diverse support functions. Individuals with hereditary neuromuscular disorders and their families often conceal their genetic condition, thereby increasing the risk of exclusion from social support systems. Nurses who maintained regular contact with these families were well-positioned to deliver effective, empathetic genetic counseling, facilitate complex decision-making processes, promote early identification of disease onset in at-risk individuals, and support the intergenerational continuity of care. The findings of this study underscore the pressing need for enhanced genetic nursing education and specialized training for community-based nursing professionals, alongside the refinement of counseling techniques.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: H.S.: Conceptualization, formal analysis, funding acquisition, project administration, resources, writing-review & editing; T.S.: Formal analysis, writing-review & editing; J.S. and M.I.: Formal analysis, methodology, writing-review & editing. All authors have read and agreed to the published version of the manuscript.
ABBREVIATION
| MGTA | = Modified Grounded Theory Approach |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Review Committee of Niigata University, Japan (approval number: 2020-0257).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants gave their informed consent for publication, with all personal details anonymized to protect privacy.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [H.S] upon reasonable request.
FUNDING
This study was conducted with funding provided by the Japan Society for the Promotion of Science in the form of the Grant-in-Aid for Scientific Research (23K10271).
ACKNOWLEDGEMENTS
The authors would like to express their heartfelt gratitude to Professor Naoko Arimori from the Graduate School of Health Sciences at Niigata University for providing valuable guidance and advice at the time this study was conducted.


