All published articles of this journal are available on ScienceDirect.
The Impact of Enhanced Recovery After Surgery (ERAS)-Based Islamic Perioperative Nursing Education Program on Nurses’ Competence
Abstract
Introduction
Nurses, as integral members of the healthcare team in enhanced recovery after surgery (ERAS) pathways, must be empowered with consistent education to provide evidence-based and culturally competent care. This study aimed to evaluate the impact of an ERAS-based Islamic perioperative nursing (ERAS-BIPN) education program on nurses’ competence, including knowledge, attitudes, and skills.
Methods
A quasi-experimental pre-post test design with a control group was implemented, involving 84 perioperative nurses in Aceh Province, Indonesia. Nurses’ competence was evaluated at baseline, immediately after the intervention, and three months after. Data were analyzed using descriptive statistics (mean and standard deviation) and inferential statistics (chi-square test, independent t-test, and repeated measures ANOVA).
Results
Findings indicated that nurses in the intervention group had significantly higher competence scores at all three measurement points (p-value <0.001) than those in the control group (p-value=0.80). A significant difference in nurses’ competence was observed over time within the intervention and control groups (F=149.654, p-value <0.001), between the two groups (F=9.139, p-value=0.003), and in the interaction between time and group (F=105.701, p-value <0.001).
Discussion
The intervention program significantly improved nurses’ competence, with effects sustained up to three months. Integrating this competence into patient care ultimately leads to better outcomes and increased satisfaction. However, further research is needed to examine the long-term sustainability of nurse competency and its impact on enhancing surgical patient care.
Conclusion
The ERAS-BIPN education program had a beneficial effect on nurses’ competence. The findings can guide the development of ongoing education programs to ensure nurses are adequately trained for effective ERAS implementation.
1. INTRODUCTION
Traditional perioperative care often relies on outdated practices that lack support from the latest evidence, resulting in detrimental effects [1, 2]. The outdated practices, such as prolonged fasting and mechanical bowel preparation before surgery, can lead to insulin resistance, decreased bowel function, and fluid and electrolyte imbalances. Intraoperative hypervolemia, excessive opioid administration, the use of drainage tubes and catheters, and delayed postoperative immobilization can prolong recovery time and increase postoperative complications, thereby delaying hospital discharge [3].
Patient-centered and evidence-based perioperative nursing care is essential as a standard protocol to accelerate the recovery process. Enhanced recovery after surgery (ERAS), pioneered by Henrik Kehlet in the mid-1990s, challenged traditional perioperative care and initiated a paradigm shift toward modern, evidence-based surgical care [2, 3]. ERAS is a multimodal perioperative management care designed to enhance patient recovery after surgery by preserving physiological function and minimizing the surgical stress response [3]. Strategies, such as preoperative carbohydrate loading and shorter fasting duration, are used to stabilize blood glucose, reduce insulin resistance, and mitigate the surgical stress response [3]. Encouraging patients to start moving and participating in physical activity shortly after surgery aims to improve bowel motility, improve circulation, prevent lung infections, and accelerate the overall recovery process [3].
Despite the numerous benefits that ERAS elements offer in promoting patient recovery, adoption in Indonesia has been slow. Not all hospitals have fully adopted the ERAS protocol as the standard for perioperative care [4]. A study conducted in an Indonesian tertiary hospital reported compliance rates of 67% with ERAS protocol components [5]. Another study indicated that no patient was proficient in fulfilling all components of the ERAS protocol, with only six respondents successfully adhering to ten or more components [6]. Three main barriers were patient-related (characteristics and compliance), physician-related (silo mentality and resistance to change), and hospital-related (long waiting lists and inability to provide required facilities) [5, 6].
Successful ERAS implementation requires a multidisciplinary team approach and a willingness to adapt to evolving medical knowledge [7]. As essential team members, nurses play a pivotal role in providing continuous patient care, and adherence to ERAS pathways relies heavily on nurses' daily patient care throughout the perioperative process [8-10]. Nurses are the professionals who spend the most time with patients throughout the perioperative pathway and frequently lead and coordinate care across disciplines, ensuring compliance with ERAS elements [10, 11]. However, while nurses are vital, most studies on ERAS implementation primarily focus on the roles and responsibilities of surgeons [11]. Currently, perioperative nursing care has yet to be fully optimized, making it crucial to strengthen the role of nursing in implementing ERAS pathways [11, 12].
Although perioperative care appears to be a multidisciplinary approach, nurses often find themselves merely executing physician-prescribed care plans, which may lead to overlooking their unique contributions. This practice undermines the critical role of nursing care in achieving optimal patient outcomes and accelerated recovery, particularly following surgical procedures [13]. Patient care cannot continue to be driven solely by tradition or the preferences of healthcare providers. Therefore, this study highlights the importance of developing nurse competencies regarding evidence-based practice in surgical patient care.
To enhance the effectiveness of healthcare services, it is essential to integrate patients' beliefs and spiritual needs [14, 15]. This principle is particularly relevant in Indonesia, which has the world's largest Muslim population, totaling 243 million individuals, or 88.25% of the Indonesian population and nearly 13% of the global Muslim community [16]. Furthermore, Aceh stands out as the province with the highest concentration of Muslim residents, totaling 5.44 million people, or 98.61% of the total population [17]. Given this demographic reality, Islamic healthcare services are essential for providing culturally relevant care.
Religious beliefs serve as a resource to mitigate anxiety and fear associated with surgery, positively influencing the recovery process [18-20]. This aligns with the International Council of Nurses (ICN) code of ethics [21], which mandates that nurses foster “an environment in which the human rights, values, customs, and spiritual beliefs of the individual, family, and community are respected.” Currently, there is a growing recognition of the importance of Islamic healthcare services, particularly for Muslim-majority countries and beyond. To promote evidence-based practices that integrate the local values of Muslim patients in perioperative nursing, nurses need to undergo a comprehensive learning process. Therefore, this study aimed to assess the effectiveness of an ERAS-based Islamic perioperative nursing education program for nurses' competence.
2. MATERIALS AND METHODS
2.1. Study Design
A quasi-experimental design, a time-series with a control group, was used to assess the impact of an enhanced recovery after surgery (ERAS)-based Islamic perioperative nursing education program on nurses' competence. The quasi-experimental design maintains both realism and feasibility, enabling causal inference through repeated measurements over time. By having a control group, researchers can effectively isolate the effects of an ERAS-BIPN educational program by comparing it to a similar group that did not receive the intervention.
2.2. Study Participants
The study participants were perioperative nurses in Aceh Province, Indonesia. The sample size was determined using G*Power 3.1.9.7 based on a reported effect size of 0.64 from previous studies [22], with a significance level of 0.05 and a power of 80%. This calculation indicated a required sample size of 40 participants per group [23]. To account for potential attrition, a total of 84 perioperative nurses were recruited.
Participants were selected through purposive sampling based on the following inclusion criteria: a minimum educational level of Diploma-III in nursing, registered nurse, at least one year of experience in perioperative nursing, effective communication skills, and voluntary consent to participate in the study. Exclusion criteria involved the inability to attend the educational program due to annual leave, maternity leave, or other essential reasons. No participants were excluded from the study.
2.3. Measurement
The measurement tools consisted of two parts. The first part collected demographic information, including age, gender, marital status, education level, work experience, and previous experience attending ERAS and Islamic healthcare seminars. The second part involved the ERAS-based Islamic perioperative nursing questionnaire (ERAS-BIPNQ). The questionnaire aims to evaluate nurses’ competence in perioperative nursing practices aligned with ERAS protocols and Islamic spiritual principles.
The ERAS-BIPNQ includes 45 questions across three domains: knowledge, attitudes, and skills. The knowledge domain comprises items that assess nurses’ understanding of ERAS protocols and Islamic perioperative nursing care, covering topics, like general principles of ERAS, preoperative education, prehabilitation, nutritional optimization, early mobilization, multimodal pain management, prevention of nausea and vomiting, minimally invasive surgery, halal dietary and medication guidelines, gender-concordant care, and spiritual support, using multiple-choice questions where correct answers are scored as 1 and incorrect as 0. The attitudes domain features statements that explore nurses’ beliefs, values, and emotional dispositions regarding the integration of ERAS-based Islamic perioperative nursing care. Content areas include the perceived importance of religious accommodations, confidence in adapting ERAS to Islamic contexts, and willingness to engage in evidence-based and spiritually sensitive care. Responses were measured using a Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The skills domain highlights self-reported practical skills in applying ERAS-based Islamic perioperative nursing care, including facilitating worship activities for surgical patients, maintaining modesty and privacy during surgery, ensuring gender-concordant care, and implementing ERAS interventions. The scores from all three domains were combined to determine overall nurses’ competence in ERAS-based Islamic perioperative nursing care, with higher scores indicating greater competency.
The researchers developed the questionnaire and intervention program module based on a literature review of ERAS protocols and Islamic perioperative nursing. Three experts in medical-surgical nursing and Islamic healthcare services assessed the questionnaire for content validity, language appropriateness, and criteria, resulting in a scale-content validity index (S-CVI) of 0.96. Its reliability was confirmed through internal consistency testing, yielding a Cronbach's alpha of 0.83. A Cronbach's alpha value above 0.70 or higher is considered an acceptable level of internal consistency for a scale or test [23].
2.4. Program Development
Program development began with a focus group discussion (FGD) involving ten perioperative nurses, followed by in-depth, face-to-face interviews with seven nurse managers, surgeons, and anesthesiologists, two Islamic religious counselors working in the hospital, and six Muslim scholars from the Ulama Consultative Council. Both FGD and interviews aimed to identify and explore the competency needs of perioperative nurses in providing evidence-based and culturally sensitive care to Muslim patients undergoing surgery. The findings have offered a better understanding of developing learning strategies and designing educational content that aligns with the local context.
2.5. Description of the Education Program
The educational content was designed and developed based on literature related to the ERAS protocols and Islamic perioperative nursing care [3, 24], as well as recommendations from nurses, surgeons, anesthesiologists, religious counselors, and Muslim scholars. The intervention aimed to enhance nurses' competence in integrating Muslim patients' spiritual values into evidence-based perioperative nursing care.
A team of program providers was formed to support the educational program based on their respective competencies and expertise, led by the research team. Four experts were selected, including a surgical nurse manager, a perioperative nurse experienced in ERAS teams, a digestive surgery specialist, and an Islamic religious counselor. All experts and researchers reached a mutual understanding of the educational program through intensive literature reviews and discussions to develop educational resources.
The enhanced recovery after surgery-based Islamic perioperative nursing (ERAS-BIPN) education program was conducted for three days, with eight hours of training per day (four sessions of two hours each). The program comprehensively covered fundamental competency content. Each session focused on a specific topic.
On the first day, the theme “Islamic Spiritual Care in Sharia Hospitals and its Implementation in Surgical Patients” was addressed through four sessions, which included the following topics: (1) the concept of Islamic spiritual care, along with the objectives and legal foundation of Islamic spiritual care in Sharia hospitals; (2) various aspects of Islamic spiritual care, including management and healthcare services; (3) minimum service standards for Sharia hospitals and mandatory quality indicators; and (4) Islamic-compliant care in surgical patients.
On the second day, the theme “Enhanced Recovery After Surgery (ERAS) Protocols” was discussed, with topics including (1) the surgical stress responses; (2) the history and concept of ERAS protocols; (3) the benefits of ERAS and its multidisciplinary team; (4) the components of ERAS and its implementation; and (5) facilitating and inhibiting factors of ERAS implementation.
The third day focused on “Optimizing Nurses’ Role in ERAS Implementation: A Case Study of ERAS Protocol Implementation in Perioperative Nursing at Dr. Cipto Mangunkusumo General Hospital (a national tertiary-level hospital)”, covering topics, such as (1) factors affecting surgical patient recovery; (2) the perioperative nursing care; (3) the role of nurses in ERAS; and (4) perioperative nursing management in ERAS. This was followed by material on “The ERAS-based Islamic Perioperative Nursing Care (ERAS-BIPN)”, covering the entire surgical pathway, with topics including (1) ERAS-BIPN in the pre-admission phase; (2) ERAS-BIPN in the preoperative phase; (3) ERAS-BIPN in the intraoperative phase; and (4) ERAS-BIPN in the postoperative phase.
The educational program was primarily delivered through face-to-face sessions to enhance nurses' participation, focus, and engagement. However, to improve accessibility, a subject matter expert from a distant tertiary hospital (2,324.5 km away) conducted learning sessions via video conference. The program utilized various teaching strategies, including didactic presentations with educational materials and case-based discussions. Additionally, supplementary teaching media consisting of modules, assessment and implementation forms, and educational leaflets were provided.
The control group only participated in a one-time mandatory Shariah service training delivered by a religious counselor at the hospital. This training focused on the standards of Shariah-based healthcare services for all nurses working in Islamic hospitals. To ensure equal treatment and address ethical concerns, if the effectiveness of the ERAS-BIPN educational program is confirmed, the intervention would be extended to provide the same educational materials to the participants in the control group.
2.6. Data Collection
After obtaining ethical approval and the necessary permissions, participants were identified and selected based on inclusion criteria. The researchers created a WhatsApp group and provided detailed information about the educational program. Nurses enrolled in the study were required to sign a consent form two weeks before the educational program commenced. Participants were randomly assigned to either the intervention or control group using a code number printed on the questionnaire; participants with even numbers were placed in the intervention group, while those with odd numbers were assigned to the control group. The equivalence between both groups was assessed.
The first author scheduled the educational sessions for participants in the intervention group and sent reminders via WhatsApp group to ensure participation at the designated times. To achieve the highest response rate, an appropriate time was allocated for data collection, and a deadline was set for submitting completed questionnaires. Additionally, participants were informed about the study’s objectives, contents, methods, and expected learning outcomes for each educational session, and were assured that they would receive a certificate upon completing the series of educational programs.
Data were collected using anonymous, self-reported electronic questionnaires from September to December 2024. Baseline data were gathered from both the control and intervention groups to assess nurses' competence regarding ERAS-based Islamic perioperative nursing care before the intervention. Post-intervention follow-up assessments were conducted twice: immediately after completing the educational program and three months later. Participants completed a Google Form questionnaire for data collection, accessed through a link shared in the WhatsApp group, with assistance provided by two research assistants.
2.7. Data Analysis
Data were analyzed using IBM SPSS version 30.0. Descriptive statistics were used to describe the participants' characteristics. Chi-square and Levene's tests were used to identify homogeneity between the control and intervention groups. Subsequently, the normality of continuous variables was examined using the Kolmogorov-Smirnov test to confirm the choice of analysis. Independent t-tests were then conducted to compare the mean competency scores of nurses between the two groups at three measurement points. To evaluate the effect of the ERAS-BIPN education program and changes in nurse competence over time, repeated measures ANOVA was utilized with a significance level set at a p-value < 0.05.
2.8. Ethical Consideration
This study was approved by the health research ethics committee of Dr. Zainoel Abidin General Hospital with number 115/ETK-RSUDZA/2023. The researchers provided detailed information about the study, and written consent was obtained from each participant. Participation was entirely voluntary, and the participants could withdraw at any time. The researchers kept all data confidential, and electronic files were stored on a password-protected computer. Identification codes replaced individual names on all documents, ensuring participant privacy throughout the study and publication of results.
| Variables | Int. (n=42) | Cont. (n=42) | x2/ t | p-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age (years) | - | - | - | - | - | - |
| < 30 | 31 | 73.8 | 30 | 71.4 | 0.167a | 0.684 |
| 30-40 | 4 | 9.5 | 4 | 9.5 | ||
| >40 | 7 | 16.7 | 8 | 19.1 | ||
| Median (IQR) = 25,00 (12) | - | - | - | - | - | - |
| Gender | - | - | - | - | - | - |
| Male | 6 | 14.3 | 7 | 16.7 | 0.091b | 0.763 |
| Female | 36 | 85.7 | 35 | 83.3 | ||
| Marital status | - | - | - | - | - | - |
| Married | 18 | 42.9 | 14 | 33.3 | 0.808b | 0.369 |
| Single | 24 | 57.1 | 28 | 66.7 | ||
| Education level | - | - | - | - | - | - |
| Diploma | 4 | 9.5 | 8 | 19.1 | 2.933b | 0.231 |
| Bachelor’s | 31 | 73.8 | 31 | 73.8 | ||
| Master’s | 7 | 16.7 | 3 | 7.1 | ||
| Work experience (years) | - | - | - | - | - | - |
| <5 | 31 | 73.8 | 31 | 73.8 | 0.400a | 0.523 |
| >5 | 11 | 26.2 | 11 | 26.2 | ||
| Median (IQR) = 1,00 (7) | - | - | - | - | - | - |
| Attendance prior to training on ERAS | - | - | - | - | - | - |
| Yes | 17 | 40.5 | 17 | 40.5 | 0.000b | 1.00 |
| No | 25 | 59.5 | 25 | 59.5 | ||
| Attendance prior to training on Islamic care | - | - | - | - | - | - |
| Yes | 27 | 64.3 | 29 | 69.0 | 0.214b | 0.643 |
| No | 15 | 35.7 | 13 | 31.0 | ||
3. RESULTS
3.1. Characteristics of Participants
All eighty-four participants completed the questionnaires at the three required measurement points, with no withdrawals during the study (response rate = 100%). The majority of both groups were female and predominantly under 30 years of age (72.6%) with <5 years of working experience (73.8%). New nurses were more adaptable to the program and tended to adapt more quickly than nurses who had worked in a certain way for years and had difficulty accepting change [25]. A comparative analysis of all participants' characteristic variables revealed p-value >0.05, indicating equivalence between the control and intervention groups. A general overview of participant characteristics is presented in Table 1.
3.2. Nurses’ Competence in ERAS-based Islamic Perioperative Nursing Care
Before the intervention, the baseline scores for all study participants ranged from 47 to 73, with a mean of 57.85 (SD = 5.734). The control group exhibited a slightly higher pre-test mean score (58.19, SD = 5.697) compared to the intervention group (57.50, SD = 5.819). However, no statistically significant difference was observed between the intervention and control groups in pre-intervention test scores (t = 0.549, p-value = 0.584), indicating baseline homogeneity between the two groups (Table 2).
Following the intervention, the intervention group demonstrated a significant increase in mean competence scores at both post-test measurement points compared to the control group (post-intervention: t = -3.840, three months post-intervention: t = -5.437, p-value < 0.001). Furthermore, the intervention group showed a significant difference in mean scores across the three measurement points (baseline, immediately post-intervention, and three months post-intervention) (F = 488.404, p-value < 0.001). Conversely, the control group did not exhibit significant differences in mean competence scores across the three measurement points (F = 2.699, p-value > 0.080). Nurse competence scores are detailed in Table 2.
The time impact analysis of the ERAS-BIPN education program revealed a significant difference in mean nurse competence scores within groups at baseline, immediately post-intervention, and three months post-intervention (F = 149.654, p-value < 0.001, η2 = 0.646). The interaction effect between time and group demonstrated a significant difference in the post-test nurse competence score of the intervention group (F = 105.701, p-value < 0.001, η2 = 0.563).
| - | n |
Cont. Mean (SD) |
n |
Int. Mean (SD) |
t | p-value |
|---|---|---|---|---|---|---|
| Baseline | 42 | 58.19 (5.697) | 42 | 57.50 (5.819) | 0.549 | 0.584 |
| Directly after the intervention | 42 | 58.64 (6.332)a | 42 | 64.50 (7.591)b | -3.840 | <0.001 |
| Three months after the intervention | 42 | 59.02 (6.384)a | 42 | 66.19 (5.675)b | -5.437 | <0.001 |
| Variable | SS | df | MS | F | p-value | η2 |
|---|---|---|---|---|---|---|
| Between subjects | ||||||
| Within group (error) | 9139.206 | 82 | 111.454 | - | - | - |
| Group | 1064.778 | 1 | 1064.778 | 9.554 | 0.003 | 0.104 |
| Within subjects | ||||||
| Time within group (error) | 577.365 | 146.460 | 3.942 | - | - | - |
| Time | 1053.722 | 1.786 | 589.957 | 149.654 | <0.001 | 0.646 |
| Time*group | 744.246 | 1.786 | 416.688 | 105.701 | <0.001 | 0.563 |
The analysis of between-group effects indicated a significant difference in nurse competence scores between the control and intervention groups across all measurement periods, with F (1, 82) = 9.554, p-value = 0.003, η2 = 0.104. It means that the ERAS-BIPN education program significantly improved nurses’ competence in the intervention group compared to the control group. The improvement was evident both immediately following the intervention and three months later, in contrast to the pre-intervention phase (Table 3).
Fig. (1) presents the profile plot of the adjusted mean (estimated marginal mean) of nurses’ competence scores at three measurement points. In the pre-test, the scores were slightly lower in the intervention group compared to the control group. However, following the intervention and three months post-intervention, the competency scores of nurses in the intervention group increased by 5.86 and 7.17 points, respectively, compared to the control group. It illustrates a significant interaction effect between the group and time variables.
4. DISCUSSION
The main factor in successfully implementing ERAS guidelines is multidisciplinary team collaboration across all aspects of patient care, from preoperative to postoperative stages [25, 26]. Nurses, often serving as ERAS managers in perioperative care, play a crucial role in ensuring adherence to the ERAS pathway [8-10]. They are the driving force behind the success of ERAS programs, making it essential to equip them with evidence-based care practices and effective communication to support patient care [8]. Educational sessions that present evidence on successful implementation, outcomes, and roles of multidisciplinary team members are vital for implementing ERAS protocols [27], as they can enhance nurse compliance [11].
This study has highlighted Muslim patients' spiritual needs, promoting the integration of Islamic values into ERAS protocols. Islamic perioperative care underscores the importance of nurses supporting patients' religious activities and providing support to both patients and their families. Guiding patients to pray before surgery is a form of Islamic nursing intervention. Allocating time for prayer and accompanying the patients during time-out procedures improve comfort levels. Preserving the privacy of surgical patients is a crucial aspect of Islamic perioperative nursing. Nurses need to provide hijabs and sterile attire to minimize unnecessary exposure during the surgical procedure [24]. Gender-concordant care and scheduling elective surgeries to avoid conflicts with prayer times are important, except in emergencies. Islamic perioperative care also emphasizes the significance of providing spiritual motivation, collaborating with an Islamic counselor when necessary, communicating gently using religious phrases, and administering halal products (medications, surgical sutures, and anesthesia) during surgery [28].
At the beginning of the study, the results indicated that nurses' competence in ERAS-based Islamic perioperative nursing care was still far from optimal (mean = 57.85; SD = 5.734). The competency scores were slightly lower in the intervention group compared to the control group (mean = 57.50; SD = 5.819 vs. mean = 58.19; SD = 5.697).
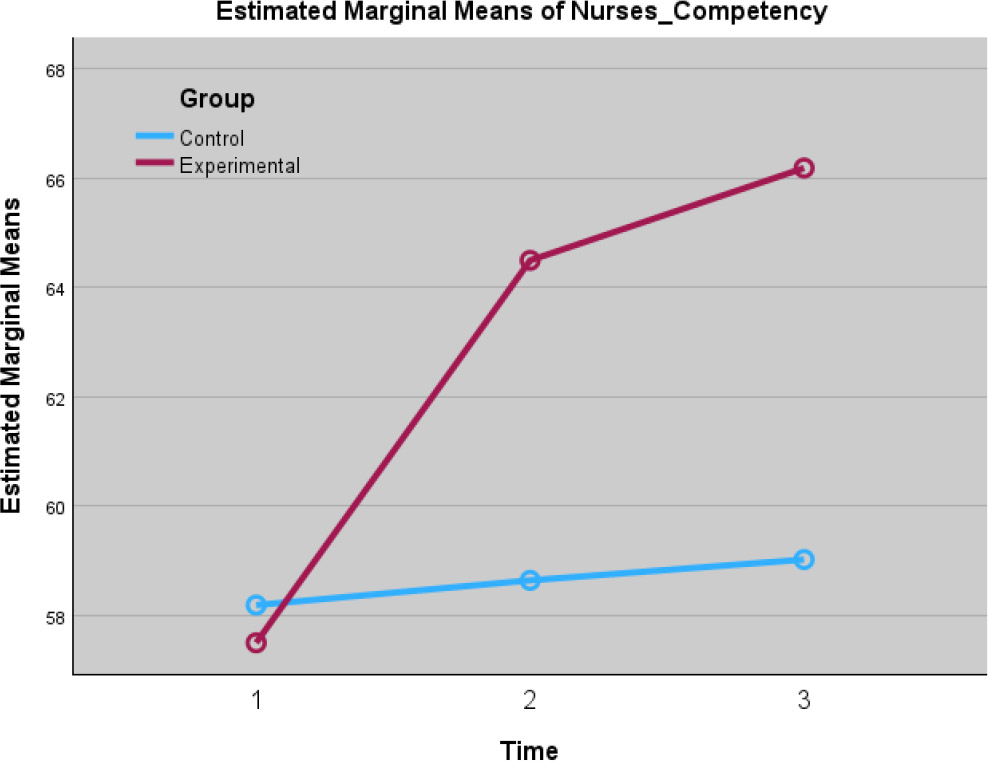
The estimated marginal means of nurses’ competence scores at three measurement points.
Similar findings have been reported by other researchers, who have observed nurses' knowledge of ERAS protocols to remain insufficient, with some exhibiting negative attitudes toward their implementation [29, 30]. Additionally, spiritual care is often overlooked because nurses feel uncertain about how to integrate these protocols into clinical practice [31, 32]. Most nurses in Muslim healthcare settings perceive spiritual care as equivalent to obligatory religious activities in Islam and report a lack of adequate skills or formal training in delivering spiritual care [33]. The baseline data have indicated that nurses’ competence requires further enhancement.
The impact of the ERAS-BIPN educational program on each group was assessed by measuring changes in nurse competence from baseline to immediate post-intervention and three months post-intervention. Nurse competence scores in the intervention group increased from 57.50 to 64.50 (T2) and 66.19 (T3), while the control group showed no significant change from the pre-test [58.19 to 58.64 (T2) and 59.02 (T3), p-value >0.05]. The steady increase in scores within the intervention group indicated the positive impact of the ERAS-BIPN educational program on participants. The findings have supported previous studies recommending that surgical nurses receive training on the evidence-based ERAS guidelines [30].
Providing comprehensive, coherent, and locally relevant information to healthcare professionals significantly enhances the implementation and delivery of ERAS pathways [25]. For Muslims, culture and faith are deeply interconnected and inseparable, as Islam influences every aspect of life, including health-related matters [34]. Islamic values strongly influence nurses' attitudes in the workplace, which can impact their commitment to the organization [35]. Undeniably, nursing care should inherently incorporate spiritual aspects [21].
The effectiveness of the ERAS-BIPN educational program was evaluated by comparing the intervention and control groups based on its impact over time, time and group interaction, and between-group differences. The findings immediately after intervention demonstrated a significant improvement in nurses’ competence, which was sustained for up to three months. The findings confirmed the ERAS-BIPN educational program to have a long-term effect on maintaining the positive impact of nurse competence in this area. Integrating these competencies into patient care has consistently been associated with improved quality of care, patient safety, and many positive clinical outcomes for surgical patients. ERAS protocols ensure that care is based on the best available research, leading to more effective and safer perioperative interventions [3, 4, 13], while spirituality-sensitive care acknowledges patients' spiritual needs, which can positively impact their overall well-being and recovery after surgery [18-20].
Nurses are expected to be sensitive and respectful of patients' spiritual beliefs and practices to meet their spiritual needs, as an essential component of holistic nursing [21]. Indeed, religiosity plays a role in shaping consumption needs in Muslim-majority countries, including preferences for healthcare services [36]. Patient demands and preferences are key reasons why implementing Islamic nursing care is essential [28], potentially increasing patient satisfaction [37]. Therefore, the researchers emphasize the importance of ERAS-based Islamic perioperative nursing education programs, particularly amid the growing demand for spiritually sensitive healthcare services.
The findings have indicated the ERAS-BIPN education program to have a beneficial effect on nurses in the intervention group, who can become more competent as a result of their participation. Through this program, nurses can be trained to understand and be skilled in providing ERAS-based Islamic perioperative care to improve the outcomes and spiritual well-being of Muslim patients undergoing surgery. The results have been found to be consistent with previous studies reporting the positive impact of educational programs on spiritual care in enhancing nurses’ competence and reducing perceived barriers [31, 38, 39]. Nurses must strengthen their relevant knowledge to deepen their understanding of ERAS protocols [11], culturally sensitive care, and how to facilitate patients' spiritual needs [15, 21]. This can enable them to integrate spirituality into patient care, provide patient-centered care, and ultimately improve patient satisfaction [14].
Expanding the scope of the ERAS-BIPN educational intervention to more units in hospitals within healthcare organizations could further strengthen the study results. However, this requires consistency across the care team, persistence to ensure compliance, continuous learning, respect for patient values, regular audits as feedback for quality improvement, and discussions regarding evidence-based care [10, 11]. Providing locally relevant information could accelerate the implementation of this program. Healthcare organizations are recommended to establish adequate policies and management support to enhance nurses' competence and professional commitment in providing quality nursing care.
Perioperative nurses' understanding of cultural values related to nursing care must be enhanced from both the patients' and nurses' perspectives [15, 40]. For Muslim patients, Islamic spiritual and cultural values influence their attitudes and behaviors in the hospital, making it essential for nurses to have a comprehensive understanding of these aspects [41]. Nurses should be empowered with the necessary knowledge, attitudes, and culturally competent skills to address Muslim patients’ spiritual needs [28, 33, 34, 37]. The findings obtained may support nursing educational institutions in tailoring the curriculum content with respect to the specific needs of the local context, ensuring nurses are competent in providing evidence-based and culturally sensitive care.
The dynamic nature of healthcare requires nurses to continually update their skills and knowledge. ERAS is not a static set of guidelines; it is a process of continuous refinement and improvement as knowledge evolves [7]. Nurses are responsible for ethical nursing practice, maintaining competence through continuous professional development, and lifelong learning [21]. Education and discussions are essential for transforming traditional practices and fostering a deeper understanding of the relevant evidence of various ERAS elements [8-10], serving as a strategy for multidisciplinary teams to address inconsistencies in daily clinical practice [25].
5. LIMITATIONS
This study has been the first to develop an educational program by adapting the ERAS protocol to the local Indonesian context. Its primary goal was to enhance nurses' competence in evidence-based perioperative care, aligning with the values and beliefs of Muslim patients. Additionally, it aimed to improve the quality of perioperative care and surgical patient satisfaction through a patient-centered approach. However, several limitations of this study should be acknowledged. Specifically, the self-reported questionnaires used for nurse competence assessment may have introduced participant bias. Nurses might have overestimated their competence levels, so the data may not accurately reflect actual skills. Therefore, future research should incorporate a more objective mixed-method competency evaluation to determine accurate competence levels among nurses. Furthermore, additional studies should explore the long-term sustainability of nurse competence and assess the impact of ERAS-BIPN implementation in holistic care on surgical patient recovery outcomes and satisfaction.
CONCLUSION
The observed improvement in post-test scores and the upward trend in outcome data suggested that the ERAS-BIPN education program could be a practical and feasible approach to enhancing nurses’ competence within this study context. Providing educational programs while ensuring alignment with local hospital values is essential to support sustainable and efficient patient care. The findings can be further strengthened by extending the educational intervention to all multidisciplinary teams and implementing more relevant surgical pathways.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: N. and H.K.: Contributed to study conception and design; N.: Contributed to data collection, formal analysis, and writing of the original draft; H.K.: Performed writing, review, and editing, data curation, and validation; M.: Contributed to visualization, data analysis, supervision, designed the methodology and performed writing, review, and editing. All authors have contributed to the analysis, data interpretation, and manuscript revision, and have read and approved the final manuscript.
LIST OF ABBREVIATIONS
| ERAS | = Enhanced Recovery After Surgery |
| ERAS-BIPN | = Enhanced Recovery After Surgery-based Islamic Perioperative Nursing |
| ANOVA | = Analysis of Variance |
| S-CVI | = Scale-content Validity Index |
| FGD | = Focus Group Discussion |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the research ethics committee of General Hospital Dr. Zainoel Abidin, Indonesia (ref.: 115/ETK-RSUDZA/2023).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Participants received prior information about the study and signed the informed consent for their voluntary participation and the participants could withdraw at any time.
AVAILABILITY OF DATA AND MATERIALS
Data generated or analyzed during this study are included in this published article, and supporting data can also be made available by the corresponding author [H.K.] upon special request.
ACKNOWLEDGEMENTS
The authors extend their appreciation to the Ministry of Health of the Republic of Indonesia for providing the doctoral scholarship and to all the nurses for their kind participation in this study. They also thank LH and FH for assisting in data collection, and Cut ZF and TH for their technical support.


