All published articles of this journal are available on ScienceDirect.
The Effect of Abdominal Massage on the Gastric Residual Volume in Adult Patients Admitted in the Intensive Care Unit: A Randomized Controlled Trial
Abstract
Introduction/Objective
Providing optimal nutrition to critically ill ICU patients is crucial yet complex. Enteral feeding is preferred, but food intolerance, often indicated by elevated gastric residual volume, remains a major challenge, highlighting the importance of prevention and effective management as essential nursing responsibilities in critical care settings. Abdominal massage is a potential technique to enhance gastric motility, though evidence from ICU settings remains limited and inconsistent. This study aims to assess the effect of abdominal massage on gastric residual volume in adult ICU patients receiving nasogastric feeding.
Methods
A randomized controlled trial was conducted from January to June 2024 in the ICU of a tertiary care hospital in Lahore, Pakistan. Thirty-four eligible patients were allocated into intervention and control groups (n=17 each). The intervention group received 20-minute abdominal massage sessions twice daily, with an interval of two hours between each abdominal massage session, for three consecutive days. GRV was measured before the first and one hour after the second massage each day.
Results
GRV decreased in the intervention group compared to the control group across all three days. On day one, mean GRV post-intervention was 96.17 ± 30.33 ml vs. 126.47 ± 39.83 ml (p=0.026); on day three, it was 85.00 ± 23.91 ml vs. 127.05 ± 38.97 ml (p <0.001). Within group comparisons showed statistically significant reductions on day two (p=0.010) and day three (p=0.003), but not on day one (p=0.174). However, ANOVA revealed that day-to-day reductions within the intervention group were not statistically significant (p=0.516).
Discussion
The study demonstrated consistent GRV reduction with abdominal massage, supporting previous positive findings, though discrepancies with some studies may relate to differences in technique, duration, and patient profiles.
Conclusion
Abdominal massage may be an effective adjunct for reducing GRV in critically ill patients. Further large-scale studies are needed to validate its routine integration into ICU care.
RCT Clinical Trial Registration No.
Randomized controlled trial conducted in the intensive care unit (ICU), registered at clinicaltrials.gov with ID NCT06062381.
1. INTRODUCTION
Providing adequate nutrition to critically ill patients in the intensive care unit (ICU) is essential for recovery, immune support, and maintaining organ function. Enteral feeding, typically administered via a nasogastric (NG) tube, is the preferred method due to its ability to preserve gastrointestinal integrity and reduce infectious complications [1].
However, gastrointestinal intolerance, including increased gastric residual volume (GRV), is a frequent barrier to successful enteral nutrition in ICU settings. Feeding intolerance is primarily manifested through symptoms such as abdominal distension, nausea, vomiting, constipation, and high GRV. Approximately 66% of ICU patients experience enteral feeding intolerance, which significantly impacts their nutritional intake [2]. Only 43–64% of critically ill patients meet their daily caloric requirements due to such complications. These complications can disrupt enteral feeding and contribute to underfeeding, hindering the holistic management of critically ill patients [3, 4].
Abdominal massage has emerged as a simple, non-invasive nursing intervention aimed at improving gastrointestinal motility and tolerance to enteral feeding. This technique is believed to stimulate peristalsis and enhance parasympathetic activity, potentially reducing GRV and improving feeding tolerance [3, 5]. Some studies suggest its effectiveness in reducing digestive complications, while others report mixed or inconclusive outcomes.
Despite increasing interest in this intervention globally, no randomized controlled trial has been conducted in Pakistan to examine the effect of abdominal massage on GRV in ICU patients. Therefore, this study addresses a critical knowledge gap in the local clinical context and seeks to provide evidence on a low-cost, nurse-led intervention that may improve enteral feeding outcomes in critically ill patients.
2. MATERIAL AND METHODS
2.1. Study Design and Setting
This study was designed as a parallel-group, randomized controlled trial conducted in the intensive care unit (ICU) of a tertiary care hospital in Lahore, Pakistan. The study was carried out from January to June 2024 and was registered at clinicaltrials.gov (Identifier: NCT06062381).
2.2. Sampling Technique and Sample Size
A total of 34 eligible adult ICU patients were recruited using non-probability convenience sampling. Although the study design followed randomized controlled trial principles, the use of convenience sampling may limit external validity and generalizability. The sample size (n=17 per group) was calculated based on previous literature comparing mean GRV levels between groups, with 80% power and 95% confidence [6].
2.3. Randomization Procedure
Participants were randomly assigned to either the intervention or control group through a simple card-drawing method using 34 identical cards (17 labeled “A” and 17 labeled “B”). While this method ensured allocation concealment, it constitutes quasi-randomization and is considered less rigorous than computer-generated randomization. The whole process of enrollment, sample selection, and randomization into intervention and control group I shown in Fig. (1).
2.4. Blinding
Due to the nature of the intervention, blinding of the patients and care providers was not feasible. The outcome assessor was also not blinded due to resource limitations.
2.5. Inclusion and Exclusion Criteria
Included were adult patients aged 18–60 years, with a Glasgow Coma Scale (GCS) score of less than 7 and receiving enteral nutrition via nasogastric tube. Exclusion criteria included recent abdominal surgery, abdominal aortic aneurysm, abdominal radiation within six weeks, current use of pro-kinetic agents, or discharge/death during the study period.
2.6. Data Collection Tool
Data were collected using a researcher-designed proforma, which served as a structured data collection instrument. It included two sections: demographic and clinical information (e.g., age, sex, diagnosis, medications, hospital stay) and daily GRV measurements. The tool was reviewed by a panel of nursing and critical care experts to establish face validity; reliability testing was not formally conducted.
2.7. Intervention
The intervention group received abdominal massage for 20 minutes, twice daily, with a two-hour interval between abdominal massage sessions for three consecutive days. The procedure was performed by the primary researcher, a registered nurse. To ensure consistency, a standard protocol was followed throughout the study. Fidelity was maintained through a standard operating protocol. Although fidelity checks were not formally documented, adherence was ensured by limiting the intervention to a single trained provider.
2.8. Control Group
Patients in the control group received routine ICU care, including GRV monitoring and nasogastric tube placement verification, but no abdominal massage.
2.9. GRV Measurement Procedure
GRV was assessed before the intervention and one hour after the second massage session each day, using a 50 ml syringe to aspirate gastric contents through the nasogastric tube. All aspirated contents were returned to the stomach, and the total GRV was recorded in milliliters.
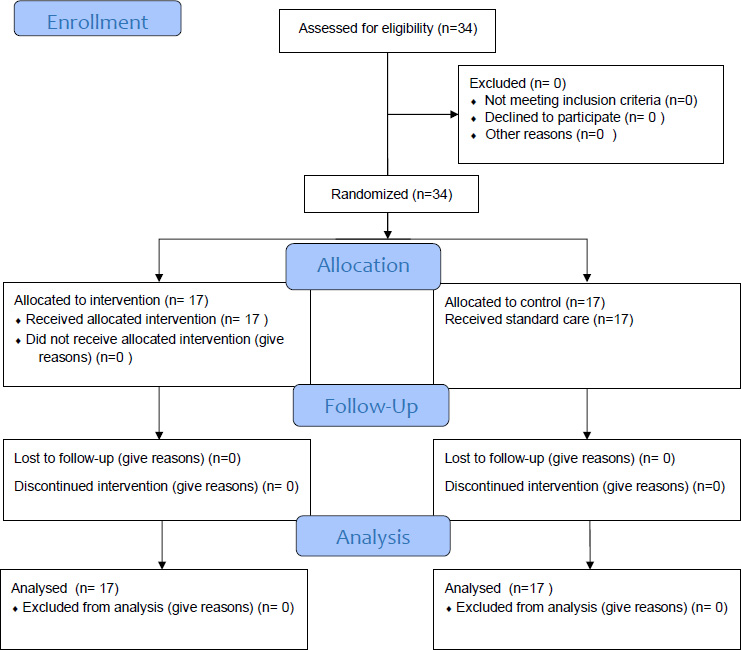
CONSORT flow diagram.
2.10. Ethical Considerations
Ethical approval was obtained from the Institutional Review Board of UHS (Letter No. UHS/DPS/23/523, dated 3rd January 2024) and Jinnah Hospital Lahore (Ref #14/23). Informed consent was secured from the legal guardians of all unconscious patients. Confidentiality and the principles of the Helsinki Declaration were strictly followed.
2.11. Statistical Analysis
Data were analyzed using SPSS version 24. Descriptive statistics (mean, standard deviation, frequencies, percentages) summarized baseline characteristics. The Shapiro-Wilk test checked data normality. Independent t-tests compared mean GRV between groups, paired t-tests evaluated within-group differences, and repeated-measures ANOVA tested GRV trends across three days. Statistical significance was set at p < 0.05.
3. RESULTS
Demographic and clinical characteristics were similar between the intervention and control groups, with no statistically significant differences in age, gender, education, diagnosis, or medication use (p > 0.05), confirming group comparability as shown in Table 1.
| Variables | Intervention Group Frequency (%) | Control Group Frequency (%) | p-value |
|---|---|---|---|
| Age (Years): | |||
| 18-30 | 5 (29.4) | 2 (11.8) | 0.226 |
| 31-40 | 2 (11.8) | 6 (35.3) | |
| 41-50 | 3 (17.6) | 1 (5.9) | |
| 51-60 | 7 (41.2) | 8 (47.0) | |
| Gender: | 0.328 | ||
| Male | 15 (88.2) | 13 (76.5) | |
| Female | 2 (11.8) | 4 (23.5) | |
| Religion: | |||
| Muslim | 16 (94.1) | 15 (88.2) | 0.545 |
| Christian | 1 (5.9) | 2 (11.8) | |
| Educational Qualification: | |||
| No formal education | 2 (11.8) | 5 (29.4) | |
| Primary School | 1 (5.8) | 2 (11.8) | |
| Matric/O level | 6 (35.3) | 3 (17.6) | 0.543 |
| Intermediate/A level | 6 (35.3) | 5 (29.4) | |
| Graduate | 1 (5.9) | 2 (11.8) | |
| Post graduate | 1 (5.9) | 0 (0) | |
| Marital status: | |||
| Single | 4 (23.5) | 1 (5.9) | 0.146 |
| Married | 13 (76.5) | 16 (94.1) | |
| Employment status: | |||
| Unemployed/student | 2 (11.8) | 2 (11.8) | 0.308 |
| Retired | 0 (0) | 1 (5.9) | |
| House wife | 1 (5.8) | 4 (23.5) | |
| Employee | 14 (82.4) | 10 (41.8) | |
| Current medication usage: | 0.227 | ||
| Antacids | 12 | 10 | |
| Antibiotic | 16 | 16 | |
| Epinephrine | 0 | 3 | |
| Length of hospital stay (days): | |||
| 15-May | 14 (82.4) | 11 (64.7) | 0.541 |
| 16-25 | 2 (11.8) | 6 (35.3) | |
| 26-35 | 1 (5.8) | 0 (0) | |
| Medical diagnosis: | |||
| TBI/SDH | 11 (64.7) | 9 (53.0) | 0.426 |
| SOL | 4 (23.5) | 5 (29.4) | |
| RTA | 1 (5.9) | 0 (0) | |
| Others | 1 (5.9) | 3 (17.6) | |
3.1. Comparison of Mean Gastric Residual Volume (GRV) before and after Intervention in both Groups over three Consecutive Days
Shapiro Wilk test was run to assess the normality of the data. The results of the test revealed that the data were normally distributed. Hence, an independent sample t-test was used to compare the GRV between the intervention and control group.
Table 2 reveals the results of an independent sample t-test, which was run to compare the mean GRV between the intervention and control group across three consecutive days. The intervention group, which received abdominal massage, demonstrated a progressive reduction in GRV from Day 1 to Day 3. In contrast, the control group maintained consistently higher GRV levels. Statistically significant differences between the two groups were observed on Day 1 (p=0.026), Day 2 (p=0.004), and Day 3 (p <0.001). The findings suggest that abdominal massage effectively reduces GRV in critically ill patients receiving enteral nutrition.
3.2. Comparison of Mean GRV before and after Intervention in the Intervention Group over three Consecutive Days
Table 3 shows the results of the paired sample t-test of the intervention group. A paired sample t-test was run to compare the mean GRV before and after intervention.
| Days |
Intervention Group (Mean ±SD, ml) |
Control Group (Mean ±SD, ml) |
Test statistic | p-value |
|---|---|---|---|---|
| Day one | 96.17±30.33 | 126.47±39.83 | 0.247 | 0.026* |
| Day two | 92.05±30.57 | 130.00±40.00 | 3.107 | 0.004* |
| Day three | 85.00±23.91 | 127.05±38.97 | 3.792 | <0.001* |
| Intervention Group | Mean GRV | Pre (Mean ±SD, ml) | Post (Mean ±SD, ml) | Test statistic | p-value |
|---|---|---|---|---|---|
| Day one | 101.47±24.67 | 96.17±30.33 | 1.421 | 0.174 | |
| Day Two | 95.58±27.26 | 92.05±30.57 | 2.748 | 0.010* | |
| Day three | 100.88±20.01 | 85.00±23.91 | 3.421 | 0.003* |
| Control Group | Mean GRV | Before Mean ±SD | After Mean ±SD | Test Statistic | p-value |
|---|---|---|---|---|---|
| Day one | 103.82±23.68 | 126.47±39.83 | 2.748 | 0.014* | |
| Day Two | 105.88±33.41) | 130.00±40.00) | 4.544 | <0.001* | |
| Day three | 111.47±27.31) | 127.05±38.97) | 3.021 | 0.008* |
| Day | Mean ± SD (ml) | F statistics | p-value |
|---|---|---|---|
| Baseline | 101.47± 24.67 | 0.671 | 0.516 |
| Day 1 | 96.17± 30.33 | ||
| Day 2 | 92.05± 30.57 | ||
| Day 3 | 85.00± 23.91 |
It is evident from the table that on the first day, in the intervention group, the mean GRV before the intervention was 101.47±24.67ml, and it declined to 96.17±30.33ml, but this difference was not statistically significant (p-value=0.174). However, on the second day, the mean GRV before intervention was 95.58±27.26ml, and it was reduced to 92.05±30.57ml with a statistically significant difference (p-value=0.01), and consistently on the third day, the mean GRV declined from 100.58±20.01ml (before intervention) to 85.00±23.91ml (after intervention), and this difference was statistically significant (p-value <0.01).
Table 4 shows the results of the paired sample t-test of the control group. A paired sample t-test was run to compare the mean GRV before feeding and three hours after (without giving any intervention). It is evident from the table that on the first day, the mean GRV increased from 103.82±23.6ml to 126.47±39.83ml, and this increase was statistically significant (p-value=0.014). Similarly, on the second day, the mean GRV was increased from 105.88±33.4ml (before) to 130.00±40.00ml (after) with a statistically significant difference (p-value<0.001), and consistently on the third day, the mean GRV was increased from 111.47±27.31ml (before intervention) to 127.05±38.9ml (3 hours later), and this difference was also statistically significant (p-value=0.008).
3.3. Comparison of GRV on 1st, 2nd, and 3rd day after Intervention in the Intervention Group
As data was normally distributed, one-way analysis of variance (ANOVA) was conducted to compare the mean residual volume on the first day, at second day, and third day in the intervention group.
Table 5 indicates the result of ANOVA, which was conducted to compare the mean residual volume at baseline, first, second, and third day in the intervention group (N=17). It is obvious from the table that the mean GRV of the intervention group at baseline was 101.47ml, and after abdominal massage on day one, it was 96.17 ml. It was decreased to 92.05 ml at day 2, and it was further reduced to 85.00 ml at day 3.
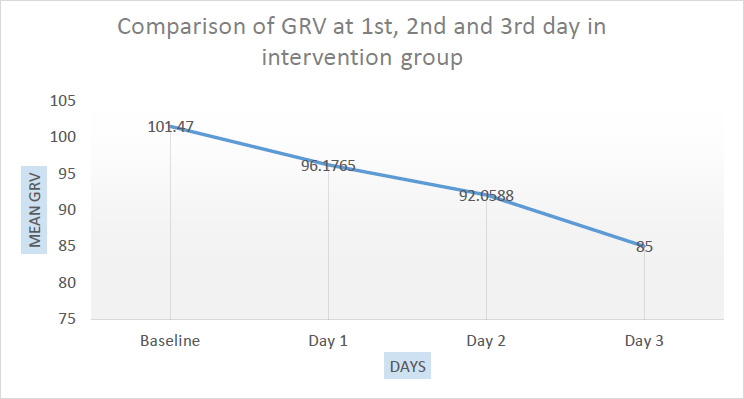
GRV trend across three days (post-intervention values) in the intervention group.
The results of ANOVA indicated no significant difference between the days (P-value =0.516). Thus, there is no significant evidence to reject the null hypothesis. A graphical representation of the comparison of mean GRV at 1st, 2nd, and 3rd day after intervention in the intervention group is given in Fig. (2).
4. DISCUSSION
Optimal nutrition is essential for critically ill patients in the ICU, as it supports healing and the immune system, particularly during the early stages of admission when catabolism rapidly depletes nutritional status [7]. This study examined the effect of abdominal massage on gastric residual volume in critically ill patients receiving nasogastric feeding. The findings indicated a reduction in GRV among the intervention group, particularly on the second and third days of massage. These results align with previous studies [6, 8-10], suggesting that abdominal massage may facilitate gastrointestinal motility and improve feeding tolerance.
Abdominal massage may enhance gastric emptying through several mechanisms. Mechanically, it stimulates peristaltic activity by applying external pressure to the intestines. Neurologically, massage may enhance vagal tone, which promotes parasympathetic activity and improves motility in the gastrointestinal tract. These physiological responses can lead to more effective gastric emptying and reduced residual volume [11, 12].
While the reduction in GRV is statistically significant, its clinical impact must be interpreted cautiously. Lower GRV may reduce the risk of aspiration, enhance tolerance to enteral nutrition, and improve nutrient delivery, all of which are critical in ICU care. However, there remains no universal GRV threshold for defining intolerance. Hence, future studies should explore how GRV reduction translates to outcomes such as reduced aspiration pneumonia or improved caloric intake.
The findings of this study were partially consistent with prior trials. Some studies did not find significant differences between groups, which could be attributed to differences in population age, massage technique, or intervention duration [13, 14]. Our study contributes new data from Pakistan, where such trials are lacking, and supports further evaluation of abdominal massage in clinical settings.
This study has several limitations. First, convenience sampling and quasi-randomization may introduce selection bias, limiting external validity. Second, the intervention was delivered by a single researcher, introducing potential operator and performance bias. Third, the outcome assessors were not blinded to the group allocations. Lastly, the sample size was small, and the duration of follow-up was limited to three days, preventing assessment of long-term clinical outcomes.
CONCLUSION
This randomized controlled trial suggests that abdominal massage may be a useful adjunct to standard care in reducing gastric residual volume in ICU patients receiving nasogastric feeding. Although GRV was lower in the intervention group across all three days, day-to-day reductions were not statistically significant when analyzed via ANOVA. Given the study’s limitations, including small sample size, quasi-randomization, lack of blinding, and short follow-up, these results should be interpreted with caution. Future large-scale, multi-center studies are recommended to confirm the findings and evaluate the long-term clinical impact of abdominal massage on feeding tolerance and patient outcomes.
RECOMMENDATIONS & IMPLICATIONS
Clinical Recommendations
- Abdominal massage may be integrated into ICU nursing protocols as a supportive measure to improve enteral feeding tolerance.
- Training programs should be developed to ensure the correct and standardized application of abdominal massage techniques.
- Consideration should be given to cost-effectiveness, feasibility, and safety before routine implementation.
Research Implications
- Conduct multi-center randomized controlled trials with larger sample sizes and longer follow-up durations.
- Investigate the relationship between GRV reduction and patient-centered outcomes such as aspiration rates, caloric adequacy, ICU length of stay, and mortality.
- Include intervention fidelity checks and blinded outcome assessment in future studies for improved rigor.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.J., H.S.K., S.K.: Study Conception and Design; M.B.M., M.J., F.S.: Data collection; M.J.: Analysis and interpretation of results, Draft manuscript. All Authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| GRV | = gastric residual volume |
| ANOVA | = Analysis of variance |
| ICU | = Intensive care Unit |
| UHS | = University of Health Sciences. |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was reviewed and approved by the Institutional Review Board of the University of Health Sciences (UHS), Lahore, Pakistan (Letter No. UHS/DPS/23/523, dated 3rd January 2024) and by the Ethical Review Board of Jinnah Hospital, Lahore, Pakistan (Ref #14/23).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
A written informed consent in both English and Urdu was obtained from the relatives/legal guardians of the patients in the ICU.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of our article has been deposited in the Zenodo Repository at https://doi.org/10.5281/zenodo.17033855, reference number 10.5281/zenodo.17033855.”
ACKNOWLEDGEMENTS
My heartfelt thanks go to my supervisor, Dr. H. S. K., for her invaluable guidance and support. I also extend my sincere appreciation to Prof. S. K., Prof. F. S., and Hafiz M. B. M. for their assistance and contributions, which played a vital role in the successful completion of this study.


