All published articles of this journal are available on ScienceDirect.
Injection Considerations for Administering Endocrine Parenteral Therapies to Children
Abstract
Introduction
Early diagnosis of chronic endocrine conditions requiring injectable treatment is common, and injections may cause children to experience uncomfortable feelings (e.g., pain and anxiety). No recent publications have comprehensively described good nursing practices for pediatric injections. This review identifies key factors that can facilitate improved injection techniques and ideal treatment options for children, with a focus on endocrine parenteral therapies.
Methods
PubMed, Embase, and CINAHL were searched. MeSH search terms included “child,” “injections/methods,” “pain/prevention and control,” “pain management/methods,” “patient positioning,” and “analgesic/therapeutic use.” Literature related to interventions pediatric nurses can implement to decrease injection-related discomfort and other treatment factors that can minimize injection-related pain was included.
Results
Nurses should build a strong rapport with the child and/or caregiver, as this can improve the expectations for the injection experience. Nurses can assist caregivers with selecting the most appropriate treatment and provide options that may reduce out-of-pocket costs. Before administering an injection, nurses should check the “Five Rights,” assess skin to select an appropriate injection site, and prepare skin for injection. Good injection techniques include: administration of room temperature medications, comforting positioning and holding of the child by the caregiver, distraction activities, and local anesthetic agents. In addition to using good pediatric injection techniques, nurses can partner with Certified Child Life Specialists when available to help alleviate the child’s anxiousness.
Conclusion
Optimal pre-, during, and post-injection techniques, along with proper education and care, can reduce pain and anxiety in children, improve caregivers’ experiences, and prevent treatment delays.
1. INTRODUCTION
Children tend to be more pain-sensitive than adults [1] and frequently experience fear in healthcare settings [2, 3]. Not only can injection-related pain and anxiety negatively impact treatment experience, but these feelings can also delay medical treatment and/or prolong treatment administration [2]. If treatment is delayed, children with endocrine conditions, e.g., growth hormone deficiency or Central Precocious Puberty (CPP), may experience psychosocial barriers like depression [4] and anxiety [4], and developmental barriers like shorter adult stature [4] and pubertal advancement [5, 6].
Pediatric nurses should strive to minimize iatrogenic anxiety and trauma as proper injection techniques reduce pain and create positive healthcare experiences for children and caregivers [2]. Optimal pre-, during, and post-injection techniques, education, and care can improve the pediatric patient experience, treatment efficacy [7], and potentially adherence. However, our review of the current literature found that no recent publications have comprehensively described good nursing practices for pediatric injections. Therefore, there is a need for a practical, comprehensive overview of key factors for optimal pediatric injection practices. The objective of this narrative review is to provide a useful reference for nurses and clinicians, offering guidance on anesthetics, distraction techniques, appropriate administration routes, injection sites, and needle characteristics (length and gauge) (Table 1) [8-23], as well as collaborating with expert child life specialists.
| - | Examples | Considerations |
|---|---|---|
| Needle size (length and gauge) | • SC insulin: 4 mm, 5 mm, or 6 mm pen needle • SC leuprolide acetate: 0.625-inch, 18 gauge [8] • SC human growth hormone: 0.156-inch, 31-gauge [9] • IM triptorelin: 1.5-inch, 21 gauge [10] • IM medroxyprogesterone acetate: 1.5-inch, 22-gauge [11] |
• Needles are typically supplied with the medications and chosen according to regulatory standards based on testing • The appropriate needle is dependent on the type, volume, and viscosity of the medication • Shorter needles may be preferred over longer needles [12] and may also be less visually frightening |
| Injection volume | • IM injections o Maximum of 3 mL in children between 1 and 15 years old [13] o IM leuprolide acetate: 1 ML for 1-month, 1.5 mL for 3- and 6-month [14] • SC injections o Maximum of 2 mL in children 12 months and older [13] o SC leuprolide acetate: 0.375 mL [8] |
• Large injection volumes tend to produce more pain and discomfort [15] • Pain can be resolved by administering a non-aspirin analgesic after IM injections |
| Intramuscular injection | • Testosterone • Glucagon • Glucocorticoids/hydrocortisone • Leuprolide acetate • Triptorelin pamoate • Medroxyprogesterone acetate |
• Injection site o Deltoid (shoulder) is preferred if muscle mass is adequately developed [16] o Vastus lateralis (thigh) is recommended for infants, toddlers, or young children with inadequately developed shoulder muscle mass [17, 18] • Avoid usage in patients with bleeding disorders (e.g., hemophilia) if possible due to the risk of hematomas [19] • Avoid multiple injections in the same limb [19] • May not be preferred for children who are thinner and/or have low muscle mass [16, 20] |
| Subcutaneous injection | • Insulin • Leuprolide acetate • Growth hormones • Octreotide • Insulin-like Growth Factors (IGF-1) • Steroids • Testosterone • Medroxyprogesterone acetate |
• May be administered at any site with adequate SC tissue [20] • May be less painful [21] and carry a lower risk of bone and nerve injury [22] compared to IM injections |
| Implants or infusion set | • Histrelin • Insulin (administered via pumps through infusion sets) |
• May be a suitable option for children with extreme needle phobia, special needs children who cannot tolerate injections, or families for whom more frequent clinic visits are problematic • Compared to injections, implantation procedures are more complicated and may require minor surgery with anesthesia for insertion or removal [23] • Local reactions such as bruising, pain, soreness, erythema, and swelling may occur after implant insertion [23] • Increased risk for infection |
| Safe, comforting positioning and holding | • See Fig. (3) for illustrations of suggested holds | • Safely prevents the child from moving their arms and legs • Avoids frightening the child by embracing rather than overpowering them • Allows the nurse or caregiver steady control of the limb and injection site |
| Distraction and pain management techniques | • Casual conversation • Slow and deep breathing • Distraction devices (e.g., vibrating devices, distraction cards, etc.), video, screens • Skin refrigerant or vapocoolant sprays • Oral sucrose |
• Refrigerant sprays, ice packs, or ice cubes are contraindicated in patients with underlying sensitivities to cold and ice • Oral sucrose is contraindicated in children with sucrose and fructose intolerance and glucose-galactose malabsorption |
| Local anesthetic agents | • ELA-Max® (4% liposomal lidocaine cream) • Maxilene™ (4% lidocaine cream) • EMLA® (2.5% lidocaine with 2.5% prilocaine cream) • Ametop® gel (4% amethocaine/tetracaine), J-Tip needle-free injection |
• Use of different local anesthetic agents may reduce the potential to develop tolerance to any one type • Should not be used with frequent injections |
2. MATERIALS AND METHODS
2.1. Search Strategy
A comprehensive search was conducted across three databases (PubMed, Embase, and CINAHL) from February to April 2023. The search utilized MeSH terms including “child,” “injections/methods,” “pain/prevention and control,” “pain management/methods,” “patient positioning,” and “analgesic/therapeutic use.” Both original research and reviews were eligible for inclusion.
Inclusion criteria were: English language, pediatric population, interventions by pediatric nurses to reduce injection-related discomfort and anxiety, and literature on treatment factors minimizing injection pain. Exclusion criteria were: non-English literature, non-pediatric population, and non-parenteral endocrine therapies.
2.2. Search Outcome
Two authors initially screened all records. Titles and abstracts of relevant studies were reviewed, with full texts assessed if abstracts indicated that the studies addressed interventions or treatment factors related to reducing injection-related discomfort and anxiety in children. Studies meeting the eligibility criteria were included in the review. The most current literature was included wherever possible. Of the thousands of publications captured in the initial search, 76 studies were selected for inclusion (Supplementary Fig. 1). The reference lists of relevant studies were examined manually to identify additional relevant studies. Main exclusions were incorrect outcome and incorrect therapy type.
2.3. Data Extraction and Synthesis
In the first phase of data extraction and synthesis, two authors independently extracted individual key findings from the 76 studies selected. These key findings were consolidated into five key factors affecting the injection experience for children and their caregivers. The synthesized key factors and the related subthemes are described below.
2.4. Strong Rapport Between Nurses and Patients/Caregivers May Improve Treatment Experience
Strong nurse-patient and nurse-caregiver relationships enhance care quality and the treatment experience. Nurses can utilize the “6 Cs”-care, commitment, compassion, courage, competence, and communication-as a framework to prioritize children’s needs while empowering their families [24]. For example, open communication between a nurse and a child fosters trust and empowers children to participate in their injection routine, involving them in tasks like site selection or supply preparation when age appropriate. Additionally, nurses can demonstrate compassion for caregivers, who also experience feelings of anxiety and helplessness, by guiding them to praise their children’s treatment successes [25].
For injections provided by caregivers, caregivers will likely need to learn new skills to ensure correct medication administration, and a strong rapport with nurses can improve knowledge acquisition and retention. Teaching plans for caregivers should adhere to adult learning theory [26], emphasizing a tailored, dialogue-based approach. Nurses should describe the rationale behind each step, emphasizing the importance of correct injection administration and the consequences of errors. Considering caregivers’ time constraints, pediatric nurses can structure training sessions within manageable time frames, recognizing the challenge of retaining procedural information. Various techniques, such as written materials [27], audiovisual aids [28], and computer-assisted instruction [29], may enhance caregivers’ knowledge retention. For practical skills, such as proper injection techniques, nurses should encourage hands-on learning by demonstrating the skill in the clinic and asking caregivers to demonstrate the new skill under guidance so they can correct any errors. This method will not only increase caregiver competence but may also help address needle phobias or psychological barriers that prevent caregivers from administering an injection to their child. Nurses may also use educational resources such as booklets with graphics [30] and instructional videos to support learning.
2.5. Factors in Treatment Selection
2.5.1. Product Composition
Medication components, including preservatives and medication composition characteristics like depot or gel-developing formulations, may induce pain or adverse reactions [31]. Factors affecting injection-site pain, such as concentration, osmolality, viscosity, pH, preservatives, and buffers, should be considered in product composition [31]. While current literature lacks studies evaluating the prolonged impact of these components on children’s injection experiences, it is crucial to recognize their potential influence during both initial and ongoing injections.
2.5.2. Duration of Action/Frequency of Injection
Longer-acting formulations reduce office visits, minimizing disruptions at school and work. More frequent injections demand more time off, potentially increasing stress, and the children may still need to visit the office for routine health check-ups between injection appointments. This frequency could lead to negative associations between office visits and injections, potentially increasing their fear and anxiety in healthcare settings.
Shorter-acting medications pose a higher non-adherence risk, potentially reducing treatment efficacy. Although no current studies on gonadotropin-releasing hormone agonist administration were found during the literature search, a 2007 retrospective study reported 74% non-adherence with 1-month Intramuscular (IM) Leuprolide Acetate (LA) for CPP, suggesting inadequate control for most children with CPP on monthly depot LA [32]. However, more recent studies on growth hormone therapy, typically injected daily, reported 43% non-adherence in children and 42% in adolescents, with “forgetting to take the injection” and “exhaustion from long-term injections” as key factors to low adherence [33]. The authors recommended longer-duration growth hormone prescriptions to improve adherence [33]. Additionally, an analysis comparing non-adherence risk for 1-, 3-, 4-, and 6-month injections found that the expected proportion of late injections per year was much higher for 1-month formulations compared to 6-month (45% vs. 28%) [34]. Although this study evaluated data from adults [34], not children, the results support that longer-acting formulations reduce the potential for non-adherence.
Long-acting therapies like yearly histrelin implants also carry non-adherence risk, as shown in case reports where children lost to follow-up retained implants for up to 7 years [35, 36]. Thus, it is important to balance the use of an appropriately long-acting agent, which can improve adherence, with adequate monitoring or in-person visits.
2.5.3. Needle Characteristics (Length and Gauge)
The manufacturer typically determines the needle length and gauge size based on the medication type, volume, and viscosity. Needles provided with injectable medication packages are selected in accordance with regulatory standards and approvals from product testing and clinical trials. Substituting needles may not be recommended or appropriate and could negatively impact the child’s injection experience or treatment efficacy. Intramuscular injections typically require longer needles for deep-muscle medication delivery, while Subcutaneous (SC) injections often use shorter needles to prevent inadvertent IM injection. Higher-viscosity formulations may necessitate wider-gauge needles for optimal product flow, and needle substitution can impact efficacy. Shorter needles may be preferred for their less intimidating appearance. When options are available, nurses can consider factors such as the child’s age, weight, and whether the skin at the injection site should be pulled taut or bunched (typically different between IM and SC routes).
Needle characteristics are key factors that impact the child’s and/or caregiver’s injection experience, though literature is limited. Pediatric studies on needle size yield mixed results [12, 37], with one study recommending the shortest option (4mm) for SC insulin injections to minimize inadvertent IM injections and glycemic variability [12] and another study finding local reactions to be significantly reduced with a 23 gauge, 25mm needle compared to a 25 gauge, 16mm needle for IM injections [37]. Although it may be standard of practice to use the needle supplied and approved for the medication, adjustments may be made for pediatric patients, especially in cases of off-label medication use or when only adult formulations/ medication kits are available, provided safety and efficacy are maintained. If there is any uncertainty about the use of alternative needle sizes on efficacy, consulting the manufacturer is advised, and close monitoring is crucial when adjustments are made, especially for pediatric patients and/or off-label medication use.
2.5.4. Injection Volume
Large injection volumes can cause more pain and discomfort during and potentially after the injection. A study on adults with diabetes evaluating injection volume, speed, and site on pain sensation found that larger volumes were associated with increased pain [15]. One proposed explanation for heightened pain with larger volumes is the different spatial distribution of injected fluid within the SC space, where more fluid is placed in the densely innervated fascia between the deep and superficial SC fat layers [15]. In the event of pain after an IM injection, caregivers can consult clinicians for appropriate measures to relieve pain (e.g., non-aspirin analgesic medications). Pediatric guidelines recommend a maximum injection volume of 2 mL for SC injections in children 12 months and older, and 3 mL for IM injections in children between 1 and 15 years old [13]. However, nurses should recognize that at maximum injection volumes, SC and IM injections will be more painful compared to lower volumes.
2.5.5. Administration Route
The administration route (IM, SC, or implant) is crucial in therapy choice. Intramuscular injections offer rapid medication absorption, while SC injections have slower, steadier rates due to a combination of the medication delivery system or formulation and the administration route. For children unable to tolerate injections, require treatment for many years, or families who cannot visit clinics often, implants may be a good option.
Intramuscular injections allow rapid drug absorption and allow larger medication volumes to enter well-vascularized muscles, bypassing first-pass metabolism [17]. Common IM pediatric endocrine medications include testosterone, depot gonadotropin-releasing hormone agonists like LA and triptorelin pamoate, and medroxyprogesterone acetate. When selecting an injection site, factors like the child’s age, muscle development, and medication volume should be considered, while also avoiding major nerves and blood vessels [16, 38]. For children with sufficient shoulder muscle development, the deltoid (shoulder) is preferred and is best for low-volume injections (≤ 1mL) [16] (Fig. 1 [20]). For infants and young children with less developed shoulder muscles, the vastus lateralis (thigh) is recommended [17] (Fig. 1 [20]). In adolescents, both the ventrogluteal (hip) and deltoid sites are appropriate [39] (Fig. 1 [20]). However, IM injections may not be ideal for children who are thinner or have low muscle mass [20].
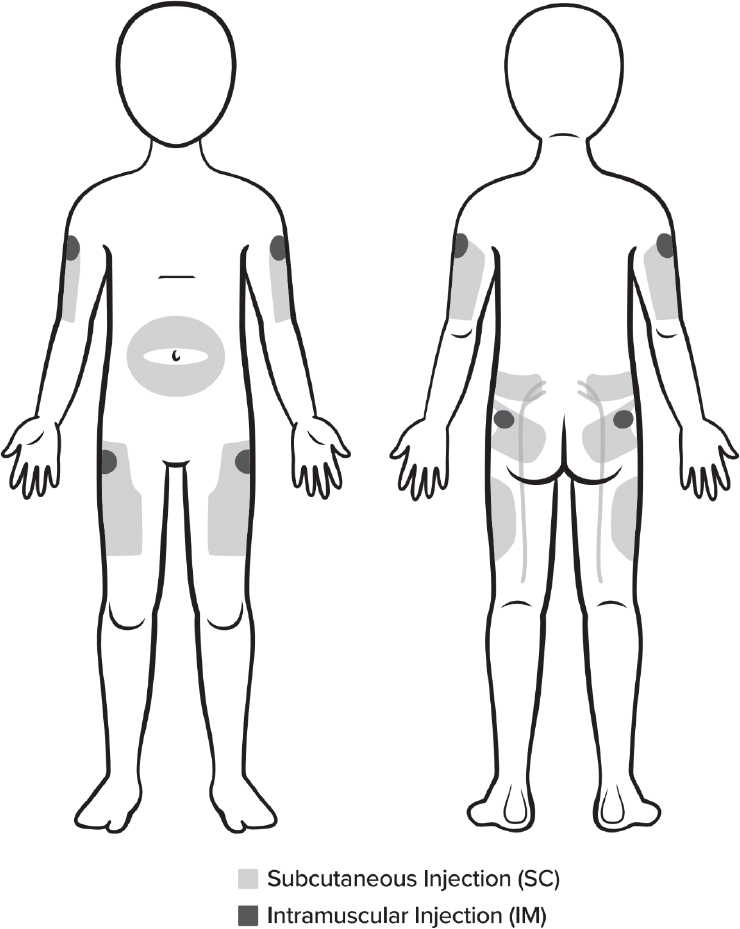
Potential injection sites for intramuscular and subcutaneous medications [20].
For patients at risk of bleeding, SC or intradermal routes are preferred over IM to avoid hematomas [19]. Multiple IM injections in the same limb should be spaced 1 to 2 inches apart to prevent overlapping reactions, with the vastus lateralis preferred if necessary [19]. Intramuscular injection complications include erythema, pain, muscle atrophy, bone injury, cellulitis, sterile abscesses, and nerve injury, while SC injection complications include pain and skin disorders like lipohypertrophy and lipoatrophy [40, 41]. The Centers for Disease Control and Prevention (CDC) advises that aspiration before IM injection is unnecessary due to the absence of large blood vessels [42], though some medication labels recommend avoiding injection if blood is aspirated [14].
For SC injections, medication is injected into the fat and connective tissue below the dermis, where lower blood flow results in slower, sustained absorption of the medication compared to IM injections [43]. Subcutaneous injections are suitable when steady absorption is desired [43], making them commonly used for medications like insulin, LA, growth hormones, octreotide, diazoxide, Insulin-like Growth Factors (IGF-1), steroids, testosterone, and medroxyprogesterone acetate. Subcutaneous injections can be administered at any site with adequate subcutaneous tissue, often chosen for convenience and a lower risk of pain compared to IM injections [20]. Typical sites for patients over 12 months include the buttocks, thigh, triceps, and abdomen (Fig. 1) [44, 45].
Compared to IM injections, SC injections may be less painful and have a lower risk of bone or nerve injury due to fewer muscle fibers and a protective fat layer [22]. Factors reducing pain for SC injections include short, thin, lubricated needles with sharp tips; abdominal injections tend to be less painful than thigh injections and are well tolerated up to 3mL [31].
Research in children suggests a preference for SC over IM injections. A comparison of SC and IM injections in a pediatric population showed a preference for SC injections for chronic treatments like growth hormone, with similar growth rates reported for SC and IM routes [46]. A separate survey of children and caregivers highlighted gaps in injection training, with 27% of children not receiving training in the last 12 months, underscoring the importance of continuous education on correct injection techniques [47].
Implants like histrelin implants and insulin pumps may benefit children with needle phobia, special needs, or families facing challenges with frequent clinic visits. Unlike injections, implantation is more complex and may require minor surgery with anesthesia, with 3% experiencing anesthesia-related complications [23]. Preoperative anxiety, affecting 42-75% of children, can be managed through age-appropriate support and preparation and evidence-based methods such as virtual reality and music therapy, where available [48, 49]. Common post-insertion reactions include bruising, pain, and swelling [23].
Pediatric studies on implants reveal significant challenges. Histrelin implants demonstrate up to 28% breakage during removal [50], and a 10-year study noted the hemostat in the medication kit was inadequate for proper insertion, especially during suturing or a delicate extraction [51]. Over a 16-week period, a prospective study on modern insulin pumps found that adverse events occurred in 11% of children, with 32% requiring hospital admission or emergency department attendance [52]. A 14-year review of insulin pump adverse events in children aged 1 to 12 years found 43% of adverse events led to hospitalization, mainly for diabetic ketoacidosis or hyperglycemia [53]. Additionally, problems related to patient education and device misuse were identified [53], indicating the need to improve device-use training for children and caregivers and to provide ongoing education throughout treatment.
2.5.6. Adverse Event Profiles
Therapies with distinct administration routes exhibit varied adverse event profiles. In children, implant breakage has been reported [50], and sterile abscesses may follow IM injections and implants [54, 55]. Children receiving insulin injections may experience bleeding, pain, bruising, allergies, and lipohypertrophy [56]. Lipohypertrophy is more prevalent in children receiving multiple daily injections, higher median insulin doses, and frequent hypoglycemia [56]. Although rare, lipoatrophy may occur, affecting insulin absorption [57]. Switching to a lower-risk formulation is advisable if specific adverse events like sterile abscesses are noted.
2.5.7. Financial Considerations
Out-of-pocket expenditures influence caregivers’ treatment decisions, and nurses can provide guidance on cost-reduction options. While insurance coverage typically determines costs, manufacturers may offer programs to reduce out-of-pocket expenses, e.g., cards that can be used toward copays and/or deductibles. These programs can assist uninsured caregivers, medications not covered by insurance, or while awaiting specialty coverage. Pediatric nurses play a crucial role in educating caregivers on these resources. To address the costs of frequent clinic visits, clinicians and nurses can adjust monitoring schedules and consider options like home visits, sponsored home injection programs, or telemedicine to ensure continuity of care [58].
2.6. Nursing Considerations for In-clinic Pediatric Injections
2.6.1. Pre-injection Assessments and Preparation
Although other healthcare providers (e.g., prescribers and pharmacists) share the responsibility of ensuring correct medication administration, nurses should perform the ‘Five Rights’ of medication administration: right patient, right drug, right route, right time, and the right dose (Fig. 2 [59]) for each medication administration [59]. This proactive approach reduces the risk of potentially irreversible medication errors. Nurses should also confirm the reason for the medication and check allergies.
Skin assessment before injection should include a visual and tactile examination to avoid bruising, scarred, fibrous SC tissue, or compressed areas [8], and the injection site must be free from inflammation or lipohypertrophy [60]. Rotation of injection sites helps prevent site complications.
2.6.2. Good Pediatric Injection Technique
2.6.2.1. Medication Temperature
It is preferred to administer medications at room temperature, if possible, as injecting chilled medication can cause pain [61]. Additionally, allowing a medication to reach room temperature before reconstitution is a requirement for the proper preparation of some medications [8]. Nurses can help ensure that enough time is scheduled for medications to reach room temperature before each child’s injection appointment.
2.6.2.2. Safe, Comforting Positioning and Holding
Appropriate positioning and holding of the child by a caregiver during injections can offer several benefits. This safely prevents the child from moving, avoids frightening the child by embracing rather than overpowering them, and allows the nurse or caregiver steady control of the limb and injection site. Suggested holds vary depending on the age and size of the child (Fig. 3a-c) [62, 63].
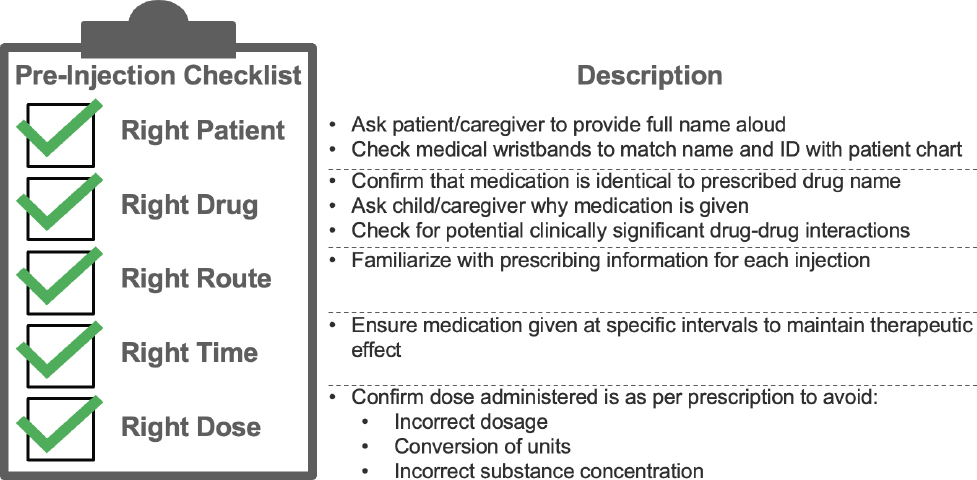
Nurses should confirm the “5 rights” of medication administration before each injection [59].
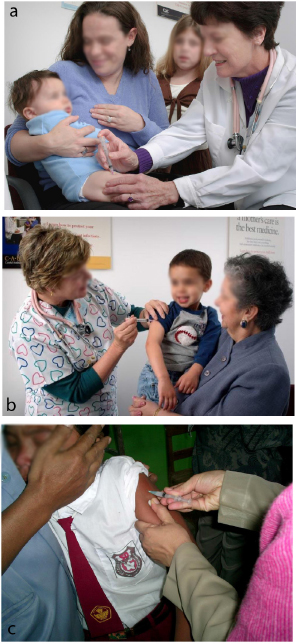
Suggested holds for children receiving injections [62].
a. Figure of infants/toddlers receiving an injection in a leg.
Source: https://phil.cdc.gov/Details.aspx?pid=9353
b. Figure of older children receiving an injection in an arm [62].
Source: https://phil.cdc.gov/Details.aspx?pid=9304
c. Figure of toddler/preschoolers who are fearful of needles [63].
Source: https://phil.cdc.gov/Details.aspx?pid=19847
2.6.2.3. Distraction and Pain Management Techniques
Non-pharmacological distraction and pain management techniques are effective in relieving needle-related pain and distress in children [64]. Many healthcare centers offer programs or staff to enhance injection experiences [65].
Common distraction methods include deep breathing, conversation, picture cards, and devices like BUZZY® for numbing [66, 67].
Topical agents such as vapocoolant sprays (e.g., Pain Ease®) and ice packs can quickly ease pain but are unsuitable for patients with cold sensitivities [68].
Oral sucrose provides mild pain relief in infants under 28 days old but is contraindicated in children with sucrose intolerance, fructose intolerance, and glucose-galactose malabsorption and should be used with caution in children with other conditions that limit oral sucrose intake [69, 70].
2.6.2.4. Local Anesthetic Agents
Local anesthetics have varying side effects. ELA-Max® (4% liposomal lidocaine cream) is applied 30 minutes pre-injection, with skin pallor reported in 7-12% of children [71]. Maxilene™ (4% lidocaine cream) is an alternative. EMLA® (2.5% lidocaine and 2.5% prilocaine cream) requires at least a 1-hour pre-application and may cause vasoconstriction [72], though it may work faster for SC injections. Ametop® gel (4% amethocaine/tetracaine), unavailable in the U.S., requires application 30-45 minutes before venipuncture and venous cannulation and may cause slight erythema at the application site [73, 74]. Local anesthetics can improve pain tolerance, but waiting for them to take effect may cause anxiety. Ice or fast-acting skin refrigerants might be more effective and economical. Nurses can advise caregivers on anesthetic options for home use or prior to appointments. Though typically used more for IM injections, studies in children suggest that while effective, local anesthetics are generally not recommended for daily or frequent injections. A meta-analysis found that topical anesthetics reduce injection pain for both IM and SC injections [75]. Rarely, immediate hypersensitivity reactions have been reported, with multiple exposures (≥ 2) being a predictive factor [76].
2.6.2.5. Post-injection Care
Nurses can guide caregivers in minimizing post-injection discomfort. Caregivers should be advised to avoid massaging the injection site unless directed [77]. A cool, damp cloth can ease redness and swelling, and a lukewarm bath can help with mild fever [78]. If fever persists, caregivers may consider antipyretics after consulting a Healthcare Provider (HCP). Ensuring adequate hydration is also recommended [78].
2.7. Teaching Children to Self-Administer Injections and Improving Adherence to Self-Administered Injections
When appropriate, nurses can teach children self-injection techniques and empower them to feel more in control of their treatment [79]. Pediatric educational strategies, like therapeutic play, have been shown to help children understand medical procedures, such as injections [80-82]. In a pilot study evaluating the effectiveness of a therapeutic play intervention to teach children with type 1 diabetes to correctly perform their insulin injections, children improved their injection skills by using stories, demonstrations on dolls, and hands-on practice [81]. After the intervention, children's injection scores significantly improved [81].
Caregivers and HCPs should support and supervise children in self-injecting, ensuring timely administration, and promoting adherence through educational, technological, and psychosocial interventions. Nurses should guide caregivers on realistic expectations for self-sufficiency. Due to specialized techniques and risks, complex medications require administration by trained HCPs, and home administration should only be conducted by experienced, trained family members.
2.8. Child Life Specialists Can Help Reduce Pain and Distress During Injections
Nurses can also collaborate with Certified Child Life Specialists (CCLSs) to provide support through education, preparation, play therapy, and distraction techniques, which can help children manage the stress of medical procedures [83]. The American Academy of Pediatrics endorsed CCLS support in 2021, highlighting their role in educating healthcare teams and supporting patient-centered practices [84]. A study found CCLS presence during injections led to more pain-relieving practices and reduced distress in children receiving injections [83]. Nurses can advocate for CCLS inclusion in pediatric care to improve pediatric patients' and their caregivers' overall injection experience.
3. LIMITATIONS
This narrative review has some limitations. First, our review does not provide definitive, evidence-based guidelines on best practices for pediatric injections. Rather, the aim was to provide a practical and accessible synthesis of diverse literature that enables readers to quickly gain an overview of pediatric injection techniques – potentially enhancing the experience for children, caregivers, and healthcare providers. Additionally, the literature included in this review does not constitute an exhaustive list of published studies relevant to best practices for pediatric injections. We prioritized recent publications to ensure the information presented was up-to-date. Lastly, our review may not be as easily reproducible as a systematic review; however, this limitation is inherent to all narrative reviews.
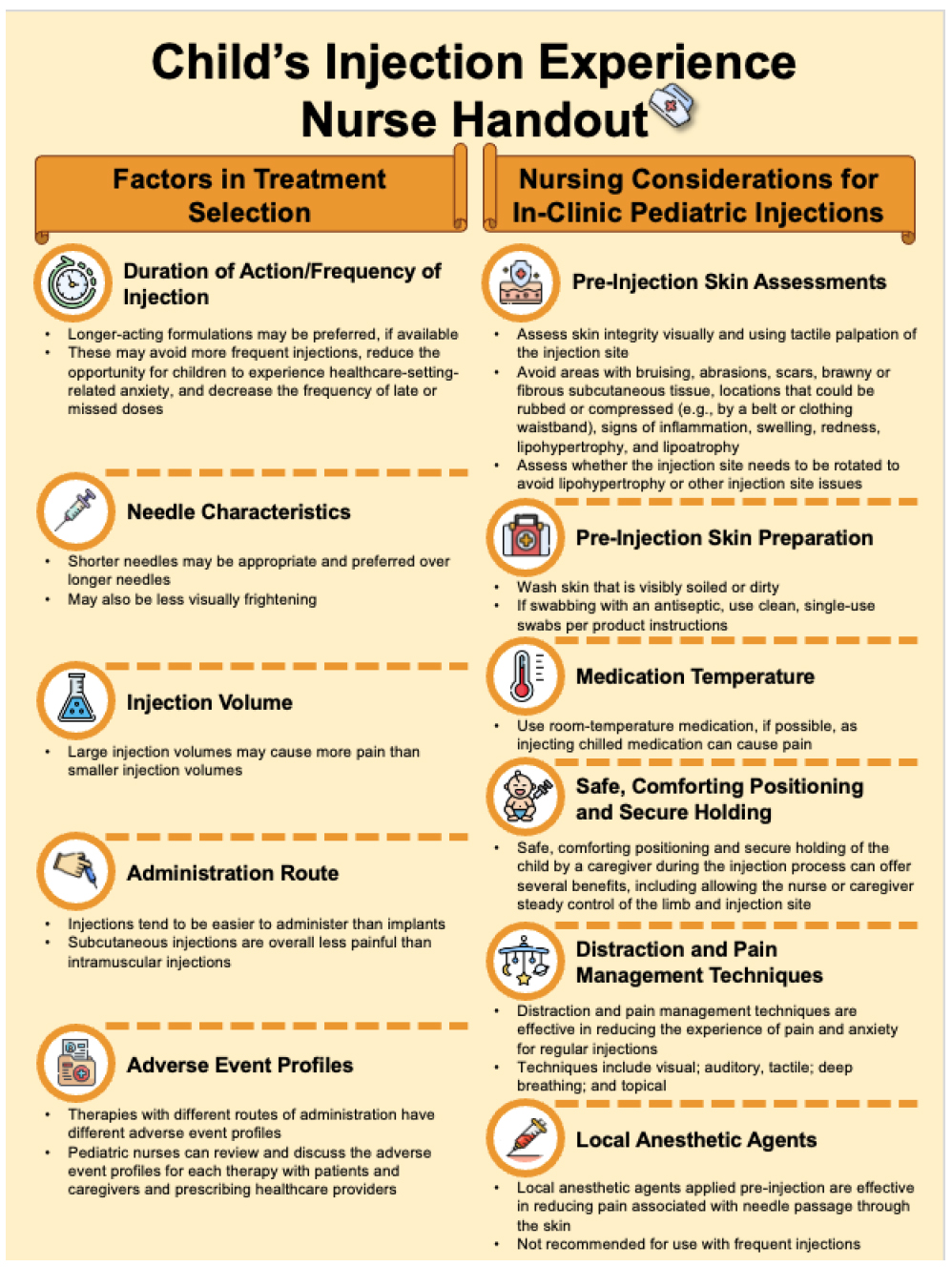
Child’s injection experience nurse handout.
CONCLUSION
Optimal pre-, during, and post-injection techniques, along with proper education and care, can reduce pain and anxiety in children, improve caregivers’ experiences, and prevent treatment delays. Pediatric nurses are encouraged to implement the following recommendations and considerations (Fig. 4) to improve injection experiences for their pediatric patients, caregivers, and healthcare providers:
- Treatment Selection Factors.
- Duration of Action/Frequency of Injection: Longer-acting formulations, if available, may reduce the need for frequent injections, thereby easing anxiety and improving treatment adherence.
- Needle Characteristics: Shorter needles may be appropriate and preferred over longer needles and are also less intimidating.
- Injection Volume: Large injection volumes may cause more pain. However, further research on the impact of injection volumes on children’s treatment experience would be valuable.
- Administration Route: Injections tend to be easier to administer than implants, and SC injections are generally less painful than IM injections.
- Adverse event profiles: Pediatric nurses should be prepared to discuss adverse event profiles for different injection routes with patients, caregivers, and prescribing HCPs.
- Financial Considerations: Nurses should help families explore ways to minimize out-of-pocket expenses to ensure that the child receives optimal treatment.
- Injection Technique.
- Medication Temperature: Use of room-temperature medication reduces pain.
- Safe, Comforting Positioning and Secure Holding: Secure holding can comfort the child and allow for steady control of the limb and injection site.
- Distraction and Pain Management Techniques: Distraction and pain management techniques like visual, auditory, tactile, and breathing exercises effectively reduce pain and anxiety during regular injections.
- Local Anesthetic Agents: Local anesthetics, pre-injection, can reduce pain but have drawbacks.
This review aims to inform best practices for pediatric endocrine nurses treating children with chronic endocrine conditions requiring injections. Nurses should enhance children’s and caregivers’ experiences by educating them on treatment options and applying evidence-based approaches to reduce pain and anxiety. A patient-centered approach incorporating up-to-date practices regarding key factors that improve the injection experience for children and their caregivers is essential for optimal care.
AUTHORS’ CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CCLS | = Certified Child Life Specialists |
| CPP | = Central Precocious Puberty |
| HCP | = Healthcare Provider |
| IM | = Intramuscular |
| LA | = Leuprolide Acetate |
| SC | = Subcutaneous |
ACKNOWLEDGEMENTS
Editorial support was provided by Xelay Acumen Group, Inc. (funded by Tolmar, Inc.).


