All published articles of this journal are available on ScienceDirect.
Challenges of Clinical Decision-making in Emergency Nursing: An Integrative Review
Abstract
Background
The Emergency department (ED) is a complex environment where nurses must make critical decisions under time pressure. This dynamic environment requires advanced clinical decision-making skills to ensure patient safety and positive outcomes.
Objective
The objective of this study is to investigate the challenges faced by emergency nurses in decision-making processes in the emergency department.
Methods
This integrative review study was conducted based on Broome’s method in three stages: the search process, critical appraisal of research, and analysis and synthesis. A search was performed for relevant studies in seven electronic databases (IranMedex, Scientific Information Database (SID), MagIran, Science Direct, PubMed, Google Scholar, and ProQuest) and it was limited to papers published in English and Persian after 2005.
Results
This integrative review identified several key challenges in clinical decision-making for emergency nurses. These include significant time constraints, ambiguous clinical scenarios, insufficient patient history, and limited access to diagnostic tools. Inexperience among newly qualified nurses, emotional stress, and poor communication further complicate decision-making. Resource limitations, ethical dilemmas, cultural diversity, and legal concerns also affect the process. These findings highlight the need for targeted interventions to support emergency nurses and improve patient care.
Conclusion
This review highlights critical challenges in clinical decision-making for emergency nurses, including time and resource constraints. Enhancing decision-making skills through targeted interventions and support systems is essential for improving patient care and outcomes in ED. Future research should focus on effective strategies to address these issues.
1. INTRODUCTION
The emergency department (ED) is a complex environment characterized by a wide range of patient presentations, ranging from true emergencies to non-urgent cases. This variability requires adaptive strategies for triage and care, as healthcare providers must effectively manage acute situations, chronic conditions, and the challenges of overcrowding [1]. Emergency department nurses work in a high-speed and unpredictable environment setting, frequently required to make crucial decisions under tight time pressures [2]. This environment requires the cultivation of advanced clinical decision-making (CDM) abilities, enabling nurses to swiftly evaluate patient needs, integrate information, and carry out suitable interventions [3].
The dynamic and nature of the ED, with its wide range of patient cases and ever-changing conditions, requires nurses to excel in information analysis, decision-making, and effective implementation within a multidisciplinary team [4]. Mastering clinical decision-making skills is essential for enhancing patient safety and achieving positive outcomes in acute care settings [5]. In the rapidly changing healthcare environment, the role of ED nurse is crucial [6]. These professionals must skillfully manage the complexity of patient care, quickly adapt to evolving needs, and make informed decisions based on best practices. Acute care nursing is a demanding field that requires nurses to navigate high levels of cognitive complexity [7]. They must juggle numerous, often conflicting factors to ensure the best possible care for patients and their families [8]. This challenging task is made even more difficult by the typical workload in acute care settings [9], where nurses may be responsible for five or more patients at once.
CDM by expert nurses is a multifaceted process, deeply rooted in dynamic contexts and enriched by a diverse knowledge base and extensive experience [10]. Factors such as patient characteristics, the nurse's expertise, prior experience, personal biases, and available decision support tools influence nurses' decision-making [11]. The dynamic and unpredictable nature of the ED nursing environment, coupled with the often uncertain and fluctuating conditions of patients, demands a high level of decision-making competency from nurses [12]. Given the critical role of CDM in emergency nursing, it is essential to explore the challenges faced by ED nurses in this context [13-15].
This study aims to provide a comprehensive, integrative review of these challenges, highlighting the factors that influence decision-making processes. By identifying and understanding these challenges, the study aims to inform strategies to improve decision-making skills and ultimately improve patient care and outcomes in the ED. The results of this review will contribute to the development of targeted educational programs and support systems that can better equip emergency nurses to manage the complexities of their work environment. In addition, this research will highlight the importance of continuing professional development and the need for robust decision-support tools to assist nurses in making timely and accurate clinical decisions.
2. MATERIALS AND METHODS
To comprehensively explore and understand the challenges of CDM in emergency nursing, we conducted this integrated review study based on Broome’s method [16] in three stages of the search process, critical evaluation of the research, and analysis and synthesis.
2.1. Search Strategy
At this stage, we searched for relevant studies in seven electronic databases, including IranMedex, SID, MagIran, Science Direct, PubMed, Google Scholar, and ProQuest. Our search was restricted to papers published in English and Persian languages after 2005. Studies were included and considered eligible if they were associated with problems related to nurses’ decision-making in the ED, were original or review articles, and were available in full text. Studies that focused solely on a particular aspect of decision-making, such as the difference between clinical judgment and problem-solving, were excluded. Search terms were defined based on the research question and inclusion criteria. We used a combination of keywords and Boolean operators to retrieve relevant studies from the database. Primary keywords included “clinical decision-making,” “emergency nursing,” and “challenges”. In addition, we used truncation () and wildcard (?) symbols to expand our search results, searching for “nurs” to encompass “nurse,” “nurses,” and “nursing,” and “decisio?” to capture “decision” and “decisions.” Filters such as publication year, language, and article type were applied to narrow the search results. This search strategy yielded a total of 53 published articles.
2.2. Critical Evaluation of the Research
In this phase, we implemented a systematic screening process to apply our inclusion criteria to the retrieved studies. Initially, we excluded 1 duplicate article. Next, we reviewed the abstracts of 52 articles and discarded 26 articles that did not meet our specified criteria (Fig. 1). This abstract review focused on identifying studies that focused specifically on the dynamics of clinical decision-making in emergency nursing, as opposed to broader topics unrelated to our topic. Third, we evaluated the full text of the remaining 26 articles (n=26) and ultimately included 26 articles with accessible full text in our analysis (Table 1). Finally, we assessed the methodological quality of the included studies using established quality appraisal tools tailored for empirical and theoretical sources to ensure the robustness of the conclusions of our integrative review.
2.3. Analysis and Synthesis
In this step, the data collected from the studies included authors’ names, year, purpose, basic concepts, study methodology (study design, data collection, and analysis), the study sample, the response rate, and also the validity and reliability of the study. The data were regularly collected in data files and used as raw data. The validity of the analyses was confirmed by the agreement of all the researchers.
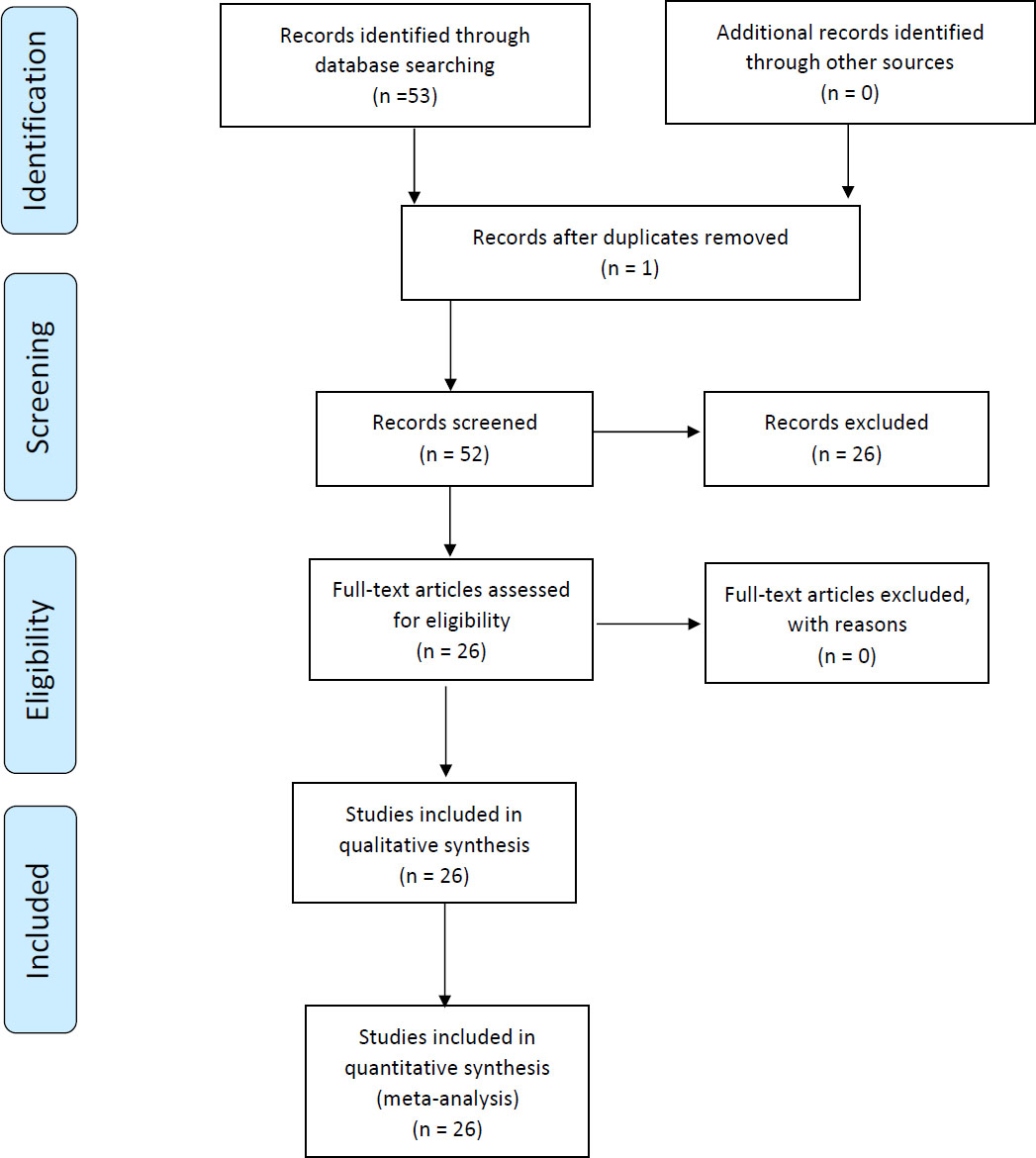
PRISMA flowchart for selection of studies retrieved from databases.
| References | Article | Tool | Objective | Language | Methodology |
|---|---|---|---|---|---|
| [17] | The factors influencing nurses’ clinical decision-making in emergency department | Semi-structured interviews | To identify key factors affecting clinical decision-making among emergency department nurses. | English | Qualitative descriptive study |
| [20] | What if it were me? A qualitative exploratory study of emergency nurses’ clinical decision making related to obstetrical emergencies in the context of a post-roe environment | Focus groups | To explore emergency nurses' decision-making processes in obstetrical emergencies after the Roe decision. | English | Qualitative exploratory study |
| [36] | Foley or not to foley: Emergency nurses' perceptions of clinical decision making in the use of urinary catheters in the emergency department | Surveys | To assess nurses' perceptions and guidelines regarding urinary catheter use. | English | Cross-sectional survey |
| [25] | Factors affecting the process of clinical decision-making in pediatric pain management by emergency department nurses | Interviews | To examine challenges faced by nurses in managing pediatric pain in the emergency department. | English | Qualitative study |
| [29] | Frailty means falling between the cracks: A qualitative study exploring emergency nurses’ understanding of frailty and its use in informing clinical decision-making related to acuity, care, and disposition | Focus groups | To analyze nurses' understanding of frailty and its implications for patient care decisions. | English | Qualitative thematic analysis |
| [18] | Clinical decision making in basic emergency obstetric and newborn care among nurses and midwives: The role of the safe delivery mhealth application - pre-post-intervention study (research protocol) | Mobile health application | To evaluate the effectiveness of an mHealth application in guiding clinical decision-making. | English | Pre-post intervention study |
| [33] | Clinical decision making of greek nurses working in health centers, emergency rooms, medical-surgical clinics, and ICUs | Survey instruments | To investigate decision-making practices across various healthcare settings. | English | Quantitative cross-sectional study |
| [43] | Facilitators of uncertainty in decision-making in Iranian nurses: A qualitative study | Qualitative interviews and thematic analysis | To explore the facilitators of uncertainty in decision-making among Iranian nurses | English | Qualitative study |
| [28] | The relationship between critical thinking and clinical decision-making in emergency nurses of hospitals affiliated with zanjan university of medical sciences in 2020 | Critical thinking assessment tool | To explore how critical thinking influences decision-making in emergency nursing. | English | Correlational study |
| [26] | Is high-fidelity simulation-based training in emergency nursing effective in enhancing clinical decision-making skills? A mixed methods study | High-fidelity simulation-based training (HFSBT) | Evaluate the effectiveness of HFSBT in improving clinical decision-making skills among emergency nurses | English |
Mixed methods. Quantitative: Pre/post-test assessments.
Qualitative: Thematic analysis of interviews |
| [31] | The comparison of role conflict among registered nurses and registered practical nurses working in acute care hospitals in Ontario, Canada | Role conflict scale | To analyze role conflicts experienced by different nursing designations in acute care settings. | English | Quantitative survey analysis |
| [5] | Effective clinical decision-making and action for patient safety in acute care settings | Review of literature | To explore challenges in nurses' clinical decision-making in acute care and propose strategies to enhance patient safety outcomes | English | Literature review |
| [24] | Clinical decision-making process in the pre-hospital emergency nurses: A qualitative study | Semi-structured interviews | To understand the decision-making process of pre-hospital emergency nurses. | English | Qualitative study |
| [34] | Delivery of mHealth application and clinical decision making among nurses and midwives on basic emergency obstetric and newborn care in district hospitals | Mobile health application | To evaluate the impact of mHealth applications on clinical decision-making in obstetric care. | English | Mixed-methods intervention study |
| [21] | An integrative literature review on clinical decision-making of novice nurses for disaster management in the emergency room | Review of literature | To identify factors influencing novice nurses' decision-making in disaster situations. | English | Integrative literature review |
| [1] | Strategies to measure and improve emergency department performance: a review. | Review of literature | Review existing strategies to measure and enhance emergency department (ED) performance | English | Literature review |
| [37] | Ethical, legal and professional accountability in emergency nursing practice: An ethnographic observational study | Observational protocols | To explore ethical and legal accountability issues in emergency nursing. | English | Ethnographic qualitative study |
| [32] | Peripheral intravenous cannulation decision-making in emergency settings: A qualitative descriptive Study | Semi-structured interviews | To investigate decision-making processes in peripheral intravenous cannulation. | English | Descriptive qualitative study |
| [39] | Practice and reflection on the management mode of pain quality control in emergency pre-check and triage | Quality control assessment tools | To assess pain management practices and reflections in triage settings. | English | Qualitative reflective study |
| [38] | Non-clinical intuitions and adaptive heuristics in emergency care: A scoping review | Review of literature | To examine the role of non-clinical intuitions in emergency decision-making. | English | Scoping review |
| [26] | Is high-fidelity simulation-based training in emergency nursing effective in enhancing clinical decision-making skills? A mixed methods study | Simulation training program | To evaluate the efficacy of simulation-based training on decision-making skills. | English | Mixed-methods study |
| [35] | Treatment targets in emergency departments: nurses' views of how they affect clinical practice | Survey instruments | To gather nurses’ perspectives on treatment targets in emergency settings. | English | Cross-sectional survey |
| [19] | Medical decision making in emergency care | Decision-making framework | To explore the factors influencing medical decision-making in emergencies. | English | Qualitative study |
| [23] | An integrated, ethically driven environmental model of clinical decision making in emergency settings | Ethical decision-making model | To propose a model for ethically-driven decision-making in emergency contexts. | English | Conceptual model development |
| [22] | ``Making clinical decisions in emergency situations | Decision-making tool | To investigate the process of making clinical decisions in urgent scenarios. | English | Qualitative exploratory study |
3. RESULTS
This integrative review revealed a complex and dynamic landscape of clinical decision-making in emergency nursing, highlighting both challenges for improving patient care. Several key challenges emerged from the synthesis of the reviewed literature:
3.1. Challenges Related to Time Pressure
Emergency nurses often work in high-stakes environments where critical situations require rapid responses [1]. The urgency of emergency care can lead to significant time constraints, forcing nurses to make quick decisions without careful consideration [17]. This pressure can lead to rushed assessments, increasing the risk of errors or oversights in patient care. Studies have shown that a culture of speed in ED can overshadow the need for careful assessment [18, 19].
3.2. Uncertainty and Complexity
ED clinical scenarios are often characterized by ambiguity and complicated conditions [20]. Nurses must assess patients with incomplete information and may encounter atypical symptoms that complicate the diagnostic process [21]. This uncertainty can lead to apprehension about making decisions, particularly when patients present with overlapping or non-specific symptoms. As such, effective clinical decision-making requires not only knowledge but also the ability to navigate complex medical landscapes [21, 22].
3.3. Lack of Adequate Information
Access to timely and relevant information is crucial for sound CDM [23]. However, emergency nurses sometimes grapple with insufficient patient history, limited clinical guidelines, and inadequate access to diagnostic tools [24, 25]. This lack of information may stem from challenges in data collection or communication breakdowns during handoffs between healthcare providers. Without a clear understanding of a patient's previous health conditions or ongoing treatments, nurses are at a disadvantage in creating effective care plans [23, 24].
3.4. Challenges related to inexperience
Newly qualified nurses or those with limited experience in emergency settings may struggle with clinical decision-making due to a lack of familiarity with the fast-paced environment [22, 26]. Inexperience can lead to hesitation in applying clinical knowledge, assessing patient needs, or making critical decisions under pressure [22, 27]. Training and mentorship are critical to developing the skills necessary for effective decision-making, but not all institutions can provide adequate support for novice nurses [26, 28].
3.5. Emotional and Psychological Stress
The emotional toll of working in emergency settings is significant, as nurses regularly encounter traumatic situations, critically ill patients, and high mortality rates [17]. This continuous exposure to stress can lead to burnout, anxiety, or compassion fatigue, which negatively impacts their mental resilience and decision-making capabilities. The interplay between emotional stress and professional responsibilities can cloud judgment and lead to poorer patient outcomes [17, 29, 30].
3.6. Team Conflicts and Poor Communication
Effective teamwork is essential in emergency care, where multiple healthcare professionals must work together to provide optimal care [31]. However, interpersonal conflicts or differences in communication styles can lead to misunderstandings and misplaced priorities. Poor communication can also cause critical information to be overlooked, further complicating the decision-making process. Building a cohesive team culture is essential to ensure that all members can contribute effectively and advocate for patient needs [24, 32].
3.7. Resource Limitations
Emergency departments sometimes face shortages of essential resources, including medical supplies, staff, and equipment. These limitations can force nurses to make difficult decisions regarding patient prioritization and care delivery [33]. Limited resources may lead to compromised patient safety and affect the overall quality of care, as nurses may need to ration their efforts or adapt care strategies in less-than-ideal circumstances [5, 34-36].
3.8. Challenges Related to Ethical Considerations
Emergency nurses frequently confront ethical dilemmas, particularly when dealing with end-of-life decisions, informed consent, and allocation of scarce resources. Balancing clinical judgment with ethical obligations can be challenging, especially in high-pressure situations where the consequences of decisions are immediate and significant. Ethical tensions can arise from differing values among team members, families, and organizational policies, requiring nurses to navigate complex moral landscapes [20, 37, 38].
3.9. Challenges Related to Cultural and Social Factors
Cultural diversity among patients and within healthcare teams can influence decision-making processes. Nurses may encounter patients from various cultural backgrounds, leading to potential misunderstandings regarding health beliefs, communication styles, and patient preferences. These social dynamics can complicate care and necessitate a deeper understanding of cultural competence to ensure respectful and effective interactions with patients [23, 39].
3.10. Legal and Accountability Issues
The constant threat of legal repercussions looms over clinical decisions in emergency nursing. Concerns about malpractice or liability can cause nurses to hesitate in their decision-making or to over-document procedures and assessments. Navigating these legal waters requires a strong understanding of both ethical practice and legal obligations, adding an additional layer of complexity to already challenging situations [20, 30, 37].
4. DISCUSSION
The results of this integrative review highlight the complex and dynamic nature of CDM in emergency nursing, revealing numerous challenges and opportunities for enhancing patient care. Emergency nurses are often under significant time pressure, which can lead to rushed assessments and increased risk of error. This urgency requires a systematic approach to manage time effectively and ensure patient safety, as emphasized by Bijani et al. (2021) [40]. The implementation of structured protocols and decision-support tools can help mitigate these risks and enable nurses to make more accurate and timely decisions. Additionally, continuous professional development and training in time management and critical thinking are crucial for maintaining high standards of care in such a fast-paced environment.
Clinical scenarios in the ED are often characterized by uncertainty and complexity, requiring nurses to navigate incomplete information and atypical symptoms. Effective decision-making in such contexts necessitates not only clinical expertise but also the capacity to navigate ambiguity and complexity. This aligns with the work of Shabestari et al., who emphasize uncertainty as a pivotal factor in nursing decision-making [41].
Access to timely and relevant information is critical to informed CDM. However, emergency nurses often struggle with insufficient patient history and limited access to diagnostic tools. This challenge is exacerbated by communication breakdowns during handoffs, highlighting the need for improved information systems and protocols to support decision-making, as noted in some other research [42].
Inexperience among newly qualified nurses or those with limited experience in emergency settings can lead to hesitation and uncertainty in CDM. Comprehensive training and mentorship programs are essential to develop the necessary skills for effective decision-making in high-pressure environments, as supported by Shabestari et al. [43].
The emotional toll of working in ED can significantly impact nurses' decision-making capabilities. Continuous exposure to traumatic situations and high mortality rates can lead to burnout and compassion fatigue. Addressing these issues requires organizational support and interventions aimed at promoting mental resilience and well-being among emergency nurses, as discussed in some studies [44, 45].
Effective teamwork and communication are essential in emergency care. Interpersonal conflicts and differences in communication styles can lead to misunderstandings and misaligned priorities, complicating the decision-making process. Building a cohesive team culture and fostering open communication are crucial for ensuring that all team members can effectively contribute to patient care, as highlighted in some research [46].
Emergency nurses frequently encounter ethical dilemmas, especially in high-pressure situations. Balancing clinical judgment with ethical obligations can be challenging, requiring nurses to navigate complex moral landscapes. Ethical decision-making frameworks and support systems are essential to guide nurses through these dilemmas [47].
Cultural diversity among patients and healthcare teams can influence decision-making processes. Understanding and respecting cultural differences are crucial for effective patient interactions and care. Training in cultural competence can help nurses navigate these social dynamics and provide respectful and effective care [48].
In conclusion, improving CDM in emergency nursing requires addressing these multifaceted challenges through comprehensive training, robust support systems, and effective communication strategies. By fostering a culture of continuous learning and resilience, EDs can improve patient outcomes and support the professional growth of their nurses.
4.1. Limitations
This integrative review on clinical decision-making in emergency nursing has limitations. The search was restricted to English and Persian articles, potentially missing relevant research in other languages. Reliance on specific databases may have overlooked some studies, and publication bias is possible. The focus on emergency nursing CDM may have excluded evidence from other fields. There is inherent subjectivity in the integrative review process, although this was mitigated by quality assessment and consensus. Finally, the findings may not be fully generalizable due to differences in healthcare systems and cultural contexts, and further validation in diverse settings is warranted.
CONCLUSION
This review underscores the complex landscape of clinical decision-making in emergency nursing and highlights the multiple challenges faced by practitioners on a daily basis. Effective CDM is significantly hindered by time pressure, which often forces nurses to make rapid judgments under stressful conditions.
This urgency can lead to increased uncertainty, as nurses frequently encounter incomplete patient histories and ambiguous clinical presentations. In addition, the lack of information further complicates the decision-making process, making it imperative for nurses to rely on their intuition and experience rather than comprehensive data.
The emotional demands of the emergency department (ED) environment contribute to cognitive overload, impacting nurses' ability to think critically and make sound decisions. These challenges are further compounded by team dynamics, where miscommunication and lack of collaboration can lead to misunderstandings and patient care errors. Resource limitations, including staffing shortages and inadequate supplies, create additional barriers that hinder effective CDM. Furthermore, ethical considerations surrounding patient care decisions require nurses to navigate complex moral landscapes, emphasizing the need for training in ethical reasoning and culturally competent care.
To improve CDM in emergency nursing, healthcare systems must prioritize comprehensive training programs that focus on developing critical thinking skills and decision-making strategies tailored to high-pressure environments. Implementing robust decision-support tools can help nurses make quick and accurate assessments, ultimately improving patient outcomes. In addition, fostering a supportive work environment that addresses emotional well-being is critical to maintaining nurses ‘performance and resilience. Promoting effective team communication is essential for building cohesive teams that work collaboratively to provide optimal care.
IMPLICATIONS FOR PRACTICE
The results indicate that to enhance clinical decision-making in emergency nursing, healthcare organizations should implement comprehensive training programs that focus on critical thinking and time management under pressure. Strengthening team dynamics through communication training and interdisciplinary collaboration is essential. Integrating clinical decision support tools will provide immediate access to essential information. Addressing emotional fatigue with mental health resources and peer support is critical to building resilience. In addition, training in ethical decision-making and cultural competency is necessary to navigate complex scenarios. Finally, fostering a culture of continuous professional development will empower nurses and improve patient outcomes.
AUTHORS' CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.G.: Contributed to the conceptualization, methodology, formal analysis, original drafting, and supervision; A.D.: Contributed to the methodology, formal analysis, data curation, and the review and editing of the writing; F.J.: Focused on formal analysis, the review and editing of the writing; P.S.: Contributed to both the conceptualization and formal analysis. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ED | = Emergency Department |
| SID | = Scientific Information Database |
| CDM | = Clinical Decision-Making |
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [A.D] upon reasonable request.
ACKNOWLEDGEMENTS
We would like to express our sincere appreciation to the Research Deputy of Tabriz University of Medical Sciences, Iran for their financial support.


