All published articles of this journal are available on ScienceDirect.
Diagnostic Accuracy Comparison between Automatic and Conventional Blood Pressure Measuring Devices in Adults with Hypertension
Abstract
Background
Blood pressure measurement is a main clinical procedure used for the detection of Systemic Arterial Hypertension. Mercury sphygmomanometer, in combination with auscultation technique, is still recognized as the gold standard for non-invasive blood pressure measurement.
Objective
The objective of this study is to compare the diagnostic accuracy between automatic non-invasive blood pressure measurement devices versus mercury sphygmomanometers in hospitalized patients.
Methods
A prospective, analytical and cross-sectional diagnostic method study was designed to compare the concordance, positive and negative predictive value, the sensitivity and specificity of automatic non-invasive blood pressure measurement devices and the mercury sphygmomanometer. The devices were divided into two groups: the reference standard which was mercury sphygmomanometer (n=150), versus the index tests, that were wrist device (n=150), semi-automatic sphygmomanometer (n=150) and vital signs monitor (n=150).
Results
The monitor detected more cases (69%) of systemic arterial hypertension (p 0.0019, OR 5.3). The semiautomatic sphygmomanometer identified more true positives (n=22) and true negatives (n=113). It also showed a higher diagnostic accuracy: 67% sensitivity (p 0.0576, OR 0.5) and 97% specificity (p 0.088, OR 3.2). A mean arterial pressure variation <5mmHg of 65% was found with the semiautomatic sphygmomanometer (p <0.0001, OR 0.02) and 61% with the vital signs monitor (p <0.0001, OR 0.12). Best concordance of blood pressure between reference standard versus index test was obtained in the following order: Semi-automatic sphygmomanometer, Vital signs monitor, and Wrist device.
Conclusion
The use of vital signs monitor to measure blood pressure is recommended in all patients, although semiautomatic sphygmomanometer is more sensitive for the detection of systemic arterial hypertension.
1. INTRODUCTION
Blood Pressure (BP) results from the blood on the walls of arterial vessels at the systemic circulation [1]. It depends on cardiac output, arterial elasticity, blood viscosity, and systemic peripheral vascular resistance [2]. The average reference values in adults are 120/80 mmHg for Systolic (SBP) and Diastolic (DBP), respectively [3]. Mean Arterial Pressure (MAP) is the average pressure in the arteries during a cardiac cycle and is calculated using the formula MAP = [(SBP)+(DBPx2)]/3 [4]. The European Society of Cardiology (ESC, 2024) introduced the category of Elevated Blood Pressure, defined as SBP of 120–139 mmHg or DBP of 70–89 mmHg. BP is a basic vital sign in physical examination [5] that provides data to diagnose and treat multiple pathologies [6]. The American Heart Association (AHA, 2017) recommends blood pressure levels below 130/80 mmHg and stresses the importance of timely interventions to prevent cardiovascular compli-cations. Therefore, blood pressure devices must be available in a reliable, simple, accurate and comfortable way for the patient [7].
Non-Invasive Blood Pressure (NIBP) monitoring allows rapid diagnosis of Systemic Arterial Hypertension (SAH) and hypertensive crises in order to provide an appropriate treatment [8, 9]. Incorrect BP measurement leads to errors in interpretation and effective treatment [10]. There are various automatic, non-invasive, simple and easily accessible Blood Pressure Measurement Devices (BPMD) for all health workers [11], such as sphygmomanometers. For correct BP measurement qualified health workers [12] are required, as well as reliable and accurate biomedical equipment [13]. The mercury column sphygmomanometer, in combination with the auscultation technique, is recognized as the traditional method for hypertension screening. Alternatively, there are other BPMDs, such as digital and semiautomatic sphygmomanometers [14]. These instruments can measure BP indirectly since they externally compress the artery and adjacent tissues under the principle that the pressure required to occlude the artery is equal to the pressure inside it [15]. The AHA recommends taking at least two blood pressure measurements one minute apart, using a calibrated and validated device and using the appropriate cuff size.
The World Health Organization currently points out that there are inaccurate and unverified BPMD and recommends that for scientific research, it is necessary to validate technically and clinically automated devices [16]. Despite the fact that there are studies in the literature that compare some BPMDs with the Reference Standard (RS), there is no clear evidence of the degree of diagnostic accuracy they have in relation to the RS. Therefore, we aimed to compare the diagnostic accuracy of automatic non-invasive blood pressure measurement devices versus mercury sphygmomanometers in hospitalized patients.
2. MATERIALS AND METHODS
2.1. Study Design
A diagnostic, prospective, analytical and cross-sectional study was designed, which included the measurement of Non-Invasive blood pressure in patients electively hospitalized in different services at a third-level hospital.
2.2. Participants
During a six-month period of time of our study (October 2023 to March 2024), a total of 150 hospitalized patients were randomly recruited and their BP was measured at random with four different biomedical devices: mercury sphygmomanometer (Mercurial 922, ADC®), wrist de-vice (OMRON®, bp652), semi-automatic sphygmomanometer (Citizen®, CH-308B), and vital signs monitor (Dräger®, Infinity Vista XL). The first three devices were owned by healthcare workers and were used in their daily practice, so it was decided to include them in the study. The validation of the device complied with the general provisions and standards of Medical Device Regulation 2017/745/EU (MDR) and Medical Devices Directive 93/42/EC Evaluation and Testing [17]. Likewise, the hospital's biomedical engineering area reviewed the good condition, operation and validation of the devices. Inclusion criteria were age ≥ 18 years, elective hospitalization, and thoracic extremity without a venous catheter installed, free of splints or bandages, and absence of injuries, fractures or distal neurovascular compromise. Those patients in which BP was measured in the pelvic extremity and by invasive methods were excluded: pregnant women, children and people with chronic kidney disease, with arterial fibrillation and stiffness.
2.3. Test Methods
BP was measured in all patients with four BP devices, which were divided into two groups: the Reference Standard (RS) that was mercury sphygmomanometer, and the Index Tests (IT) that were Wrist device, the Semi-automatic sphygmomanometer and vital signs monitor. For each measuring device, at least two readings were taken at different times to address the intrinsic variability of BP. Subsequently, the average data was calculated in order to obtain a final representative value of each measurement. Therefore, we obtained 150 measurements for each device, which represented a total of 600 SBP, DBP and MAP evaluations.
BP of all patients was measured after five minutes sitting in a quiet environment, and with their arm resting comfortably on a surface at the heart level. Reusable non-invasive blood pressure cuffs were used according to the arm circumference, based on the following measurements: NIBP-S 17-25 cm, NIBP-M 23-33 cm and NIBP-L 31-40 cm. BP measurements were performed in the same arm sequentially, with a time difference of one to two minutes between each of them (according to interval recommendations) [18]. The measurement with the mercury sphygmomanometer was carried out placing a stethoscope, and after inflating and deflating the cuff, the Korotkoff sounds were listened carefully and the SBP and DBP readings were recorded. The setting used to hear the Korotkoff sound was a noise free space. Since measurement with wrist device is dependent on the position of upper extremity, so the wrist was placed at heart level during the measurement. It is important to highlight that BP was measured by three nursing graduates who were experts in measuring NIBP, each of whom used a different device.
Once registered, the mean BP values of all the patients with each of the BPMDs were reviewed, and the pressure variation between IT and RS was obtained. The difference in the variations of MAP and SBP of the IT in relation to the RS was calculated, considering 5 mmHg as the maximum tolerable cut-off point. Values greater than this variation of MAP and SBP were considered as a lack of precision of the IT with respect to the RS. Finally, the sensitivity, specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of each of the BPMDs were calculated. Additionally, these parameters were also studied in the detection of patients with SAH. Analysis of BP was based on the BP ranges stated by the American Heart Association [19]. For patients with SAH, high BP was considered to be SBP ≥130 mmHg and DBP ≥90 mmHg.
2.4. Statistical Analysis
All the NIBP data were recorded in an Excel spreadsheet for analysis with the statistical software SPSS v. 25.0. Descriptive statistics were used to present the socio-demographic and clinical characteristics of the recruited patients. Numerical variables are described as mean ± standard deviation, with minimum and maximum variability ranges. Categorical variables are described as frequency and percentage in relation to the population at risk. Comparison between IT and RS was made by means of a Chi-square test, and the OR was calculated with a 95% confidence interval. Statistical significance was considered with a p-value <0.05. Bland-Altman scatterplot was used to evaluate the concordance values of MAP between the mercury sphygmomanometer and the automated devices. Sensitivity, specificity, PPV, and NPV were calculated using conventional formulas. This study was developed in accordance with the Standards for Reporting of Diagnostic Accuracy Studies (STARD, 2015).
2.5. Ethics Approval and Consent to Participate
All individuals submitted informed consent before inclusion in the study. The protocol was approved by the research committee of the Regional High Specialty Hospital of Ixtapaluca (code NR-086-2023) and, therefore has been carried out in accordance with the ethical standards established in the Declaration of Helsinki.
3. RESULTS
All hospitalized patients included in the study (female: male ratio of 1:1.3) were recruited equally in the Internal Medicine, Orthopedics, Surgery and Oncology services. A quarter of them had SAH. The population studied was young older adults with weight, height, and body mass index within the normal range. Almost a quarter were smokers and practically a third of them were alcoholics (Table 1).
| Variable | n (%) / mean ± SD (min - max) |
|---|---|
| Gender | Male= 65 (43.3%), Female= 85 (56.7%) |
| Age (years) | 47.2 ± 17.1 (18 - 82) |
| Weight (kg) | 65.7 ± 14.8 (32.5-104.7) |
| Size (cm) | 158 ± 8.7 (141-179) |
| BMI | 25.9 ± 5.2 (14-42) |
| Smoking | 34 (22.7%) |
| Alcoholism | 48 (32%) |
| SAH | 39 (26%) |
| Hospitalization service | |
| Oncology | 35 (23.3%) |
| Surgery | 45 (30%) |
| Orthopedics | 25 (16.7%) |
| Internal Medicine | 45 (30%) |
3.1. Comparison of Mean Arterial Pressure in the Study Groups
The Bland-Altman diagram (Fig. 1) represents the comparison of the MAP measurement obtained using the IT versus the RS. The best concordance of MAP between RS versus IT was obtained in the following order: Semi-automatic sphygmomanometer, Vital signs monitor, and Wrist device.
Table 2 shows the comparison of the variation in the MAP measurement with the different IT in relation to RS (mercury sphygmomanometer). We can see that half of the MAP measurements with the wrist device presented a <5mmHg variation compared to the RS. With the semi-automatic sphygmomanometer, the percentage of variation <5mmHg was 65% and with the vital signs monitor was 61%. The last two methods, unlike the wrist device, significantly presented a <5mmHg variation in the MAP measurement that was greater than this value in relation to RS, particularly in the vital signs monitor (p <0.0001, OR 0.12), compared with the semi-automatic sphygmomanometer (p <0.0001, OR 0.02).
3.2. Study of Systolic Arterial Hypertension with Different Measurement Methods
Table 3 shows the comparison of SAH detection with different methods in relation to RS. We can see that a significantly greater number of hypertensive patients was detected with the vital signs monitor (p 0.0019 and OR 5.3) than with the other two IT.
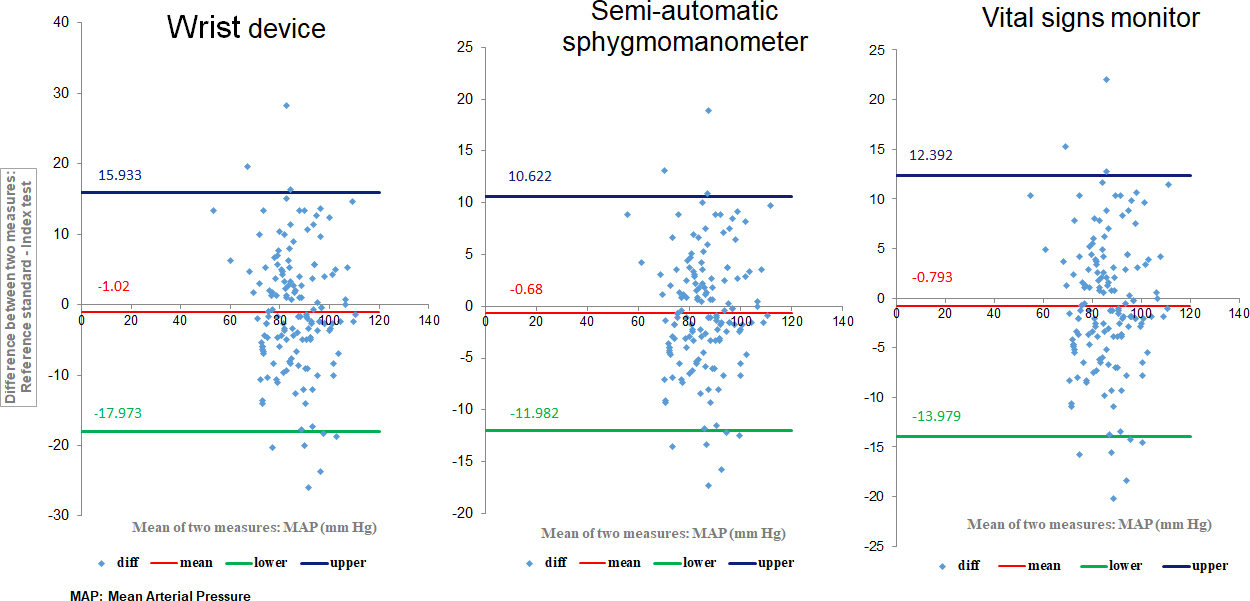
Bland-Altman Scatter plots for concordance of MAP between mercury sphygmomanometer and automated devices.
| Index Tests | MAP ≥ 5 mmHg | MAP < 5 mmHg | p | OR (95% CI) |
|---|---|---|---|---|
| Wrist device | 75 (50%) | 75 (50%) | 1.0000 | 1.0 (0.5 - 1.9) |
| Semiautomatic BP device | 52 (34.6%) | 98 (65.4%) | <0.0001 | 0.02 (0.005 – 0.094) |
| Vital signs monitor | 58 (38.7%) | 92 (61.3%) | <0.0001 | 0.12 (0.05 – 0.27) |
| Index Tests | SBP ≥ 130mmHg | p | OR (95% CI) | |
|---|---|---|---|---|
| Yeah | No | |||
| Wrist device | 16 (48.5%) | 17 (51.5%) | 0.8056 | 0.8 (0.3 – 2.3) |
| Semi-automatic sphygmomanometer | 19 (57.6%) | 14 (42.4%) | 0.2201 | 1.8 (0.6 – 4.8) |
| Vital signs monitor | 23 (69.7%) | 10 (30.3%) | 0.0019 | 5.3 (1.8 – 15.1) |
Fagan’s nomogram for the detection of systolic arterial hypertension with the three index tests in relation to the reference standard.
| Sensitivity | Specificity | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Device | Mercury Sphygmomanometer | Test Index | p | OR | Mercury Sphygmomanometer | Test Index | p | OR | |
| Wrist device | 79% | 67% | 0.0576 | 0.5 (0.3 – 1) | 91% | 92% | 0.7999 | 1.1 (0.4 – 3.1) | |
| Semiautomatic BP device | 79% | 67% | 0.0576 | 0.5 (0.3 – 1) | 91% | 97% | 0.0885 | 3.2 (0.8 – 12.2) | |
| Vital signs monitor | 79% | 61% | 0.0061 | 0.4 (0.2 – 0.8) | 91% | 93% | 0.6030 | 1.3 (0.5 – 3.7) | |
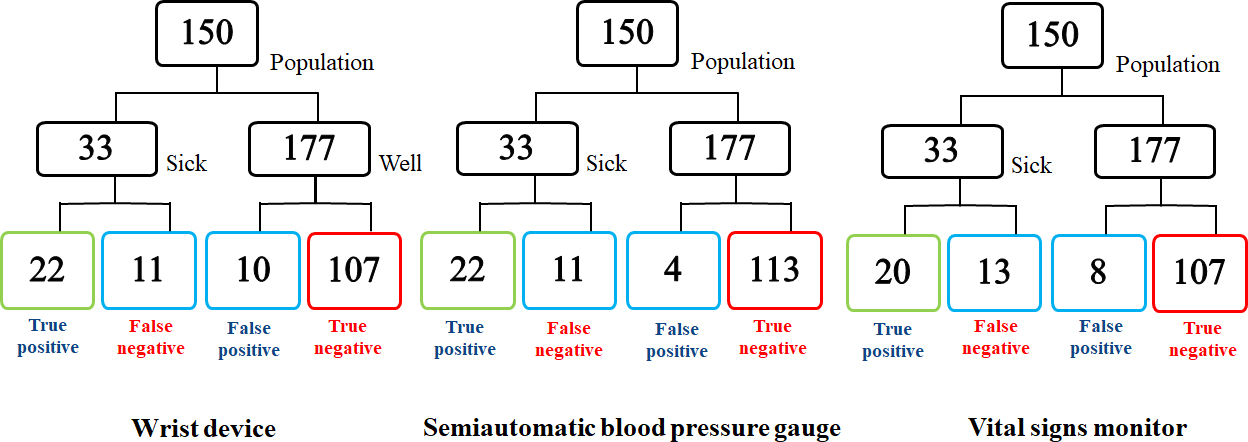
Fig. (2) shows the Fagan Nomogram for the diagnosis of SAH, which was performed with the three IT used and compared with RS. For each test, the prevalence, sensitivity and specificity of the SAH was obtained. We can see that a relatively higher number of true positive cases of SAH (n=22) and true negatives (n=113) was detected with the semiautomatic sphygmomanometer than with the other two IT.
3.3. Comparison of the Index Tests with the Reference Standard for Arterial Hypertension
Table 4 compares the sensitivity and specificity published in the literature for the diagnosis of SAH with the three IT in relation to RS. The wrist device and the semi-automatic device show practically no significant variations in sensitivity compared to the RS, while the sensitivity of the vital signs monitor is significantly lower. Regarding specificity, none of the three IT presented significant variations when compared to RS.
4. DISCUSSION
4.1. Major Findings
Because BP measurement in clinical practice is relevant to detect hypertensive patients, different instruments have been developed to measure this basic vital sign. However, reliable equipment is required in terms of sensitivity and specificity in order to discard false positive and false negative cases. The use of a validated sphygmomanometer is necessary to measure BP, as it must be able to allow reproducible and accurate measurements. In this study, we evaluated the diagnostic accuracy of three digital devices to measure BP and compared the variation of the equipment with respect to the mercury sphygmomanometer, used as the traditional method for SAH screening test. It should be noted that the devices have advantages and disadvantages of use. Incorrect BP measurement can lead to poor control and increased risk of cardiovascular mortality [20]. In this study, Bland-Altman Scatter plots showed a better concordance between mercury sphygmomanometer and Semi-automatic sphygmomanometer, followed by Vital signs monitor. The lowest concordance was obtained with the Wrist device.
4.2. Understanding Study Findings
Mercury sphygmomanometer, considered as the RS to measure BP, identifies hypertension and hypotension. However, we only emphasized SAH, for it is a public health problem in order to detect it and provide rapid treatment in critical cases. BP monitoring equipment has been shown to be part of the treatment of hypertension despite its heterogeneity [21]. It should be noted that some commercially available BPMDs have not been independently evaluated using a valid protocol [18]. Mercury sphygmomanometer is cost-effective, does not require electricity or batteries, but needs constant calibrations and there is a risk of noise interference [22]. However, it has been gradually discontinued by WHO (2020), because mercury has actually been considered as a risk factor for environmental pollution [16]. It also needs the ability to reduce evaluator's bias and requires more time and effort from health workers. Mercury sphygmomanometer has a moderate level of accuracy and identifies hypertension with a 79% sensitivity and a 91% specificity [23]. WHO recommends evaluating the hearing capacity and the accuracy of the measurements of professionals on a regular basis since deficiencies in vision, hearing or manual dexterity are factors that contribute to inaccurate BP measurements when using the mercury sphygmomanometer [16].
4.3. Results in Comparison with Other Studies
A wrist device that automatically inflates and deflates is easy to use, fast, and records multiple BP readings [24]. The disadvantages of this device are that the pressure results are sometimes inaccurate since it has lower precision compared to aneroid and mercury sphygmomanometer. In case of hypotension it can mark “Error” or give erroneous readings [25]. The WHO describes that wrist devices are not appropriate for clinical use, since their accuracy has not been validated [16]. However, device validation studies are very important, as some wrist devices have already been validated by the international scientific organization STRIDE BP and the International Society of Hypertension [26]. In this study, it was found that half of the MAP evaluations with the wrist device presented a variation of less than 5mmHg compared to the RS, while no significant variations were observed in terms of sensitivity.
Semiautomatic sphygmomanometer includes a bulb to inflate the cuff, with deflation and automatic determination of BP [3]. It senses arterial flow in which pulses received through the cuff are filtered, amplified, processed, and applied to an algorithm to estimate systole and diastole values [22]. It is easy to use and suitable for screening, saves clinical time and resources, and needs less expertise and training when used in lack of an experienced health worker [27]. The disadvantage of this device is its high cost and the constant requirement for battery replacement [28]. The hybrid sphygmomanometer is a device that can be used in replacement of a mercury sphygmomanometer [29]. Our results suggest that the semiautomatic sphygmomanometer detected a relatively higher number of true positive (n=22) and true negatives (n=13) SAH cases, compared with the other two index tests. In the diagnosis of SAH, the semiautomatic method practically did not present significant variations in terms of sensitivity compared to the RS.
The vital signs monitor displays vital signs graphically, including invasive and non-invasive BP [30]. It is the most frequently used device in intensive care units since it measures BP automatically at scheduled times. The disadvantage is that the results can be affected by external factors, such as patient movement, electromagnetic interference, and incorrect use of the device [31]. The monitor has a moderate level of accuracy and identifies SAH with similar sensitivity and specificity to RS. Using inaccurate BPMD can lead to overdiagnosis and unnecessary treatment or underdiagnosis and exposure to preventable cardiovascular disease [18]. Therefore, it should be considered that the monitor that has been favorably validated in adults may not be accurate in children, pregnant or patients with arm circumference >42 cm. Our results showed a moderate level of precision when comparing the variation of the MAP less than 5mmHg, and it was 65% for the semiautomatic sphygmomanometer and 61% for the vital signs monitor, which presented a significant variation with respect to the RS but not with the wrist device (50%). In this study, a significantly higher number of patients with SAH were detected with the vital signs monitor than with the other index tests. It was identified that the monitor was closer to the reference standard in the measurement of SBP and MAP. In contrast, its application for the detection of arterial hypertension presented significantly lower sensitivity.
4.4. Clinical Implications
BP measurement is essential for the prevention of cardiovascular risk and the control of high BP; for this, there are various BP measurement devices, so a reliable sphygmomanometer is required in terms of sensitivity and specificity, which provides security in clinical results.
4.5. Strengths and Limitations of the Present Study
Measurements of BP values were only obtained in stable patients and not in critically ill ones, despite the reduced sample, considering that our evaluation was carried out in all hospitalized patients. Therefore, the results, although showed a clear tendency, cannot be widely generalized to all hospitalized populations, for a major cohort of patients is highly recommended in order to validate our findings [32].
CONCLUSION
The accuracy of BPMDs is essential for a quality and safely healthcare. Therefore, the use of the vital signs monitor is recommended to measure NIBP in all patients, although the semi-automatic sphygmomanometer presented greater sensitivity in detecting SAH. The wrist device was useful for diagnosing hypotension, however, lower accuracy was obtained, so its accuracy needs to be validated before its use in clinical practice. Digital BP sphygmomanometer can be used to identify hypertension due to their specificity and moderate sensitivity in diagnosing true positive cases. Mercury sphygmomano-meter is gradually disappearing from clinical practice, although it is currently the reference standard until an alternative standard is established.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| BP | = Blood Pressure |
| BPMD | = Blood Pressure Measurement Devices |
| DBP | = Diastolic Blood Pressure |
| IT | = Index Test |
| MAP | = Mean Arterial Pressure |
| NIBP | = Non-Invasive Blood Pressure |
| NPV | = Negative Predictive Value |
| PPV | = Positive Predictive Value |
| RS | = Reference Standard |
| SAH | = Systemic Arterial Hypertension |
| SBP | = Systolic Blood Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Institutional Review Board (or Ethics Committee) of Regional High Specialty Hospital of Ixtapaluca, dependent on the Health Services of the Mexican Social Security Institute for Welfare, Mexico (code NR-086-2023) dated September 20, 2023.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All subjects gave their informed consent before being included in the study. The information was used for statistical research purposes and was handled confidentially, respecting the rights of the patients.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article are available upon request from the corresponding author [N.S-G].
ACKNOWLEDGEMENTS
Declared none.


