All published articles of this journal are available on ScienceDirect.
Impact of a Modified Discharge Program on Health-related Quality of Life Following Coronary Artery Bypass Grafting: A Randomized Controlled Trial
Abstract
Introduction
The patients of post-operative coronary artery bypass graft (CABG) often face complications impacting their health-related quality of life (HRQOL). Effective discharge planning can facilitate recovery and improve HRQOL. Therefore, the aim of this study was to evaluate the impact of a modified re-engineered discharge program on the HRQOL in patients 30 days after Coronary Artery Bypass Graft surgery.
Methods
A posttest-only randomized clinical trial with 104 CABG patients compared a modified project Re-Engineered Discharge (RED) program to standard procedures. The intervention group received specialized training, while the control group followed routine care. HRQOL was assessed 30 days post-discharge using the SF-36 scale. Chi-square and independent t-tests were used to perform statistical tests.
Results
Of 104 participants, 55 in the intervention and 49 in the control group completed the study. No statistically significant differences were found in overall HRQOL scores (M (SD) =49.93 (14.00) vs. M (SD) 47 (11.85) P =.272) or in subscales, such as physical functioning (P=.818), emotional health (P=.155), and pain (P=.839). Minor, non-significant subscale improvements were noted in the intervention group. Routine care and pain may have impacted program effectiveness.
Conclusion
The study emphasizes the complexities of embedding structured discharge programs within standard care, offering valuable insights into limitations in post-operative cardiac care.
1. INTRODUCTION
In the first month post-CABG, patients commonly experience pain, sleep disturbances, dyspnea, anxiety, depression, gastrointestinal issues, dizziness, palpitations, appetite loss, and leg/foot swelling. Fatigue resulting from these symptoms hinders their ability to perform daily activities [1]. Additionally, lifestyle changes can increase irritability, anger, and anxiety, but discharge training and counseling can improve outcomes [2]. Furthermore, CABG patients with discharge planning and counseling showed faster recovery and improved quality of life [3]. Two studies showed significant quality-of-life improvements in CABG patients after in-hospital training and follow-up counseling [4, 5]. Insufficient knowledge at the time of discharge among Jordanian CABG patients has been identified as a risk factor that hinders self-care activities due to unmet educational needs [6]. Studies by Mosleh, Eshah [7], and Subeh and Salami [8] have highlighted this issue. Subeh and his colleague noted that the absence of structured discharge planning programs in two Jordanian hospitals led to patients reporting a lack of knowledge regarding complications management, self-care activities, medication issues, and diet [9]. Thorough discharge information and follow-up were shown to improve the postoperative management and HRQOL of patients, reducing failures and readmissions [10-12], reducing mortality, morbidity, and complications [13], and improving patient outcomes [14-16]. Project RED aims to reduce hospital readmissions through a series of structured steps led by a discharge advocate nurse [17]. Project RED has been studied for its effects on post-discharge outcomes, including hospital use, mortality, follow-up, patient preparedness, morbidity, patient experience, family involvement, and cost-saving. However, its impact on health-related quality of life remains unassessed. Post-CABG discharge planning, supported by a discharge educator, enhances recovery, understanding of care, communication, and follow-up [18-20]. Nurses play a pivotal role in the postoperative care of patients, particularly those recovering from complex surgical procedures, such as coronary artery bypass grafting (CABG) [8]. Their responsibilities encompass a range of critical tasks, including educating patients about self-care practices, monitoring for potential complications, managing pain effectively, and providing emotional and psychological support during the recovery process.
Additionally, nurses ensure adherence to discharge plans by reinforcing instructions on medication regimens, lifestyle modifications, and follow-up care [18-20]. These comprehensive nursing interventions are essential for optimizing recovery, enhancing health-related quality of life, and reducing the risk of readmissions, underscoring the significant impact of nursing care on postoperative outcomes [18-20].Therefore, the purpose of the current study was to investigate the effect of implementing a modified discharge intervention based on the Project RED program on health-related quality of life among CABG patients 30 days after surgery.
2. MATERIALS AND METHODS
2.2. Setting
The study was conducted at the largest specialized center for cardiovascular surgeries in Jordan.
2.3. Participants
The study included Jordanian adults who underwent first-time elective CABG surgery for single to triple CAD, met inclusion criteria (18+, Arabic-speaking, contactable, no history of aortic calcification or stroke, able to consent), and were discharged to home. Exclusion criteria covered mental disorders, combined cardiac procedures, cerebrovascular disease, TIA, significant carotid stenosis (≥70%), emergency CABG, extended postoperative stays over 15 days, and in-hospital mortality.
2.4. Sampling Procedure
Single-center non-probability sampling was used to recruit the study participants. The sampling procedure adopted the block randomization method to select the patients. Blocked randomization could provide approximately equal groups of participants assigned to intervention and control groups [21]. Block of 2,4, or 6 (according to the availability of the patients) was used each day to assign the patients to intervention and control groups. The researcher used the RAND function on an Excel sheet to assign a random number to each patient. Each day, one-half of the CABG patients were assigned to the intervention group and the other half to the control group. The order in which the intervention was assigned in each block was randomized, and this process was repeated for all consecutive blocks of participants (Fig. 1).
2.5. Sample Size
The sample size calculation aimed to achieve sufficient statistical power to detect group differences, thereby minimizing type II errors. Power analysis involved setting an alpha level (typically 0.05), estimating effect size, and determining the desired power (commonly 0.80) to ensure adequate sample size. Effect size estimation often uses pilot studies or previous research in nursing, where medium effect sizes are standard. For this study, sample size estimation employed the Chi-Square test and G*Power software. With an alpha of 0.05, a medium effect size (0.50), and a power of 0.80, 52 subjects per group were required, totaling 104. Anticipating a 30% dropout rate, 67 participants per group (totaling 134) were recruited to ensure adequate completion rates [22] (Fig. 2).
2.6. Instruments
The study used two questionnaires: patient demographic data and the SF-36 questionnaire.
2.6.1. Patient Demographic Data
Researchers developed a demographic questionnaire, collecting patient data via self-report and medical records. Data included gender, age, education, admission date, social and employment status, chronic disease history, post-operative blood units, graft count, hospital and ICU stay, creatinine levels, aortic cross-clamp time, ventilation duration, ejection fraction, and stroke history [23-25].
2.6.2. SF-36 Questionnaire
The SF-36 scale assesses population health, disease burden, clinical outcomes, and treatment effects [26]. It is considered a golden standard for QOL assessment. It includes multi-item scales to measure the following eight dimensions: physical functioning (10 items), role limitations due to physical health problems (4 items), bodily pain (2 items), social functioning (2 items), general mental health (5 items), role limitations due to emotional problems (3 items), vitality, energy and fatigue (4 items), and general health perception (5 items). The eight subscales can be collated into two higher-order domains representing the physical and mental aspects of the QOL, referred to as a physical component summary and a mental component summary [27]. The eight domains can be clustered into two main domains: 'Physical Component Summary (PCS) and 'Mental Component Summary (MCS) [28, 29]. The SF-36 was extensively used and validated among CABG patients [30, 31]. Moreover, the Arabic version of the scale is valid and reliable; Cronbach’s alpha ranged between 0.71- 0.94 [28, 32]. The scores were calculated and transformed to a scale from 0-100, with a mean of 50 and a standard deviation of 10. The higher scores reflected better health [26]. The SF-36 scoring system was for the total score and each dimension separately, with zero being the worst and 100 the best possible score . The lowest scores indicate the lowest health state, which indicated a functional limitation, severe social and role disability, and distress.
2.7. Ethical Consideration
The study received ethical approval from the “Royal Medical Services Human Research Ethics Committee no.5/2020. Researchers informed patients about the objectives of the study, assured voluntary participation, and allowed withdrawal at any time. Oral and written consent was obtained from all participants before the study began.
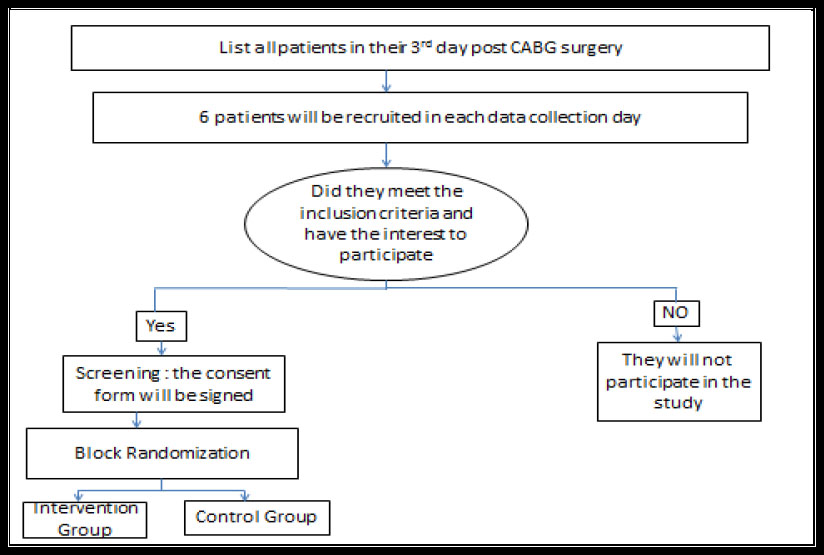
Sampling procedure.
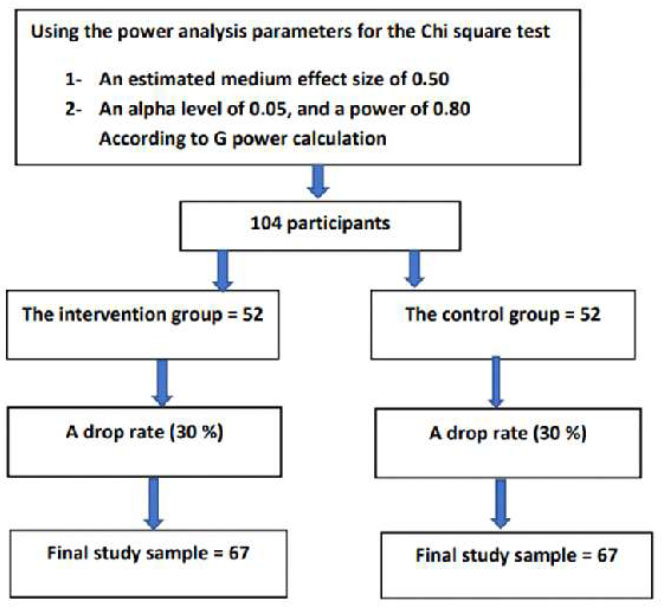
Sample size calculation.
2.8. Data Collection
Data collection occurred from July 15 to October 30, 2020, delayed by COVID-19-related clinic closures and elective surgery postponements in Jordan. A total of 118 eligible CABG patients from QAHI surgical floors were randomized into intervention (n=59) and control (n=59) groups. The intervention group received a modified Project-RED discharge plan, including an After-Hospital Care Plan (AHCP) with educational and medication guidance, plus a follow-up call. The control group received standard discharge care, including a summary, medications, clinic appointments, and verbal instructions. Health-related quality of life (HRQOL) was measured 30 days post-discharge using the SF-36 questionnaire. Researchers obtained IRB approval and informed consent, gathering baseline demographic and medical data pre-discharge (Figs. 3 and 4).
2.9. Intervention
Project RED is a standardized hospital-based program designed to provide patients and caregivers with the information they need to continue care at home (AHRQ, 2013). It has been demonstrated to reduce all-cause readmission (Adams et al., 2014; Berkowitz et al., 2013; Ceppa et al., 2015; Jack et al., 2009; S. E. Mitchell et al., 2016)), reduce all-cause mortality (Ceppa et al., 2015; Patel and Dickerson, 2018), improve patient outcomes (Cancino et al., 2017; Ceppa et al., 2015; Jack et al., 2009), and improve patient safety during care transitions (Ceppa et al., 2015) [12, 13, 16, 17].
Project RED was proposed by a cardiologist at Boston Medical Center (BMC) in 2007 as a mechanism to reduce 30-day readmission (AHRQ, 2013). The team tabulated areas of critical weakness leading to readmission and formulated 12 steps to address these issues.
The proposed intervention in the current study, which is a modified project RED, will be used for the preparation of the patients for hospital discharge. Through the proposed intervention, patients will receive individualized education before discharge, all the medication will be reconciled, and the patients will be educated about it. A written educational booklet (after-hospital care plan [AHCP]) will be handed to the patients, specifying all patient appointments (details given regarding location, date, time, and name of the physician) and all the medication with a color-coded table to facilitate comprehension of the medicines regimen. Moreover, the AHCP will include the frequently experienced signs and symptoms, and the patients will receive a follow-up phone call within 72 hours after discharge.
2.9.1. After Hospital Care Plan
Following ethical approval and randomization, the DE prepared individualized After-Hospital Care Plans (AHCP) for intervention group patients, a core component of Project RED. AHCP preparation involved reviewing patient files, consulting with physicians, and meeting the patient and if needed, the clinical pharmacist. The AHCP ensured
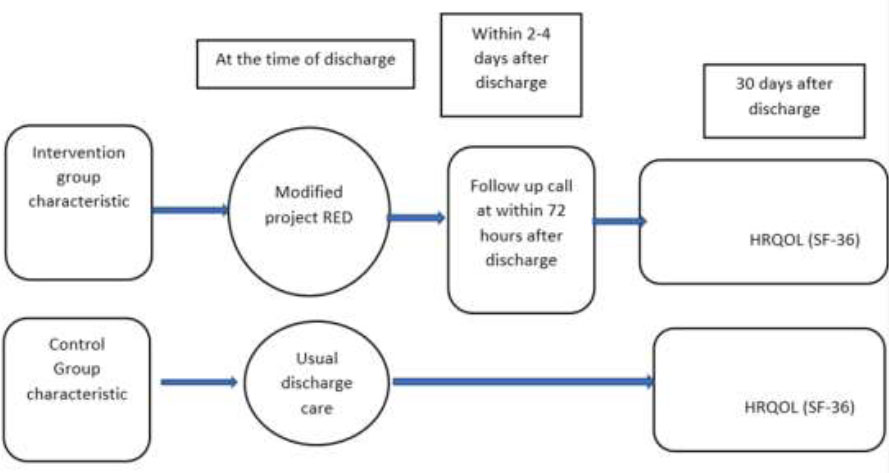
Data collection procedure.
that the patients understood their diagnoses, surgical procedures, comorbidities, and treatment plans and included essential information, such as surgeon and pharmacy contact details, medication allergies, and follow-up call information. This comprehensive, patient-specific AHCP enhanced the understanding of care requirements post-discharge.
2.9.2. Post-discharge Follow-up Phone Call
In the intervention group, CABG patients received a follow-up call from the discharge educator (DE) within 2–4 days post-discharge. During the 20–30-minute call, the DE clarified discharge plans, assessed health status, reviewed medications, confirmed appointment details, and provided guidance on managing potential complications. Health assessments distinguished post-surgery effects from new concerns, with recommendations for non-urgent issues. Medication adherence and understanding were supported, and any non-adherence was addressed through education or consultations. Key information, including health status, medication management, and post-discharge instructions, was documented to aid the transition of patients to home care.
2.10. Analysis Strategy
Data were analyzed using IBM SPSS Statistics version 20, incorporating both descriptive and inferential statistical methods to evaluate the impact of the intervention on outcomes. Descriptive statistics, including frequency distributions, percentages, means, and standard deviations, were used to summarize demographic and clinical characteristics. Baseline characteristics were assessed for group homogeneity using independent t-tests for continuous variables and Chi-square or Fisher’s exact tests for categorical variables, ensuring comparability between groups. Levene’s test was performed to verify homogeneity of variance, with the Mann-Whitney U test applied to non-normally distributed data or where variance assumptions were violated. The primary outcome, Health-Related Quality of Life (HRQOL) as measured by the SF-36, was analyzed to compare total scores and individual subscale scores between groups, employing independent t-tests for normally distributed data and non-parametric tests for distributions deviating from normality. Subscale scores were examined individually to explore specific quality-of-life dimensions impacted by the intervention. Missing data were managed through pairwise deletion to maximize the available dataset for analysis. Statistical significance was set at p < 0.05, and effect sizes were calculated to provide insight into the magnitude of observed differences.
2.10.1. Results
A total of 118 patients were randomized equally into intervention (n=59) and control (n=59) groups, with final samples of 55 and 49, respectively, due to follow-up losses. An independent t-test was used to assess group homogeneity across variables, including age, creatinine levels (pre- and post-operative), aortic cross-clamp time, ICU stay, and hospital stay. Age showed no significant differences between the intervention (M=56.98, SD=8.06) and control (M=56.2, SD=8.937) groups, and clinical variables were similar across both groups. Levene’s test confirmed variance homogeneity, except for mechanical ventilation, where the Mann-Whitney test revealed a significant difference between groups (Table 1).
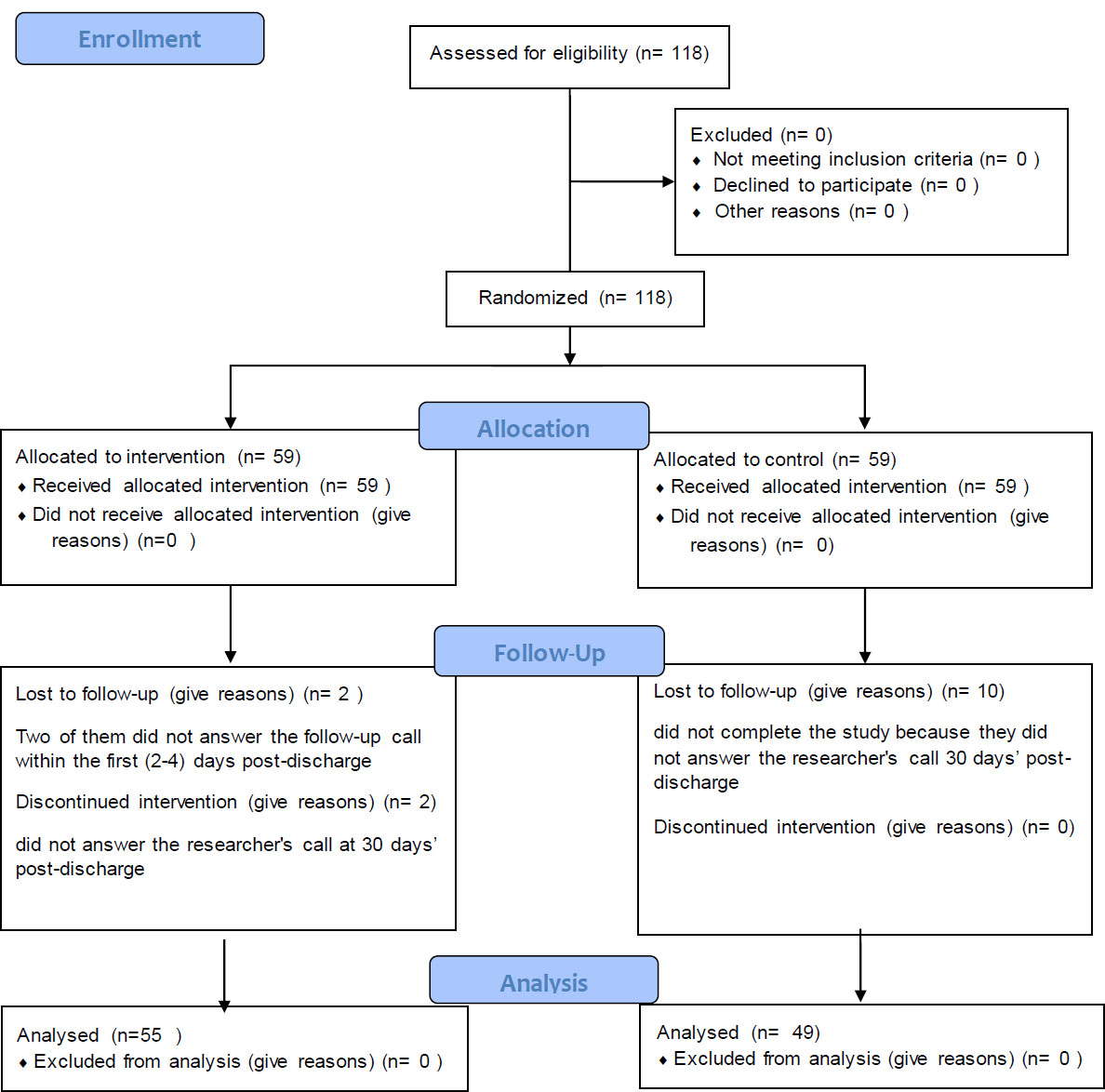
Flow diagram.
| Continuous Variable | Intervention (n=55) | Control (n) =49 | Test Name | p-value | ||
|---|---|---|---|---|---|---|
| - | M (SD) | M (SD) | - | - | ||
| Age | 56.98 (8.066) | 56.2(8.937) | Independent t-test | .642 | ||
| Pre-operative creatinine | .8502(.2823) | .8918(.2264) | .412 | |||
| Post-operative creatinine | .8253(.26316) | .8369(.221614) | .807 | |||
| Aortic cross-clamp time | 56.69(18.885) | 54.39(15.334) | .500 | |||
| ICU length of stay | 2.13(1.292) | 2.24(1.164) | .628 | |||
| Hospital length of stay | 7.67(2.381) | 8.14(2.574) | .336 | |||
| Duration of mechanical ventilation | -2.306 | Mann-Whitney test | .021 | |||
| Categorical Variable | Intervention | Control | - | p-value | ||
| - | Count | % | Count | % | - | - |
| Gender | - | - | - | - | Chi-square test | .787 |
| Male | 46 | 83.6% | 40 | 81.6% | - | - |
| Female | 9 | 16.4% | 9 | 18.4% | - | - |
| Education | - | - | - | - | Chi-square test | .967 |
| Intermediate | 25 | 45.5% | 23 | 46.9% | - | - |
| Secondary | 17 | 30.9% | 14 | 28.6% | - | - |
| Collage/university | 13 | 23.6% | 12 | 24.5% | - | - |
| Social Status | - | Fisher exact test | .167 | |||
| Married | 48 | 87.3% | 47 | 95.9% | - | - |
| Widow | 7 | 12.7% | 2 | 4.1% | - | - |
| Employment status | - | - | - | - | Chi-square test | .879 |
| Employed | 21 | 38.2% | 18 | 38.7% | - | - |
| Not employed/retired | 34 | 61.8% | 31 | 63.3% | - | - |
| Dislipidemia | - | - | - | - | Chi-square test | .991 |
| Yes | 28 | 50.9% | 25 | 51% | - | - |
| No | 27 | 49.1% | 24 | 49% | - | - |
| Diabetes | - | - | - | - | Chi-square test | .862 |
| Yes | 29 | 52.7% | 25 | 51% | - | - |
| No | 26 | 47.3% | 24 | 49% | - | - |
| Hypertension | - | - | - | - | Chi-square test | .844 |
| Yes | 27 | 49.1% | 25 | 51% | - | - |
| No | 28 | 50.9% | 24 | 49% | - | - |
| Ejection fraction | - | - | - | - | Chi-square test | .108 |
| Normal | 25 | 45.5% | 30 | 61.2% | - | - |
| Abnormal | 30 | 54.5% | 19 | 38.8% | - | - |
| Experienced previous strokes | - | - | - | - | Fisher exact test | .341 |
| Yes | 1 | 1.8% | 3 | 6.1% | - | - |
| No | 54 | 98.2% | 46 | 93.9% | - | - |
| Units of blood received post-operatively | 2.281 | Fisher exact test | .905 | |||
| 0 units | 23 | 41.8% | 20 | 40.8% | - | - |
| 1 unit | 23 | 41.8% | 18 | 36.7% | - | - |
| 2 units | 4 | 7.3% | 6 | 12.2% | - | - |
| 3 units | 3 | 5.5% | 4 | 8.2% | - | - |
| 4 units | 1 | 1.8% | 0 | 0% | - | - |
| 5 units | 1 | 1.8% | 1 | 2% | - | - |
| Number of Grafts | 3.172 | Fisher exact test | .579 | |||
| 1 graft | 1 | 1.8% | 0 | 0% | - | - |
| 2 grafts | 7 | 12.7% | 8 | 16.3% | - | - |
| 3 grafts | 22 | 40% | 23 | 46.9% | - | - |
| 4 grafts | 25 | 45.5% | 17 | 34.7% | - | - |
| 5 grafts | 0 | 0% | 1 | 2% | - | - |
The Chi-square test was used to compare categorical variables (gender, education, employment status, dyslipidemia, diabetes, hypertension, and ejection fraction) between intervention and control groups, with all assumptions met. For variables with expected cell frequencies under five (social status, previous strokes, graft count, and blood units received), the Fisher exact test was applied. Results indicated no significant differences between groups across all categorical variables. Additionally, all patients underwent on-pump CABG. A comparison of study groups is detailed in Table 1.
An independent t-test assessed mean differences in the total SF36 score and subscales between groups. Preliminary screening confirmed approximate normality, and Levene's test validated homogeneity of variance. No significant differences emerged in HRQOL total mean scores between intervention (M=49.93, SD=14.00) and control groups (M=47, SD=11.85), (t=-1.10, p=.27), indicating similar quality of life levels across both groups. The details are provided in Table 2.
A comparison of HRQOL subscale scores between intervention and control groups included physical functioning, physical health limitations, emotional health limitations, energy/fatigue, emotional well-being, social functioning, pain, and general health. Preliminary screening confirmed approximate normality, except for physical function limitations and general health subscales, which were analyzed using the Mann-Whitney test. Levene’s test validated homogeneity of variance for most subscales, allowing pooled variance t-tests, while a separate t-test version was applied for variables violating this assumption. Results indicated no significant differences in subscale means between groups, though the intervention group had slightly higher scores on two subscales (Table 2).
| Quality of Life | Intervention (55) | Control (49) | Skewness | T | p-value *** | |
|---|---|---|---|---|---|---|
| - | M (SD) | M (SD) | - | - | - | |
| Total quality of life | 49.93(14.007) | 47(11.856) | 0.050 | -1.104 | .272 | |
| QOL Subscales | ||||||
| Physical functioning | 38 (18.871) | 37(19.012) | .199 | -.230 | .818 | |
| Limitations due to physical health | 4.55(18.060) | 2.04(8.595) | 4.984 | 1328* (-.285) ** |
.776 | |
| Limitations due to emotional health | 63.64(46.380) | 50.34(48.171) | -.295 | -1.433 | .155 | |
| Energy/fatigue | 56.82(18.963) | 54.39(17.429) | -.471 | -.678 | .500 | |
| Emotional wellbeing | 62.76(20.481) | 65.31(17.727) | -.384 | .673 | .503 | |
| Social functioning | 48.86(23.108) | 47.19(17.542) | -.426 | -.418 | .677 | |
| pain | 41.18(18.763) | 40.51(14.179) | .050 | -.204 | .839 | |
| General health | 83.64(15.500) | 79.90(16.024) | -1.169 | 1129* (-1.434) ** |
.152 | |
3. DISCUSSION
This study assessed the impact of a modified Re-Engineered Discharge (RED) intervention on HRQOL 30 days post-CABG among Jordanian patients using a posttest randomized controlled design. A total of 104 patients (88%) completed the study [33]. Coronary artery bypass graft surgery involves a prolonged recovery, potentially impacting quality of life. Although substantial research exists on quality of life post-CABG, studies specifically examining the effects of discharge education and counseling on quality of life outcomes are limited [34, 35]. The results of the current study showed that the mean score for the total HRQOL SF36 scale was 49.93 (14.00) for the intervention group and 47.00 (11.85) for the control group, with a p-value of 0.27. The findings revealed a nonsignificant difference between both groups post-intervention. Akbari and Celik [34] investigated the effect of discharge training and post-discharge counseling on QOL among CABG patients. In this study, 100 patients were non-randomly assigned to intervention and control groups. The intervention included three training sessions, starting from admission, and provided in-hospital support with an educational booklet, discharge plan, and group counseling. Post-discharge support involved home visits and follow-up calls at 2, 10, and 6 weeks. Teaching methods comprised lectures, demonstrations, Q&A, and feedback. Post-discharge counseling addressed individualized needs and problem management. Six weeks post-discharge, SF-36 assessments showed significantly higher quality of life scores in the intervention group (93.19) than in the control group (47.00) [34]. The current study was inconsistent with a previous study [34]. The differences in results may stem from study design and intervention methods. In this study, patients were randomly assigned and received a single, one-on-one educational session post-operatively, with a written discharge plan but no comprehensive educational booklet. In contrast, the referenced study used a non-random assignment and provided an educational booklet covering the surgical procedure, care topics, complications, and post-CABG activities [34]. Moreover, the follow-up was limited to one follow-up call 2-4 days post-discharge without home visits compared to frequent telephone calls and home visits done by Akbari and Celik [34].
4. IMPLICATIONS FOR PRACTICE
Nurses are essential in post-surgery patient support, providing interventions that enhance recovery and reduce readmissions [36]. Interventions like discharge planning, education, home visits, follow-up calls, telehealth, and skilled nursing transitions reduce readmission rates [37]. The primary goal of these nursing interventions is to decrease mortality rates, prevent hospital readmissions, and enhance patient outcomes in CABG patients [38]. Effective discharge planning is essential for patients for their smooth transition home, addressing immediate and long-term care needs and ensuring continuity. In Jordan, it includes medication education, lifestyle advice (e.g., smoking cessation, diet), blood sugar/blood pressure management, and scheduling a follow-up within two weeks post-discharge.
5. LIMITATIONS AND STRENGTHS OF THE STUDY
The strengths of this study lie in its robust RCT design and fulfillment of all criteria for testing hypotheses, with block randomization minimizing investigator bias. However, limitations include potential investigator bias, as a single researcher conducted all study procedures. Additionally, the discharge summary transfer was constrained by hospital guidelines, and the small sample size may limit representativeness. Furthermore, the short duration (four months) of the study also restricts long-term outcome evaluation, limiting the findings to immediate post-intervention effects.
CONCLUSION
This study explored how a modified Re-Engineered Discharge (RED) intervention affects the quality of life for Jordanian patients after CABG surgery. The results showed no significant difference between the intervention and control groups, suggesting that a single educational session and minimal follow-up may not be enough to improve post-surgery outcomes. Previous studies with more comprehensive discharge education and follow-up support have shown better results, highlighting the importance of ongoing patient engagement. Nurses play a crucial role in ensuring a smooth transition from hospital to home, and effective discharge planning can make a real difference in recovery. While this study had strengths, such as its rigorous randomized design, limitations like a small sample size and short follow-up period suggest that more research is needed to develop stronger, long-term support strategies for post-CABG patients.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: H.S.A.: Study conception and design; J.A.A.: Investigation; D.A.M. and M.K.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CABG | = Coronary Artery Bypass Grafting |
| RCT | = Randomized Controlled Trial |
| AHCP | = After-Hospital Care Plans |
| DE | = Discharge Educator |
| HRQOL | = Health-Related Quality of Life |
| RED | = Re-Engineered Discharge |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study received ethical approval from the ” Royal Medical Services Human Research Ethics Committee no.5/2020.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Oral and written consent was obtained from all participants before the study began.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [D.A.M] upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


