All published articles of this journal are available on ScienceDirect.
Communication Methods Used with Conscious Intubated Patients: Scoping Review
Abstract
Background
Intubated conscious patients often experience communication difficulties. The present narrative review outlines the current evidence on communication methods adopted and the experience of conscious intubated patients in critical care areas.
Objectives
To our knowledge, studies have attempted to examine communication with conscious intubated patients. The present review had two objectives: (1) to identify the methods adopted by nurses and conscious intubated patients to ease the communication difficulties faced due to intubation and (2) to identify the experience of nurses and conscious intubated patients with the adopted communication methods.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist was followed throughout this review. PubMed and ProQuest databases were searched with the terms “intubated conscious patients,” “communication,” and “nurse”, including original research articles published between January 2019 and May 2024 on conscious patients needing intubation. Dissertations, review papers, non-interventional research, and articles written in languages other than English were excluded. Only eight of the original 2,041 studies, which included 137 intubated patients and for 545 nurses, met the inclusion criteria. The authors used the Mixed Method Appraisal tool (MMAT) and the Critical Appraisal Skills Program (CASP) to collect data and assess quality.
Results
After the first search of generated 2041 papers, only eight articles—representing various studies—were able to meet the inclusion requirements. The included studies were six (6) quantitative, one (1) qualitative study and one (1) mixed-method study. Four communication intervention types were identified, namely: (1) Communication boards/charts (two studies), which improved communication and increased patient satisfaction. (2) Gestures and facial expressions (four studies) were reported to be frequently initiated for communication by the nurses with the patients. (3) Multiple methods (three studies) used were found to be insufficient to communicate with the patients. (4) Digital technology program, including Communicative Digital Technology Program was found to be effective means of communication in three such studies.
Conclusion
Results imply that communication techniques may be useful in enhancing patient–nursing professional communication with conscious intubated patients. However, in developing countries with fewer resources, a low-cost communication tool addressing both physical and emotional needs may be developed to aid in communication among patients and nurses.
1. INTRODUCTION
No matter how greatly developed we become scientifically and technologically, humans will always need humans to interact physically. We are emotional beings who crave one-to-one personal connection. More so when we are sick; for the patients who are taken in for care at a very low point in their lives, nothing could be more important than being able to communicate with their caregivers. Also, for caregivers, communication and personal connections are the most meaningful interactions.
In ICUs, there has been a paradigm shift over the past ten years with the adoption of no-sedation protocols, mild sedation, daily sedation breaks and decreasing use of heavy sedation [1-3]. This is aimed at shortening the duration of mechanical ventilation and the length of stay in the intensive care unit; daily interruption of sedation, no sedation, and light sedation are implemented in critically sick and mechanically ventilated patients [4].
With the recent intubation practices to keep patients awake [5], critically ill patients experience extreme difficulties in communication because of intubation and associated cognitive, sensory and language deficits [6]. Often, this distances patients from their caregivers and loved ones. Difficulty in communication may cause stress, anxiety and depression among intubated conscious patients and eventually, the prognosis becomes poor [6, 7]. Research has shown that effective communication between patients and healthcare providers is essential for the treatment and recovery of patients [8-10]. To improve patient-centered care, it is imperative to prioritize tailored communication approaches and to sustain supportive interactions with patients throughout their treatment path [11].
Though it doesn't always go as planned, health professionals recognize the importance of communication [12]. Sharing ideas, concerns, and facts with others at a particular time and location is the process of effective communication. Poor treatment outcomes, resource misallocation, increased healthcare costs, and, in extreme situations, even death can result from ineffective communication [13].
Communication difficulties not only affect the patients but also affect the nurses. A study [14] reflected nurse-patient communication in conscious intubated patients is characterized by a common experience – frustration [6]. Communication problems increase the possibility that patients' gestures may be misinterpreted, which can lead to patient dissatisfaction and frustration for both the patient and the caregiver [15, 16].
Nurse-conscious mechanically ventilated patient communication (N-CMVPC) is defined as a collection of attributes in communication experiences, emotions, methods, and behaviours of the nurse and the patient. It is categorized using three main themes: nurse commu- nication, patient communication, and quantitative-qualitative aspects. It may take the form of questions, statements, or instructions and is often nurse-controlled, even though it depends on the experiences, feelings, and positive or negative behaviours of the patient and nurse [17].
To overcome communication difficulties, critical care nurses often use different ways to interpret nonverbal forms of communication (such as gesturing) [6], but most of the time, nurses guess the need [18]. A study proposed a variety of non-verbal methods and tools to enhance communication in conscious intubated patients [19]. Non-verbal methods require not only a lot of energy and motivation but are also tiring and emotionally draining for patients and the caregiver both [20]. Researchers in their meta-analysis have reported that Augmentative and Alternative Communication (AAC) may enhance communication, which is available in different forms such as speech, text, gestures, sign language, symbols, images and electronic speech-generating devices [21]. The analysis also showed that AACs are available in two forms: low cost, low technology-based and costly, high-technology-based. Meanwhile, researchers have proposed to design and implement future packages to aid in communication which are easy to use [14]. An in-depth inquiry into the communication with conscious intubated patients is done to aid in the development of cost-effective, low technology-based communication tools for intubated conscious patients as an intervention that may help to enhance communication in the critical care area, addressing both physical and psychological needs.
1.1. Objectives
To our knowledge, studies have attempted to examine communication with conscious intubated patients. The present review had two objectives: (1) to identify the methods adopted by nurses and conscious intubated patients to ease the communication difficulties faced due to intubation and (2) to identify the experience of nurses and conscious intubated patients with the adopted communication methods.
2. METHODS
A scoping review approach was adopted with specific selection criteria on studies under review. The present review adhered to the PRISMA-ScR checklist in the development and reporting of its objectives, analysis techniques, inclusion and exclusion criteria [22].
2.1. Study Selection Criteria
This scoping review included both quantitative, qualitative research and mixed method research designs as described in Table 1. Quantitative studies included RCT, quasi-experimental and cross-sectional observational studies (but not reviews). Communication with patients who were conscious but intubated was the main area of attention.
| Author and Year/Refs. | Rationale for Exclusion-unrelated to Communication Ease/methods |
|---|---|
| Momennasab et al., 2022[22]. | Evaluation on training program effectiveness for AAC |
| Bodet-Contentin et al., 2022[23]. | Study on ICU patients not necessarily conscious intubated patients only were included |
| Istanboulian et al., 2021[24]. | Study to assess communication difficulties during Covid-19 with infection control precautions in the context |
| Zasso et al., 2021[25]. | Decision-making in a simulated airway emergencyby healthcare team-Not communication devices for patients |
| Decavèle et al., 2023[26]. | Interventions relieving dyspnea in intubated patients |
| Wang et al., 2020[27]. | Comparison between dexmedetomidine and midazolam for sedation in patients with intubation |
| Lewis et al., 2022[28]. | Cuff leak test and airway obstruction in mechanically ventilated intensive care unit patients |
Relevant literature was identified by using various databases and the search was limited to published English articles involving conscious intubated patients. Both qualitative and quantitative research studies were reviewed to increase the span of review results.
2.2. Information Sources and Search Strategy
Electronic databases (Pubmed and Proquest) were thoroughly searched. Only full-text, peer-reviewed research manuscripts from the past five years were considered. The publishing dates (January 2019 to May 2024), document type (original article), language (English only), and source type (scholarly journal) were the filters that were used. Only full-text articles that underwent peer review were included. The first two researchers (M.K. and S.L.P.) independently examined every paper to determine its applicability to the goal. The other two researchers, S.L.P. and F.M.S., checked the technique for accuracy. Included were research publications using any one of the three following designs: mixed, qualitative, or quanti- tative. Studies that comprised a cohort of conscious intubated patients were included. Excluded from consideration were evidence-based research, dissertations and theses, reviews of relevant literature, case studies, field reports, general data, conference proceedings, and commentary. The eight chosen studies and the references from pertinent reviews were manually searched in addition to the list. The electronic search approach merged text terms with keywords. Two concepts served as the foundation for the electronic search: (1) research on nurses' communication with conscious intubated patients; and (2) research on communication challenges using current communication tools. There were search language restrictions of the English text only. There was no relevant unpublished research found, despite tracking the development of abstracts and papers or publications presented at conferences. In addition, manual searches of important journals in the area were conducted using the reference lists of published works that met the study's eligibility requirements. These journals included the American Journal of Nursing, the British Journal of Nursing and Nursing Made Incredible Easy.
Though the initial search was started with “communication strategies,” later, the preliminary search for relevant communication methods used by conscious intubated patients and nurses were done from a few manuscripts and then the most quoted ones like “communication tools” and “aids” was taken into account for further search.
The search terms included were ‘conscious intubated patients’, ‘communication’, ‘nurse’. To fulfill the purpose of the review of literature terms were matched and combined together to include all studies and get an extensive search on relevant research studies. The string used was “communication or tools or aids and nurses and conscious intubated patients”. After doing a preliminary search, 2041 studies in total were found. By manually scanning through the identified papers' reference lists, only two studies were found. Of these, 1769 articles were disqualified because they weren't peer-reviewed, full-text, scholarly, or hadn't been released before 2019. Based on the inclusion and exclusion criteria, 253 articles were removed from the remaining 272 articles, leaving 19 articles. The final search consisted of 19 articles screened on the basis of title and abstracts.
2.3. Inclusion and Exclusion criteria
Research that documented any correspondence between nurses and the aware intubated patients qualified for inclusion. Participants using non-invasive equipment were excluded, along with those with all forms of intubation. One of the study's outcomes was an increase in communication. This review only covered original English language articles that were accessible in their entirety. Conversely, the following were not included: field reports, general information, conference proceedings, disser- tations/theses, literature reviews, field reports, and commentary. Articles written in languages other than English were also disqualified.
These nineteen manuscripts underwent additional filtering, and seven of them were eliminated at this stage because they had nothing to do with the issue i.e., related to communication. (Table 1) [23-29]. The remaining twelve studies were evaluated to determine their applicability to the objective. Four more articles were eliminated in this step; one of them was on the paediatric group, one was not in English, one was non-invasive ventilator BiPAP and one was duplicate. Ultimately, this review contained eight studies (Table 2). M.K. and S.L.P. evaluated the chosen studies in order to extract data using the PICO (Population, Intervention, Comparators, and Outcomes) framework [30]. M.K, S.L.P and F.M.S. manually verified the included studies' methodological soundness and intervention effects.
| Broad Categories | Sub-heading of Broad Categories | Types of Research Designs | Number of Studies |
|---|---|---|---|
| Quantitative | Cross sectional | Descriptive | 1 |
| Quantitative | Experimental | Quasi-experimental | 3 |
| Quantitative | Observational | Descriptive | 1 |
| Quantitative | Observational | Prospective | 1 |
| Qualitative | - | - | 1 |
| Mixed method | - | - | 1 |
Using the Critical Appraisal Skills Programme (CASP) checklist (randomized control study, cohort, or qualitative study checklist), M.K and S.L.P. evaluated the studies on their own [31-33]. The quality of the mixed-method studies was evaluated by the same authors using the Mixed Methods Appraisal Tool (MMAT) [34]. To reduce error, M.K., S.L.P. and F.M.S. subsequently verified both processes. Thus, the methodological bias was eliminated.
Using the American Association of Critical-Care Nurses Levels of Evidence, every included study was carefully evaluated to determine the quality of the evidence [35]. Meta-synthesis of qualitative research or meta-analysis of quantitative research are included in level A, whereas well-designed controlled trials (randomized or non-randomized) with results that consistently support a particular course of action, intervention, or treatment are included in level B. Qualitative research, descriptive research, systemic reviews, and randomized trials with contradictory findings are all included in Level C. Peer-reviewed professional and organizational standards backed by recommendations from clinical studies are included in Level D. Only the manufacturer's suggestions are included in Level M. Only levels B and C applied, given the included research in the current evaluation.
2.4. Study Selection
Based on the specified research inclusion criteria, an independent screening process was carried out (refer to Fig. 1). Duplicate and irrelevant research was eliminated after the titles and abstracts of each study were first examined. To ascertain if inclusion requirements were satisfied, the whole texts of possibly pertinent papers were further reviewed. The final inclusion of studies was(n =8). All of the included studies were published between January 2019 and May 2024.
2.5. Data Synthesis
A scoping review was used instead of combining quantitative and qualitative data to do a meta-analysis because of clinical variation in the methodology, treatments, and outcomes of the included studies.
In order to achieve the objectives, the studies included in this scoping review were examined to identify the experience of patients and/or nurses who faced challenges while using a particular communication method.
This was followed by a stepwise search for appropriate articles, illustrated in Fig. (1).
3. RESULTS
The studies were selected and analyzed for a year of study, author, and study design, sample and major findings. Full text articles were examined on the basis of mentioned search terms and reviewed to match the purpose. All studies that did not match the purpose were excluded. The final review database consisted of a total of eight full-text articles.
After reading and re-reading the articles, central theme was jotted. This was followed by interpreting the themes. Characteristics of the included studies are summarized in Table 3 [36-43]. There are five (5) quantitative, two (2) qualitative and one (1) mixed-method studies. Studies are mostly published in journals related to critical care, intensive and critical care nursing and anesthesiology.
A total of four adopted communication methods have emerged through the search:
communication boards/charts (two studies);
gestures and facial expressions (four studies);
multiple methods (three studies);
Digital technology program (three studies).
The outcomes reported contained a wide range of measures. All the researchers have focused on the improvement of communication and assessed the methods adopted using different tools. Most commonly subjective assessments of improvement of communication or investigator-developed questionnaires were used.
Researchers have found mixed communication experience. The reviews didn’t highlight any specific patients.However, reduction in communication difficulty with the communication board, though training requirements for the use of communication aids have been reported [36-38]. The study recommended the use of AACs to augment communication strategies. According to qualitative data, the ICU-COM helped nurses manage communication problems, and nurses thought the tool was useful and appropriate in general, though implementation challenges were identified with multi-component approach- ICU-COM [39]. Various studies have revealed that the communication pattern assessment allowed the nurses to find out and distinguish the sources of patients’ discomforts and disturbed symptoms, notably the domains such as psychological, physiological, spiritual, comfort needs, expectations and planning appropriate AAC for aware MV patients [43].
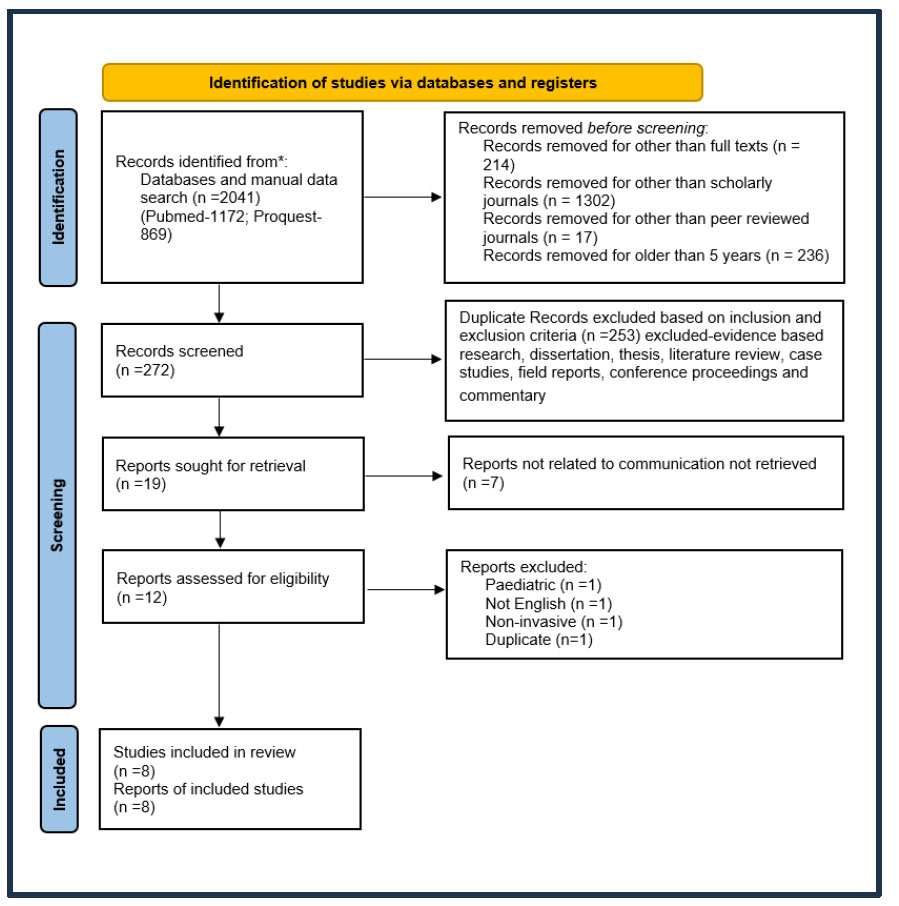
Flow chart of narrative literature review.
(PRISMA Group, 2020).
| S.No. | Study Year | Study/Refs. | Author | Study Design | Sample | Major Finding | Level Of Study | |
|---|---|---|---|---|---|---|---|---|
| - | - | - | - | - | - | Methods Adopted | Communication Experience | - |
| 1 | September 2019 | A simple aid to reduce communication difficulties of mechanically ventilated patients in the ICUs [36]. | Bhardwaj, Kiran & George, Mini | Posttest only designquasi experimental | 50 intubated patients | Communication Board | Reduction in communication difficulty | B |
| 2 | December 2022 | Communicating with mechanically ventilated patients who are awake. A qualitative study on the experience of critical care nurses in Cyprus during the COVID-19 pandemic [37]. | Kyranou, Chariklia, Eliada | Qualitative study | 14 ICU nurses | Strategies of unaided (movements-lips, hands, legs-facial expressions, gestures, touching) and aided forms of communication (pen and paper, boards, tablets, mobiles) | Nurses are neither trained in augmentative and alternative communication methods nor have access to the necessary communication tools. | C |
| 3 | April 2021 | Communicating to Non-Speaking Critically Ill Patients: Augmentative and Alternative Communication Technique as an Essential Strategy [38]. | Al-Yahyai, R., et al | Cross sectional descriptive survey research design | 194 nurses | Reading the patient’s mouthing words and gestures | Traditional communication strategies were not enough for effective communication | C |
| 4 | November 2022 | A multicomponent intervention to optimise nurse-patient communication in the intensive care unit: A mixed-methods acceptability and feasibility study [39]. | Holm A, Nikolajsen L, Dreyer P | A mixed-methods design | 300 nurses | Multi component approach-ICU -COM | Implementation challenges were identified and the delivery needs to be repeated | B |
| 5 | July 2022 | Opportunities for interactive communication in mechanically ventilated critically ill patients: A video-based observational study [40]. | Yamaguchi, A et al. | Descriptive observational study | 7 patients and 7 nurses | Gestures and facialex pression by patients, verbal communication by nurses | Nurses created communication opportunities more frequently than patients did | C |
| 6 | January 2023 |
A user evaluation of speech/phrase recognition software in critically ill patients: a DECIDE-AI feasibility study using multiple triangulations [41]. | Musalia et al., 2023 | Prospective study | 14 patients with tracheostomies | Dynamic time warping (DTW) and deep neural networks (DNN) methods in a speech/phrase recognition application | Speech/phrase recognition technology could be a therapeutic option to bridge the gap in communication in critically ill patients | B |
| 7 | June 2023 | Needs communicative digital technology program for intubated patients with critical illnesses: A quasi-experimental study [42]. | Nuttapol C & Bunthan, W | Quasi-experimental study | 30 each in experimental & control group of intubated patients | Needs communicative digital technology program | Successful in meeting participants ' needs and improving the efficacy of communication | B |
| 8 | February 2022 | Assess the communication pattern among conscious mechanical ventilation patients and nurses in the selected intensive care unit [43]. | Neelavathi P, Bhubaneswar G, Umapathi. M | Quasi experimental study (pre- test and post- test design) | 10 experimental & control group intubated patients and 15 nurses | Pen and paper and gesture and facial expression | Communication with intubated patients was found to be of great challenge nursing personnel | C |
Traditional communication strategies like mouthing words and gestures were not sufficient and were found to be challenging for effective communication for both nurses and patients, though most of the time nurses initiated the same [38, 40, 43]. But digital methods could successfully bridge the communication gap [41]. It was clear from the program's utilization of cutting-edge technology of the Needs Communicative Digital Technology Program that intubated patients with serious illnesses can have their demands efficiently satisfied [42].
4. DISCUSSION
4.1. Communication Methods Adopted and the Experience
4.1.1. Communication Boards/Charts
Common demands are represented by symbols and images on a communication board for intubated patients. Four investigations were conducted using this: three quasi-experimental studies and one RCT [36, 37]. The quantitative study on intubated patients during weaning evaluated the effectiveness of the Communication Board and found reduced Communication Difficulty. However, no significant relationship was found with the patient’s demographic variables and clinical characteristics [36].
The studies have also reported that patients who are undergoing awake intubation days experience moderate to extreme levels of psycho-emotional distress due to the inability to speak or communicate their needs, which leaves them helpless and frustrated [44]. This study evaluated the effectiveness of a communication board on ease of communication. On one side of the board, the patient's needs were represented in textual form and relevant visuals. The other half of the board was divided into two sections: a whiteboard and a schematic image of the body. The findings supported that the use of a communication board can facilitate communication and lessen patients' anxiety [45]
In addition to the similar quantitative findings on the effectiveness of the use of the communication board, several qualitative remarks were provided on recommen- dations for certain changes to the communication board, such as increasing the font size and reducing the number of written word alternatives [45]. Another study evaluated the effectiveness of a communication chart that emphasized the intubated patient's physical, emergency, and psychological requirements to be effective [46].
4.1.2. Gestures and Facial Expression
Studies have discussed the use of gestures and facial expressions as a practiced method of communication [37, 38, 40, 43]. A descriptive observational study evaluated the use of unaided communication where nurses initiated contact with patients or observed and addressed the Patient-Intentional-Action, and then chances for communication with the patients were established. The result showed that nurses should not wait for the patient to initiate communication; instead, they should be able to identify and react to patient-intentional action. The study reflected that the nurses did initiate communication with the intubated patients and emphasized the need for communication [6, 40]. Whereas cross-sectional descriptive study, a qualitative study and a study on patients and nurses found reading patients mouthing words and gestures were not enough to establish effective communication [37, 38]. All the studies reiterated the need for developing effective communication devices for such patients.
5. MULTIPLE METHODS
In one qualitative study, nurses employed assisted (pen and paper, boards, tablets, mobile phones) and unaided (movements—lips, hands, legs—facial expressions, gestures, touching) ways of communication with patients. The study concluded that the complex communication demands of critically sick patients are unmet due to a lack of training for nurses and a lack of technology to support augmentative and alternative communication [37].
A similar study evaluated the communication between patients and nurses both simultaneously using pen and paper along with facial expressions and gestures. The results of this study demonstrated the challenges of the nursing staff to communicate with intubated patients. The patients find it difficult to pinpoint the causes of discomfort and distressed symptoms and to satisfy their psychological, physiological, spiritual, and comfort needs [43]. The study reflected the use of multiple methods to communicate but still identified the need to develop better communication devices.
In another study, although the results of the qualitative and quantitative research were somewhat contradictory on the effectiveness of ICU-COM, they did show how the intervention may be improved to fit with clinical practice and get across implementation issues of the tool [47]. (Holm, Nikolajsen and Dreyer, 2021). Another study by Ten Hoorneet al., (2016), in their narrative review, suggested that a combination methods of AAC communication methods may be effective in improving patient–healthcare professional communication with mechanically ventilated patients [6, 47].
5.1. Digital Technology Program
A study evaluated the effectiveness of Needs Communicative Digital Technology Program (NCDTP) of 30 requirements converted into voice messages, text messages, and picture messages fed into the tablet. The audio messages get transmitted to the computers at the nursing station when the patients push the screen to express their wants via the tablets. The nurse would then be aware of the patients' needs and able to promptly address them. The results of this study showed that the 48-hour NCDTP was successful in meeting participants' requirements and improving communication [42]. A mixed method study with multi-component approach ICU-COM found effective results on communication, but challenges in the implementation of the ICU-COM were faced [39]. Dynamic time warping (DTW) and deep neural networks (DNN) was found to be Speech/phrase recognition technology which could be a therapeutic option to bridge the gap in communication in critically ill patients [41]. A recent study discussed the use of eye-tracking systems in addition to eye-blinking, lip-reading and similar methods that helped in communication with conscious patients in critical care areas [48].
For further clarity into the digital programs used and their cost effectiveness, which may be applied to the setting of the developing country, the researchers and the organisations would be contacted by the researchers prior to the development of communication tools to ease the communication.
5.2. Nurse Patient Characteristics and Barriers to Usage of the Communication Intervention
The adopted communication methods were effective for most of the participants being nurses having more than one year of experience in critical care areas [38, 39]. Time constraints evolved to be the barriers to their use [44, 45]. Patients who used the communication boards were able to read the prints, oriented, and had been intubated for more than five days [1, 3, 7, 19].
Along with the many advantages of the use of communication aids, few issues were also found while using the various communication boards, like too many cues on them and font size too small including several patients’ needs and requirements missing from the board [7]. For the communication tool with the tablet, the main constraint of the tablet being Android, other devices could not be used [14]. Fatigue, a lack of upper extremity muscular power or coordination, a short attention span, or drowsiness was also found as obstacles to utilizing the different communication methods [18, 19].
In spite of studies reporting barriers of using different kinds of communication methods, it is evident from the studies that nurses have been instrumental in trying and implementing communication methods. More evidence-based studies are required to develop easily available and cost-effective, easy-to-use devices for ease of communi- cation with conscious intubated patients.
5.3. Limitations
The review was not entered for registration into Prospero, because of the heterogeneity of the included studies including differences in study designs, different interventions to promote communication between nurses and conscious intubated patients used in different combinations, and wide variations in analysis techniques and outcome measures—a meta-analysis could not be conducted. It was not possible to create a forest plot or another similar graphical representation of the results to display any point estimates obtained from selected research about the same condition or treatment because the selected studies were quantitative, qualitative, and mixed methods studies.Communicating and establishment of a therapeutic relationship with intubated patients is challenging but not impossible. Thorough knowledge of the experience of nurses and the barriers faced by conscious intubated patients will help develop a suitable communication tool [6, 49, 50]. The use of communication tools may significantly reduce miscommunications and help develop more successful nurse-patient communi-cation [6, 51].
5.4. Summary
Findings from this review generated substantial evidence of communication experiences and the methods adopted by the nurses and patients to ease communication separately.Only one study focused on the communication experience of both patients and the nurses’simultaneously. Articles were reviewed to understand mainly the nurses among health care providers. The main goal of this review was to identify existing evidence regarding communication with intubated conscious patients. The main purpose was to construct the development strategies to aid in effective communication with these conscious intubated patients and also help the nurses understand patients' need. Nursing personnel in the ICU who are trained and become familiar with communication strategies on the use of communication devices or tools would probably deliver quality patient care in terms of patient satisfaction.
CONCLUSION
The findings of the review would help to develop effective communication tools to be undertaken in other hospitals and settings to ease the professional’s communication skills.
The researcher being from a developing country, and high-cost digital tools may not be feasible; thus, a low-cost effective communication tool like a communication board with visual cues may be adopted based on experiences and needs expressed by patients and nurses. Since nurses could contribute a lot towards holistic health in the work situation by sharing their communication experience, studies of this sort would help improve the quality of nursing services in the critical care area. The use of effective communication techniques using developed communication tool-visual cue card to communicate with conscious intubated patients may be included in the curriculum of various nursing programmes to orient the student nurses to this area of nursing practice. Moreover, the administrator may create a good working environment and provide effective communication tools- visual cue cards to the clinical nurses for communicating with conscious intubated patients. Also, how the intubated patients prefer to communicate need to be explored and thereby improve the therapeutic communication relationship between nurses and the patients by developing a communication tool.
RECOMMENDATIONS FOR FURTHER RESEARCH
The relationships between experience and adopted communication methods discovered may serve as the foundation for the communication tool development. The tool must be discussed during the design process with a team focusing on communication with critically ill patients, which included intensivists, critical care nurses, and student nurses.
AUTHORS' CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PRISMA-ScR | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| CASP | = Critical Appraisal Skills Program |
| MMAT | = Mixed Method Appraisal tool |
| N-CMVPC | = Nurse-conscious mechanically ventilated patient communication |
| AAC | = Augmentative and Alternative Communication |
| PICO | = Population, Intervention, Comparators, and Outcomes |
| CASP | = Critical Appraisal Skills Programme |
| MMAT | = Mixed Methods Appraisal Tool |


