All published articles of this journal are available on ScienceDirect.
A Case Report on Placenta Accreta: Developing a Conceptual Framework
Abstract
Introduction
Placenta accreta is a pathological condition of the placenta associated with multiple maternal and neonatal complications, but its diagnosis and treatment have been sparsely reported from the nursing viewpoint. This report describes a case of placenta accreta from the nursing perspective to develop a conceptual framework of care.
Case Presentation
Our case involved a 37-year-old pregnant woman with four previous caesarean sections and a previous in vitro fertilisation. She was diagnosed with placenta accreta only in the operating theatre during a scheduled caesarean section, and she had not performed thorough antenatal care as in her previous pregnancies despite having significant symptoms, such as severe urinary incontinence. The patient experienced many complications during the caesarean section, including bladder injury, massive haemorrhage, and hysterectomy.
Conclusion
We develop a theoretical framework illustrating the core factors that influence the management of placenta accreta and associated maternal morbidities. This model highlights the distinction between patient characteristics, nurse characteristics, organisational factors, and pregnancy outcomes and shows their relationship to the diagnosis and prevention of placenta accreta. The model has important implications for research and practice, and the case reminds nurses of their recommended interventions to diagnose, manage, and prevent placenta accreta. The quality of care for placenta accreta cases should be promoted through the assessment of patients, nurses, and organisational factors and the application of prevention measures.
1. INTRODUCTION
Placenta Accreta (PA) is a placentation disorder in the gravid uterus that is characterised by placental invasion only to the surface of the myometrium [1, 2]. PA increases the risk of adverse maternal and neonatal outcomes, such as postpartum haemorrhage, hysterectomy, bladder injury, preterm birth, admission to the Neonatal Intensive Care Unit (NICU), and death [1-4].
The incidence of PA is increasing worldwide [1, 2] due to the growing number of previous Caesarean Sections (CSs), increased maternal age, multigravidity, congenital uterine disorders, previous In Vitro fertilisation (IVF), and previous uterine procedures [1, 3, 4]. These factors are associated primarily with alterations in hormone levels and in the implantation environment, especially in the presence of previous scars.
A review of the literature reveals problems with the diagnosis of PA [5, 6]. Several reports [6-8] recommend using ultrasonography to diagnose suspected PA, whereas Magnetic Resonance Imaging (MRI) is not deemed ess- ential. When PA is diagnosed prenatally, it should be managed by expert multidisciplinary teams (an obste- trician specialised in complex pelvic surgery and foetal medicine, anaesthesiologist, urologist, etc.) in a tertiary care hospital, that is, a specialised centre that includes adult intensive care as well as a blood bank to support access to blood products. Furthermore, PA guidelines recommend the administration of corticosteroid drugs for lung maturity between 32–34 weeks if PA is diagnosed and preterm birth is expected [6-8]. The nurse’s role focuses on managing high-risk women in emergency situations, such as PA, so nurses should possess good knowledge and practices related to PA management guidelines and protocols so as to be confident when caring for PA patients in collaboration with a multidisciplinary team.
To our knowledge, most previous reports investigated the diagnosis, risk factors, and management of PA from the obstetric and gynaecological perspectives. The present report describes a unique case of PA to raise awareness of management and prevention measures for PA from a nursing perspective. Therefore, a conceptual framework was designed to analyse this case and provide insights on the dimensions of nursing care for women with PA to achieve better health outcomes.
2. CASE PRESENTATION
A 37-year-old woman of high socioeconomic status with four previous CSs (three girls and one boy) was diagnosed with PA during her fifth CS. Before this pregnancy, spontaneous pregnancy did not occur for two years due to blockage of the fallopian tube as diagnosed by hysteroscopy. One trial to conceive a male child by IVF failed. After two months of IVF, spontaneous pregnancy occurred as diagnosed by a missed menstrual period at eight weeks of gestation. At four weeks of gestation, the patient experienced vaginal bleeding equivalent to menstrual flow. The obstetrician did not recognise this, and the patient was unaware of this critical symptom.
At the end of her pregnancy (around 35 weeks), the woman had severe urinary incontinence, which she had not experienced in previous pregnancies. She ignored this complaint and did not seek antenatal care, as her great wish was to complete the pregnancy and have another male child. During this period, she underwent routine antenatal follow-up in a private obstetric clinic. She did not undergo a detailed ultrasound screening in this pregnancy as in previous ones.
PA was diagnosed only at childbirth during a planned CS at 37 weeks under spinal anaesthesia in a govern- mental secondary care hospital in Jordan. The patient experienced many complications, including massive haemorrhage, hysterectomy, and bladder injury; the baby was admitted to the NICU and the mother to the intensive care unit. She believed that the adverse outcomes occurred due to a lack of early antenatal diagnosis of PA, as she had intentionally followed less antenatal care.
The patient reported that another expert obstetrician and a urological surgeon were called from outside the hospital to manage her case, and blood products were prepared from two other hospitals. Only after the ope- ration did she learn that she had a unicornuate uterus (one having a single fallopian tube and an abnormally shaped uterine cavity). She was discharged from the hospital after one week with her baby in relatively stable condition.
Ethical review and approval were waived for this study due to its adopting a case report design with a single patient whose information was obtained retrospectively.
3. DISCUSSION
The case presented in this study has implications for nursing practice and research related to the diagnosis, prevention, and management of PA. We developed a conceptual model (Fig. 1) that describes patient, nurse, and organisational factors in addition to nursing actions, which are described according to the three levels of prevention measures.
Regarding patient characteristics, our case had many risk factors for PA (Fig. 1), as well as subjective complaints or symptoms that could indicate the risk. However, women’s perceptions and attitudes towards pregnancy may affect the extent to which they seek antenatal care. In other words, maternal intention to seek sufficient antenatal care may be low among high-risk women whose pregnancy is planned and desired, as indicated in our case. In that vein, some studies have found that adverse pregnancy outcomes were associated with inadequate antenatal care, especially among high-parity women [9, 10]. Although few studies to date have investigated high-risk women’s emotions and beliefs about antenatal care, one qualitative study revealed that pregnant women had high levels of stress related to the unborn baby, preferred not to know about their medical condition, and were not motivated to seek antenatal care [11]. Further research is needed to evaluate beliefs and attitudes toward seeking antenatal care among high-risk pregnant women, particularly if PA is suspected.
Furthermore the level of nurses’ knowledge about PA may affect its early diagnosis and treatment (Fig. 1). To our knowledge, there is a gap in research on the knowledge and expe- rience of nurses in the management of PA. One qualitative study revealed that healthcare providers generally experienced emotional distress and medical helplessness when PA was diagnosed [12]. It suggests a need to develop and examine the effectiveness of educational interventions on PA management for nurses in clinical practice.
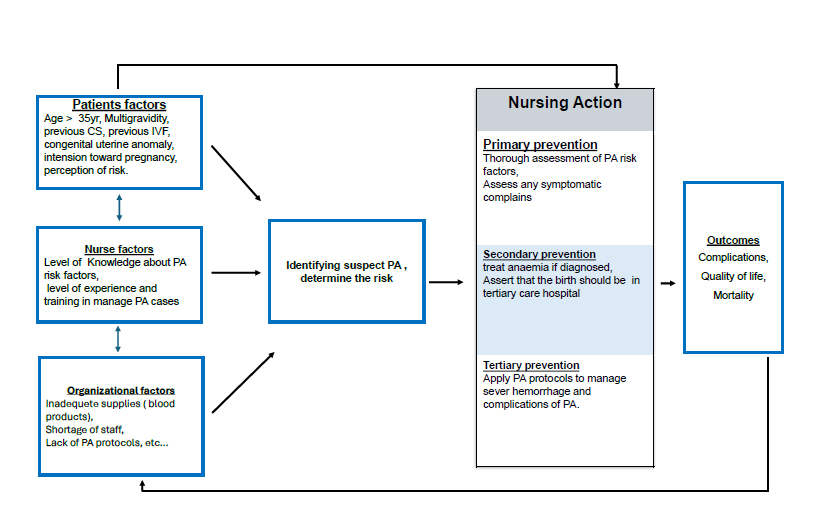
Conceptual framework reflecting nursing care of placenta accreta (PA).
In addition, our case shed light on resources and staff in maternal and neonatal health care settings. Organisational characteristics should meet the needs of high-risk women with PA (Fig. 1). One Jordanian study found that governmental hospitals experience deficiencies in health services and resources in maternal and neonatal settings [13], which was apparent in our case.
Primary prevention interventions should focus on the early identification of suspected PA. This can be achieved by taking a thorough patient health history, developing educational interventions and training on PA management for nurses, and improving the quality of resources and health services in health care settings.
Nurse leaders should recognise the secondary prevention measures that are reported in some obstetric guidelines [6-8]. When PA is diagnosed prenatally, corticosteroid drugs should be administered to women at high risk of preterm birth, and haemoglobin should be maintained within the normal range. Health education sessions and interventions can increase women’s awareness of the risk of PA [6-8]. Applying prenatal care protocols for PA has a positive effect on maternal and neonatal health outcomes, as evidenced by an Egyptian quasi-experimental study [14].
Nurses should adopt tertiary prevention measures when PA is diagnosed and haemorrhagic morbidities occur. In that effort, collaboration with expert multi- disciplinary teams is essential. Blood products should be arranged and given in this life-threatening condition, and neonatal and adult intensive care units should be prepared to provide supportive care to improve maternal and neonatal health [6-8]. Psychological interventions should be provided to patients and families during and after birth. Generally, nurse and midwife care should be directed towards promoting neonatal health and improving maternal quality of life after birth, consequently decreasing morbidities and mortalities.
Our conceptual framework may be used in future research efforts to clarify the degree of association between the interrelated factors, prevention measures, and pregnancy outcomes. Specific attention should be directed towards modifiable factors that contribute to better health outcomes.
A limitation of this case report is its focus on the phenomena of PA in a single patient, so the findings cannot be generalised to all patients with PA. Moreover, our case illustrates only the significant role of medical teams rather than nursing staff in managing and diag- nosing PA. This requires further studies that investigate the knowledge and practice of nurses in managing PA.
CONCLUSION
Our conceptual framework illustrates the complex interplay of factors that can impact the management of PA and its pregnancy outcomes. It suggests clear implications for developing effective interventions, research, and policies for women with or suspected of having PA. The application of PA guidelines and protocols in healthcare settings contributes to its early diagnosis and management. Nurses should take a thorough, compre- hensive health history, have good knowledge of PA risk factors, and pay attention to women’s subjective symptoms, which could indicate a pathological condition or suspected PA. Furthermore, nurses must collaborate with other healthcare professionals in caring for women and babies in the operating theatre and after birth. Nurse and midwife care should be directed towards promoting neonatal health and improving maternal quality of life after birth, thereby decreasing morbidities and mortalities.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| PA | = Placenta Accreta |
| MRI | = Magnetic Resonance Imaging |
| CSs | = Caesarean Sections |
ETHICAL STATEMENT
Ethical review and approval were waived for this study due to its adopting a case report design with a single patient whose information was obtained retrospectively.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patient before the writing of this report, and the patient provided written informed consent to publish this paper.


