All published articles of this journal are available on ScienceDirect.
Nursing Clinical Assessment of Factors Associated with Depression in Older People with Type 2 Diabetes in Primary Care: A Cross-sectional Research
Abstract
Background
Brazil has one of the largest older populations and people with diabetes. Non-communicable diseases account for 10.2% of hospitalisations in older people due to causes sensitive to primary care.
Objective
This study aims to evaluate the factors associated with depression in older people with type 2 diabetes in primary care, according to the clinical nursing judgment based on NANDA-I Taxonomy II.
Methods
This is a cross-sectional study of 389 older people with type 2 diabetes in primary care in a municipality in the state of São Paulo, Brazil. A bivariate analysis was performed to associate sociodemographic and clinical exposure variables with the outcomes of the geriatric depression scale. Only those variables associated at the level of p < 0.20 level were entered into a multiple logistic regression model.
Results
The study identified two predictive factors: adherence to medication “low to probable low” (p=0.01; OR = 2.07 [95% CI 1.18-3.63]) and probability of repeat hospitalisations (Prh) (p<0.01; OR = 2.68 [95% CI: 1.42-5.04]). Therefore, it can be concluded that these factors are significant in predicting the outcome.
Conclusion
Based on the interpretation of these factors, a cyclical procedural model has emerged that predicts and fosters depression in the population covered by primary care services, as well as signalling a risk for unstable blood glucose level and consequently a risk for metabolic syndrome and frail elderly syndrome. This is due to poor health in the community, which is related to programme failure and puts the group at risk.
1. INTRODUCTION
Brazil has one of the largest populations of older people in the world [1], which is expected to triple by 2050 and surpass that of children. This demographic change is accompanied by an epidemiological transition, charac- terised by the prevalence of non-communicable diseases (NCDs) [2], particularly among older people. In fact, 75.3% of the elderly population depend exclusively on the Brazilian Unified Health System (SUS) [3].
Brazil has one of the highest prevalence of multimorbidity in the world, around 70%, with women and the elderly being the most affected, similar to high-income countries such as Spain and Finland. However, the Brazilian context is considered risky due to the rapid and challenging epidemiological transition [4], social inequalities, economic crisis, and democratic processes [3].
Non-communicable diseases account for 10.2% of hospitalisations among older patients. The most common NCDs are hypertension (52.2%), back problems (40.8%), high cholesterol (30.5%), cataracts (24.9%), arthritis or rheumatism (21.0%), depression (18.6%) and diabetes (15.8%), among others [1, 5].
Between 2015 and 2016, 11.6% of the elderly Brazilian population experienced at least one hospitalisation related to NCDs, including hypertension (52.2%), depression (18.6%), diabetes (15.8%), cardiovascular disease (11.7%), stroke (5.3%), and cancer (5.3%). Furthermore, 16.2% of the elderly population experienced functional limitations in performing basic activities of daily living (BADL) [3]. Four of these NCDs, including stroke, cardiovascular disease, diabetes, and hypertension, are associated with hospitalisations and are part of the Brazilian list of primary care hospitalisations sensitive to primary care. These results indicate that effective actions at the primary care level can reduce unnecessary hospitalisations among older people [3]. Brazil is ranked sixth among the countries with the highest number of people aged 20 to 79 years of age who have diabetes, with 15.7 million cases. By 2045, this number is projected to increase to 23.2 million. The hospitalisation rate for diabetes increases with age, with 56.5 hospitalisations for every 10,000 people aged 60 years or older [6].
Primary care services, including Basic Health Units (BHU) and Family Health Units (FHU), serve as the main entry point to the SUS Health Care Network (HCN). They are responsible for organising and providing the necessary care to the population according to their demands and needs, using various strategies such as clinical protocols, guidelines, and referral flows to other points of care within the HCN [7].
The co-occurrence of diabetes and depression [8, 9] can lead to poor glycaemic control [10] due to the challenges of managing both conditions with medications and non-pharmacological treatments. This can increase the risk of complications such as nephropathy, neuro- pathy, retinopathy, and cerebrovascular and cardio- vascular diseases, particularly in women and those with associated hypertension (64.2%) [11].
To maintain nurses' contributions to the health team and strengthen the leadership / caregiver relationship in primary care, it is important to assess their clinical performance. The first step is to perform an initial screening to analyse the data, identify positive factors, vulnerabilities and concerns, and determine potential nursing diagnoses [12]. The concept of nursing diagnosis proposed by NANDA-I is defined as a clinical judgment on a human response to health conditions/life processes, or a vulnerability to such a response, of an individual, a family, a group, or a community [12]. Older people with type 2 diabetes in primary care are a population at risk due to shared characteristics that make each member susceptible to a particular human response, with exposure to particular events and experiences in the face of diabetes-related conditions. This research aims to answer the following questions. What factors are associated with depression in older people with type 2 diabetes in primary care, and how can this information inform the clinical judgment of nurses to predict the risks for this group in the community?
The objective of this research is to evaluate factors associated with depression in older people with type 2 diabetes in primary care, according to the clinical nursing judgment based on NANDA-I Taxonomy II.
2. MATERIALS AND METHODS
2.1. Study Design
This was a cross-sectional observational study [13] conducted in accordance with the Guidelines for Quality and Transparency in Health Research, using the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist [14].
2.2. Population and Sample
The study population consisted of older people (60 years or older - Brazilian parameter) with type 2 diabetes who were registered in primary care units in a municipality located in the state of Paulo, Brazil. The study was carried out in the area covered by the Regional Health Department VI (DRS VI) of Bauru, SP, Brazil. The Municipal Health Department serves a population of 74,779 [15] through five BHU and six FHU, with 34,782 registered users.
To obtain the non-probabilistic sample of 389, we used the Municipal Health Department's Primary Care System database, which contained a list of type 2 diabetics organised by the health unit. The list included the following data: registration code, full name, address, and date of birth (Fig. 1).
Of the 1,585 older people with diabetes registered in this system, 1,196 were excluded and 389 were evaluated, as illustrated in Fig. (1).
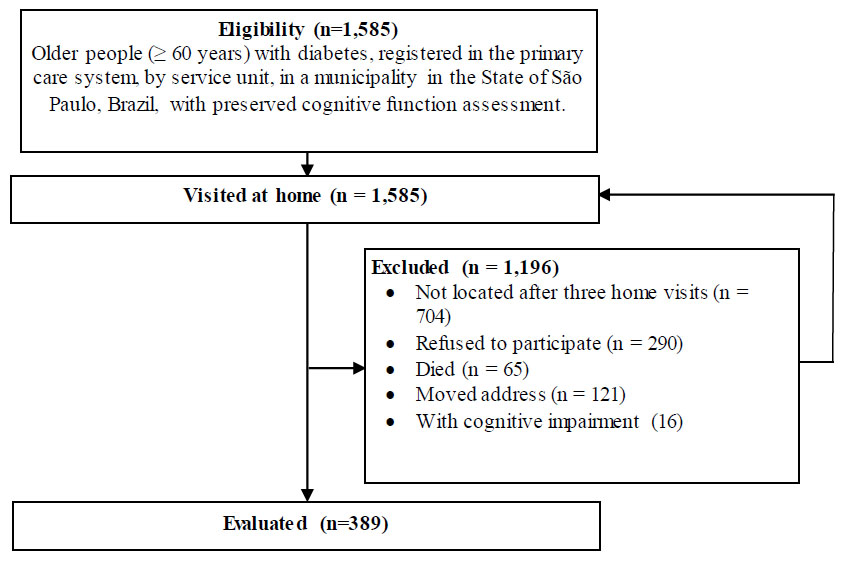
Flow chart for the design of the non-probabilistic sample of older people with type 2 diabetes, in primary care in a municipality in the state of Paulo, Brazil, from August to December 2019.
2.3. Ethical and Data Collection Procedures
Data collection occurred between August and December 2019 after obtaining approval from the CAAE Research Ethics Committee: 10027719.6.0000.5411, Opinion Number: 3.244.330. Data were collected at the participant's home after they had read and signed the informed consent form (ICF) for participation in the research. It is important to mention that before the elderly person signed the ICF, their cognitive functions were evaluated using the clock test [16], even if they had previously agreed to the terms.
Data were collected from five undergraduate nursing students who were trained and supervised by a researcher.
2.4. Exposure Variables
(A) Sociodemographic data: assigned health unit; age group (≤ 79/ ≥ 80); gender (F/M); schooling in years (≤ 4, ≥ 5); housing (owned, loaned, rented or long-term care facility); with whom they live (family, partner, alone, long-term care facility);
(B) Clinical:
(B1) Circumference in centimetres (cm) in the most prominent part of the left calf, with a non-elastic measuring tape, to assess lean mass in the elderly. Sarcopenia: for men (≤ 34 cm) and women (≤ 33 cm) [17];
(B2) Number of self-reported comorbidities (≤ 2/ ≥ 3);
(B3) Number of medications in continuous use (≤ 4/ ≥ 5) and classifications according to function and class [18];
(B4) Function of continuous use medications by systems: endocrine, cardiovascular, central nervous, and other disorders [18];
(B5) Functional performance: Brief Functional Assessment (BFA) was used, which is a multidimensional functional screening tool designed by Lachs in 1990 for use in BHU or offices by any health professional. The BFA consisted of 11 items, including questions, anthropometric measurements, and performance tests. Evaluation assessed common areas often affecting older individuals’ vision, hearing, upper and lower limb function, urinary continence, nutrition, cognition, affect, activities of daily living (ADL), instrumental activities of daily living (IADL), home environment, and social support [19]. The Lipschitz classification was adapted for the nutrition assessment [20].
(B6) Adherence to treatment was assessed by two variables:
(B6.1) Glycaemic control by biochemical test result glycated haemoglobin (HbA1c) (no ≥ 7.5% and yes < 7.5%). Glycaemic control parameters were used according to the objectives of treating elderly people with type 2 diabetes who are considered healthy [21] because 95.6% of the sample did not have multimorbidity. HBA1c is used as one of the screening or even diagnostic tests for diabetes, as well as prognostic tests for chronic complications. HbA1c levels are elevated in diabetic patients with sustained hyperglycaemia and reflect the degree of metabolic control. As HbA1c circulates within red blood cells, which have an average lifespan of 120 days, it generally reflects the state of glycemia during the previous eight to 12 weeks [22]. Therefore, the date of data collection with the patient was considered the reference point for the validity of the HbA1c result at a maximum of 12 weeks (90 days).
(B6.2) The Brief Medication Questionnaire (BMQ) is a validated instrument in the Brazilian Portuguese language that is used to assess adherence to medications. It consists of three domains: regimen, beliefs, and recall. Adherence is classified as “high”, “probably high”, “probably low”, and “low” [23]. For statistical analysis, compliance measures were regrouped as “low to probably low” and “probably high to high”.
(B7) Probability of repeated hospitalisations (Prh) is an instrument proposed by Boult et al. in 1993. It is recommended as a quick screening tool to identify people with a higher risk of frailty. The tool classifies individuals into “low”, “medium”, “medium-high”, and “high” risk categories. Prh can be administered by an administrative professional in person or remotely [24]. For statistical analysis, it was grouped into “low to medium” and “medium-high to high” categories.
2.5. Outcome Variable
Screening for depression. The 15-item Geriatric Depression Scale (GDS) was used. This is a validated instrument for the screening for depression in Brazilian Portuguese. It is easy to understand, has few response options and can be administered independently or by a trained interviewer in any healthcare setting. It is not recommended for older people with cognitive decline. The suggested cut-off point is 5/6. A total score of more than five indicates depression. All questions should be asked in the order suggested by the authors. Start by saying: “I'm going to ask you a few questions to find out how you feel during the last week” [25]?
2.6. Data Analysis
A bivariate analysis was performed in which each exposure variable was associated with the outcome. Only variables that showed an association at the p<0.20 level were included in a multiple logistic regression model. The analyses were carried out using EpiInfo software version 7.
The collected data were entered into an Excel spreadsheet and before model adjustment, an exploratory analysis was carried out to locate outliers that would deserve revisions.
3. RESULTS
3.1. Descriptive Analysis
The study analysed a sample of 389 older people with type 2 diabetes attended by primary care in a municipality in the state of São Paulo, Brazil. Of the total sample, 54% came from communities assigned to the FHU and 46% to the BHU. Most of the samples were women (66.1%) and had less than or equal to four years of schooling (90.3%). Furthermore, 85.9% of the sample owned their own home and, 56.0% lived with their family, while 28.3% lived with their partner and 1.0% lived in a long-term care facility (Table 1).
| Variables | Categories | N. | % |
|---|---|---|---|
| Older people, according to the primary care service model (n = 389) | Family Health Units (FHU) | 210 | 54.0 |
| Basic Health Units (BHU) | 179 | 46.0 | |
| Age (in years) (n =389) | ≤ 79 | 333 | 85.6 |
| ≥ 80 | 56 | 14.4 | |
| Sex (n = 389) | Female | 257 | 66.1 |
| Male | 132 | 33.9 | |
| Schooling (in years) (n = 382) | ≤ 4 | 345 | 90.3 |
| ≥ 5 | 37 | 9.7 | |
| Housing (n = 389) | Owned | 334 | 85.9 |
| Loaned | 27 | 6.9 | |
| Rented | 24 | 6.2 | |
| Long-term care facility | 4 | 1.0 | |
| Co-residents (n = 389) | Family | 218 | 56.0 |
| Partner | 110 | 28.3 | |
| Alone | 57 | 14.7 | |
| Long-term care facility | 4 | 1.0 | |
| BFA1. Vision: vision acuity with lenses, assessed with a Jaeger card [ 19 ] (n=389) | No | 64 | 16.5 |
| Yes | 325 | 83.5 | |
| BFA2. Hearing: hearing acuity in whisper test “What is your name?” whisper test [ 19 ] (n=389) | No | 39 | 10.0 |
| Yes | 350 | 90.0 | |
| BFA3.Urinary incontinence: leakage of urine through underwear [ 19 ] (n=389) | No | 288 | 74.0 |
| Yes | 101 | 26.0 | |
| BFA4.AVD/AIVD: can get up, dress, prepare meals and do the shopping without help [ 19 ] (n=389) | No | 30 | 7.7 |
| Yes | 359 | 92.3 | |
| BFA5. Arm: function of arms when touching hands to the back of the head and picking up a spoon [ 19 ] (n=389) | No | 13 | 3.3 |
| Yes | 376 | 96.7 | |
| BFA6. Leg: ability to stand up and walk for three metres, returning to the chair in ≤ 12 seconds [ 19 ] (n=389) | No | 111 | 28.5 |
| Yes | 278 | 71.5 | |
| BFA7. Nutrition [ 19 ]: adapted to Lipschitz classification [ 20 ] (n=387) | Underweight (BMI < 22) | 27 | 7.0 |
| Eutrophic (BMI 22 to <2 7) | 138 | 36.0 | |
| Overweight/Obesity (BMI) > 27 | 221 | 57.0 | |
| BFA8. Mental state: ability to memorise three words and repeat them after one minute [ 19 ] (n=389) | No | 180 | 46.3 |
| Yes | 209 | 53.7 | |
| BFA9. Depression: assessed by the answer to the question: Do you often feel sad or depressed [ 19 ]? (n=389) | No | 215 | 55.3 |
| Yes | 174 | 44.7 | |
| BFA10. Home environment: with a risk of falling, such as difficulties with stairs, the presence of a bathtub, poor lighting, and the use of carpets [ 19 ] (n=389) | No | 257 | 66.1 |
| Yes | 132 | 33.9 | |
| BFA11. Social support: perception of being able to depend on someone in case of urgency/emergency or illness [ 19 ] (n=389) | No | 54 | 13.9 |
| Yes | 335 | 86.1 | |
| Circumference in centimetres at the most prominent part of the left calf [ 17 ] (n=341) | (Normal) Male ≥ 35; Female ≥ 34 | 305 | 89.2 |
| (Sarcopenia) Male ≤ 34; Female ≤ 33 | 37 | 10.8 | |
| Number of comorbidities (n=389) | ≤ 2 | 372 | 95.6 |
| ≥ 3 | 17 | 4.4 | |
| Main comorbidities reported (n=421) | Hypertension | 280 | 66.5 |
| Dyslipidaemia | 18 | 4.3 | |
| Cardiovascular disease | 30 | 7.1 | |
| Nephropathies | 9 | 2.1 | |
| Osteoarticular diseases | 11 | 2.6 | |
| Cerebrovascular diseases | 12 | 2.8 | |
| Other diseases | 61 | 14.5 | |
| Glycaemic control by HbA1c [ 21 ] (n=142) | No (HbA1c >7,5%) | 77 | 54.2 |
| Yes (HbA1c ≤ 7,5%) | 65 | 45.8 | |
| Probability of repeated hospitalisations (Prh) [ 24 ] (older people at increased risk of frailty) (n=389) | “Low to Medium” | 319 | 82.2 |
| “Medium-High to High” | 69 | 17.8 | |
| Number of ongoing medications reported (n=386) | ≤ 4 | 378 | 97.4 |
| ≥ 5 | 10 | 2.6 | |
| Screening for depression by GDS [ 25 ](n = 389) | No | 287 | 73.8 |
| Yes | 102 | 26.2 | |
| Medication adherence by BMQ [ 23 ] (n=389) | “Low to probably low” | 82 | 21.1 |
| “Adherence to probably high” | 307 | 78.9 | |
| Function of medicines for continuous use [ 18 ] (n=791) | Endocrine system | 571 | 72.4 |
| Cardiovascular system | 205 | 26.0 | |
| Central nervous system | 10 | 1.3 | |
| For other disorders | 3 | 0.3 |
Hypertension is the most frequently reported comorbidity (66.5%), followed by cardiovascular disease (7.1%) and dyslipidaemias (4.3%). Regarding comorbi- dities, 95.6% had two and took continuous medication (97.4%), most of which was for the endocrine system (72.4%), specifically antidiabetics (70.5%). There were 78.9% with a “probably high to high” adherence to medication treatment, but 54.2% had parameters that indicated uncontrolled glycemia (HbA1c, 5%). Regarding the assessment of the likelihood of repeated hospitalisations among older people at increased risk of frailty, 82.2% were classified as “low to medium” and 17.8% as “medium-high to high” (Table 1).
Only 30.8% of the elderly had laboratory results for glycaemic control recorded in the medical records of primary care units.
Upon initial analysis of the data, which refers to the 11 domains that predominantly affect or interfere with the daily activities of the elderly, it is evident that the majority of the population has preserved functional domains for vision (83.5%) and hearing (90%). The study found high rates of AVD/AIVD (92.3%), arm function (96.7%), and perceived social support (86.1%). Urinary continence was reported in 74% of the participants, while 71.5% had good leg function. The mental state of memorisation was reported in 53.7% of the participants and 55.3% had no depression. Furthermore, 66.1% of the participants reported having a safe home environment for falls (Table 1).
On closer analysis of the data, it becomes apparent that only two elderly individuals had all functional dimensions preserved for the BFA. Furthermore, 57.1% of the participants had altered nutritional status due to overweight/obesity, while 89.2% had preserved the estimated lean mass assessed by the circumference of the left calf. The BFA instrument indicated that 44.7% of the participants exhibited manifestations of depression, often verbalising feelings of sadness or depression. The GDS represented a lower percentage, at 26.2%. The percentage of individuals with mental state deficit, indicated by their inability to memorise and repeat three words after one minute, was 46.3% (Table 1).
Although the BFA instrument detected depression in 44.7% and GDS in 26.2% of these elderly people, the classes of continuous use drugs mentioned the least frequently were antidepressants (0.6%) and anxiolytics and hypnotics (0.4%) (Table 1).
|
Sociodemographic Variables and Functional and Multidimensional Performance by Brief Functional Assessment*
(exposure variables) |
Geriatric Depression Scale - GDS† Outcome n=389 |
p-value and Odds Ratio (OR) | |||||
|---|---|---|---|---|---|---|---|
| No (n=287) | Yes (n=102) | TOTAL | |||||
| N. | % | N. | % | N. | % | ||
| Older people according to the primary care service model (n = 389) | - | - | - | - | - | - | - |
| Family Health Units (FHU) | 140 | 78.2 | 39 | 22.0 | 179 | 100.0 | p=0.07‡ (ns) |
| Basic Health Units (BHU) | 147 | 70.0 | 63 | 30.0 | 210 | 100.0 | |
| Age group (in years) (n. 389) | - | - | - | - | - | - | - |
| ≤ 79 | 251 | 75.4 | 82 | 24.6 | 333 | 100.0 | p=0.08‡(ns) |
| ≥ 80 | 36 | 64.3 | 20 | 35.7 | 56 | 100.0 | |
| Sex (n. 389) | - | - | - | - | - | - | - |
| Female | 184 | 71.6 | 73 | 28.4 | 257 | 100.0 | p=0.17‡ (ns) |
| Male | 103 | 78.0 | 29 | 22.0 | 132 | 100.0 | |
| Schooling (in years) (n. 382) | - | - | - | - | - | - | - |
| ≤ 4 | 250 | 72.5 | 95 | 27.5 | 345 | 100.0 | p=0.03‡ (s) OR=0.32(IC=95%:0.11-0.92) |
| ≥ 5 | 33 | 89.2 | 4 | 10.8 | 37 | 100.0 | |
| Housing (n = 389) | - | - | - | - | - | - | - |
| Owned | 248 | 74.3 | 86 | 25.7 | 334 | 100.0 | p=0.31§ (ns) |
| Loaned | 22 | 81.5 | 5 | 18.5 | 27 | 100.0 | |
| Rented | 15 | 62.5 | 9 | 37.5 | 24 | 100.0 | |
| Long-term care facility | 2 | 50.0 | 2 | 50.0 | 4 | 100.0 | |
| Co-residents (n=389) | - | - | - | - | - | - | - |
| Family | 151 | 69.3 | 67 | 30.7 | 218 | 100.0 | p=0.06 ‡ (ns) |
| Partner | 90 | 81.8 | 20 | 18.2 | 110 | 100.0 | |
| Alone | 44 | 77.2 | 13 | 22.8 | 57 | 100.0 | |
| Long-term care facility | 2 | 50.0 | 2 | 50.0 | 4 | 100.0 | |
| BFA 1. Vision [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 45 | 70.3 | 19 | 29.7 | 64 | 100.0 | p=0.49‡ (ns) |
| Yes | 242 | 74.5 | 83 | 25.5 | 325 | 100.0 | |
| BFA 2. Hearing [ 19 ](n = 389) | - | - | - | - | - | - | - |
| No | 30 | 76.9 | 9 | 23.1 | 39 | 100.0 | p=0.63‡ (ns) |
| Yes | 257 | 73.4 | 93 | 26.6 | 350 | 100.0 | |
| BFA 3. Urinary incontinence [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 224 | 77.8 | 64 | 22.2 | 288 | 100.0 | p<0.01‡ (s) OR=2.11(IC=95%:1.30-3.44) |
| Yes | 63 | 62.4 | 38 | 37.6 | 101 | 100.0 | |
| BFA 4. ADL / IADL [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 16 | 53.3 | 14 | 46.7 | 30 | 100.0 | p<0,01‡ (s) OR=0.37 (IC=95%:0.17-0.79) |
| Yes | 271 | 75.5 | 88 | 24.5 | 359 | 100.0 | |
| BFA 5. Arm function [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 7 | 53.8 | 6 | 46.2 | 13 | 100.0 | p=0.03‡ (s) OR=0.32(IC=95%:0.11-0.92) |
| Yes | 280 | 74.5 | 96 | 25.5 | 376 | 100.0 | |
| BFA 6 Leg function [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 79 | 71.2 | 32 | 28.8 | 111 | 100.0 | p=0.09‡ (ns) |
| Yes | 208 | 74.8 | 70 | 25.2 | 278 | 100.0 | |
| BFA 7. Nutrition [ 19 ]: adapted to the Lipschitz classification [ 20 ] (n = 386) | - | - | - | - | - | - | - |
| Underweight (BMI < 22) | 18 | 66.7 | 9 | 33.3 | 27 | 100.0 | p=0.97§ (ns) |
| Eutrophic (BMI 22 to <2 7) | 105 | 76.1 | 33 | 23.9 | 138 | 100.0 | |
| Overweight/Obesity (BMI) > 27 | 163 | 73.8 | 58 | 26.2 | 221 | 100.0 | |
| BFA 8. Mental state [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 129 | 71.7 | 51 | 28.3 | 180 | 100.0 | p=0.38‡ (ns) |
| Yes | 158 | 75.6 | 51 | 24.4 | 209 | 100.0 | |
| BFA 9. Depression [ 25 ] (n = 389) | - | - | - | - | - | - | - |
| No | 183 | 85.1 | 32 | 14.9 | 215 | 100.0 | p< 0.01‡ (s) OR=3.84(IC=95%:2.37-6.23) |
| Yes | 104 | 59.8 | 70 | 40.2 | 174 | 100.0 | |
| BFA 10. Home environment at risk of falls [ 19 ] (n. 389) | - | - | - | - | - | - | - |
| No | 203 | 79.0 | 54 | 21.0 | 257 | 100.0 | p<0.01‡ (s) OR=2.15(IC=95%:1.35-3.42) |
| Yes | 84 | 63.6 | 48 | 36.4 | 132 | 100.0 | |
| BFA 11. Social support [ 19 ] (n = 389) | - | - | - | - | - | - | - |
| No | 248 | 74.2 | 86 | 25.8 | 334 | 100.0 | p=0.60‡ (ns) |
| Yes | 39 | 70.9 | 16 | 29.1 | 55 | 100.0 | |
| Circumference in centimetres in the most prominent part of the left calf [ 17 ] (n =342) | - | - | - | - | - | - | - |
| (Normal) Male ≥ 35; Female ≥ 34 | 243 | 76.2 | 76 | 23.8 | 319 | 100.0 | p=0.48‡ (ns) |
| (Sarcopenia) Male ≤ 34; Female ≤ 33 | 19 | 82.6 | 4 | 17.4 | 23 | 100.0 | |
| Adherence to medication by BMQ [ 23 ] (n =389) | - | - | - | - | - | - | - |
| “Adherence to probable high” | 238 | 77.5 | 69 | 22.5 | 307 | 100.0 | p<0.01‡ (s) OR=2.32(IC=95%:1.39-3.39) |
| “Low to probable low” | 49 | 59.8 | 33 | 40.2 | 82 | 100.0 | |
| Glycaemic control by HbA1c [ 21 ], (n = 142) | - | - | - | - | - | - | - |
| Yes (HbA1c ≤ 7,5) | 45 | 69.2 | 20 | 30.8 | 65 | 100.0 | p=0.23‡ (ns) |
| No (HbA1c > 7,5) | 60 | 67.9 | 17 | 22.1 | 77 | 100.0 | |
| Number of reported comorbidities (n = 389) | - | - | - | - | - | - | - |
| ≤ 2 | 208 | 74.5 | 71 | 25.5 | 279 | 100.0 | p=0.58‡ (ns) |
| ≥ 3 | 79 | 71.8 | 31 | 28.2 | 110 | 100.0 | |
| Number of continuous medications (n = 388) | - | - | - | - | - | - | - |
| ≤ 4 | 281 | 74.3 | 97 | 25.7 | 378 | 100.0 | p=0.08‡ (ns) |
| ≥ 5 | 5 | 50.0 | 5 | 50.0 | 10 | 100.0 | |
| Probability of repeated hospitalisations (Prh) [ 24 ] (elderly at higher risk of frailty) (n=389) | - | - | - | - | - | - | - |
| “Low to medium” | 249 | 78.1 | 70 | 21.9 | 319 | 100.0 | p<0,01‡ (s) OR=2.90(IC=95%:1.68-5.00) |
| “Medium-high to high” | 38 | 55.1 | 31 | 44.9 | 69 | 100.0 | |
3.2. Bivariate Analysis
Table 2 shows that eight exposure variables were associated with the outcome of the depression screening in older people with type 2 diabetes in primary care, three providing protection and five increasing the risk.
Protective variables were:
(a) ≥ 5 years of schooling (p=0.03), in 68% (OR = 0.32 [95% CI: 0.11-0.92]);
(b) maintenance of ADL/IADL (p<0.01), in 63% (OR = 0.37 [95% CI: 0.17-0.79]);
(c) maintenance of arm function (p=0.03), in 68% (OR = 0.32 [95% CI: 0.11-0.92]).
The variables that were found to increase the risk were:
(d) suffering from urinary incontinence (p<0.01), increases 2.1 times (OR = 2.11 [95% CI: 1.30-3.44]);
(e) having depression detected by BFA (p<0.01), increases the chances of it being confirmed by GDS 3.8 times (OR = 3.84 [95% CI: 2.37-6.23]);
(f) living in a home environment with risks of mobility and falls, such as difficulty on stairs, the presence of a bathtub, poor lighting and the use of carpets (p<0.01), exposes the elderly person 2.1 times (OR = 2.15 [95% CI 1.35-3.42]);
(g) having “low to probable low” adherence to medication adherence (p<0.01), i.e., poor compliance to medication treatment increases the chance of depression 2.3 times (OR = 2.32 [95% CI 1.39-3.39]);
(h) being rated as “medium high to high” Prh (p<0.01) increases the chance of depression approximately three times.
3.3. Multiple Logistic Regression Analysis
Twelve variables were inserted into a multiple logistic regression model (Table 3). The seven exposure variables that were statistically associated with the outcome of the GDS depression screening were schooling, urinary incontinence, AVD/AIVD, arm function, home environment for falls, adherence to BMQ drug treatment, and Prh. Furthermore, five other variables showed a p<0.20 association: elderly according to service models in primary care, age group, sex, leg function, and number of continuous prescription medications.
It is important to mention that the AFB9-based depression evaluation variable was not included in the model to avoid confusion. This is because the outcome variable, GDS-screened depression, is considered the gold standard for this purpose.
The analysis indicates that older people with adherence “low to probable low” evaluated by BMQ (p=0.01) are twice as likely to be tested for depression (OR = 2.17 [95% CI: 1.21 - 3.88]) compared to those with medium to high Prh (p<0.01). The latter group consists of older people with a higher risk of frailty and are 2.7 times more likely to be tested for depression (OR = 2.68 [95% CI: 1.42 - 5.04]) (Table 3).
4. DISCUSSION
This research identified predictive factors that promote depression in older people with type 2 diabetes in the community. The study paid particular attention to poor adherence to medications and older people assessed to have a higher risk of frailty (medium-high to high Pir).
Analysis of these factors for depression in older people, in the context of NANDA-I Nursing Diagnoses Taxonomy II [12], involves a process that begins with an initial assessment, also known as screening or screening of the risk population in primary care, for older people with type 2 diabetes (Fig. 2).
Poor compliance with medication treatment has been identified as a factor that increases the risk of depression in people with diabetes (diabetics) [26, 27]. Systematic reviews have highlighted the high prevalence of depression in people with diabetes [8, 9] that is associated with poor glycaemic control [10, 26] resulting from the difficulty of following recommendations such as diet, regular exercise, self-monitoring glycaemic, and drug treatment. This context suggests that people with depression may be more likely to have low adherence to diabetes treatment, which can increase their vulnerability to comorbidities such as nephropathy, neuropathy, retinopathy, cerebrovascular, and cardiovascular diseases. This is particularly true for women and those with associated hypertension (64.2%) [11, 28].
| Variables | Odds Ratio | 95% CI | P-value* | |
|---|---|---|---|---|
| Primary care service models: basic health unit (bhu)/family health unit (fhu) (fhu reference) | 0.71 | 0.40 | 1.26 | 0.24 |
| Schooling (in years): ≤4/≥5 (reference “≥5”) | 2.70 | 0.86 | 8.42 | 0.09 |
| Age (in years): ≤79/≥80 (reference “≤79”) | 1.20 | 0.60 | 2.41 | 0.60 |
| Sex: m/f (reference “f”) | 0.68 | 0.39 | 1.18 | 0.17 |
| Medications for continuous use: ≤4/≥5 (reference “≤4”) | 1.79 | 0.44 | 7.39 | 0.42 |
| Medication adherence by bmq [23]: “low-probably low”/“probably high-high” (reference “probably high-high”) | 2.17 | 1.21 | 3.88 | 0.01 |
| Probability of repeat hospitalisations (prh) (older people with a higher risk of frailty) [24]: “low to medium”/“medium-high to high” (reference “low to medium”) | 2.68 | 1.42 | 5.04 | <0.01 |
| Bfa3. Urinary incontinence [19]: yes/no (reference “no”) | 1.46 | 0.82 | 2.60 | 0.20 |
| Bfa4. Avd/aivd [19]: yes/no (reference “yes”) | 1.53 | 0.62 | 3.81 | 0.36 |
| Bfa5. Arm function [19]: yes/no (reference “yes”) | 1.08 | 0.28 | 4.08 | 0.91 |
| Bfa6. Leg function [19]: yes/no (reference “yes”) | 0.63 | 0.33 | 1.18 | 0.15 |
| Bfa10. Home environment at risk of falls [19]: yes/no (reference “no”) | 1.50 | 0.88 | 2.55 | 0.14 |
| Constant | -- | -- | -- | <0.01 |
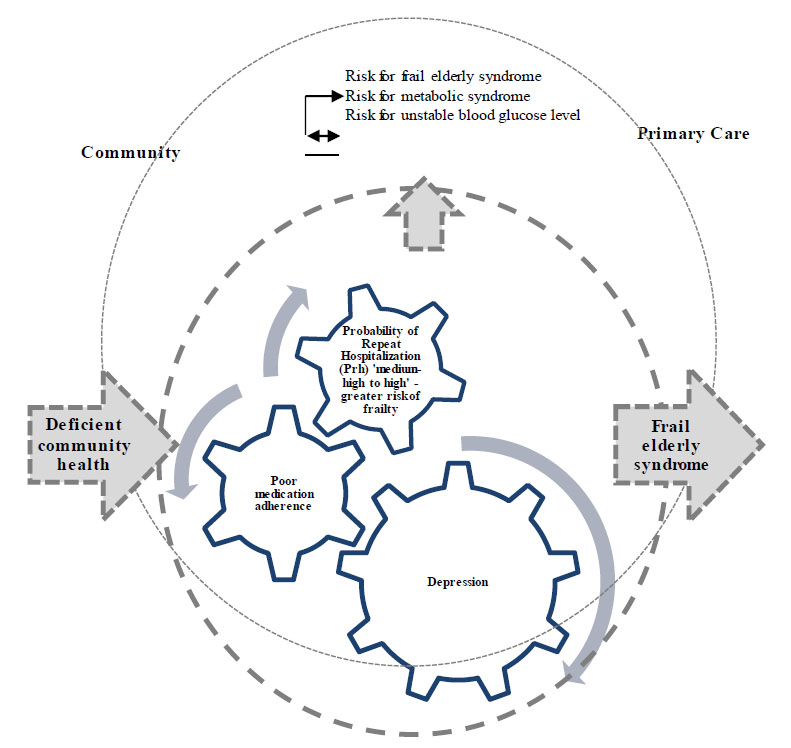
From deficient community health, related to the failure of a type 2 diabetes harm reduction programme, to frail elderly syndrome in primary care: depression as an intervening component, promoted by poor compliance with medication treatment and the probability of repeated hospitalisation (Prh). Primary care services in a city in the state of São Paulo, 2021.
It should be noted that there has been little research on the longitudinal association between HbA1c and depressive symptoms. However, population cohort follow-ups have found that high concentrations of HbA1c are associated with an increased risk of depressive symptoms [29].
In this study, 40.2% of elderly type 2 diabetics with low probable adherence to drug treatment were tested for depression by GDS, increasing the probability of mental health comorbidity by 1.7 times.
In this context, the nursing diagnostic hypothesis (NDH) [30] was that these elderly people are at risk for unstable blood glucose levels due to the lack of adherence to the diabetes control plan. This is evidenced by poor adherence to medications and is associated with depression, as identified by GDS (Fig. 2).
When clinically evaluating elderly type 2 diabetics, it is recommended to assess their overall health and individual glycaemic values before establishing treatment goals and strategies. These practices categorise procedures into three groups: (a) general health assessment, which includes functional assessment (ADL and IADL), depression, memory, risk of falls, nutritional status according to BMI, blood pressure (BP), tobacco use, alcohol use, review of drug treatment, cancer assessment, hearing, conditions for comorbidities, visual acuity and physical fitness/fitness; (b) general health examinations. The following health screenings are recommended: Electrocardiogram (ECG), lipid profile, bone density, and ultrasound for abdominal aortic aneurysm. For non-diabetics, diabetes screening is also recommended. For people with diabetes, it is important to monitor retinopathy, nephropathy, and neuropathy. Nutrition therapy and diabetes management training are also important aspects of diabetes-specific health [31].
As part of the clinical and individual evaluation of the elderly, screening for depression, reviewing drug treatment, and assessing physical fitness are necessary to prevent disease complications. Metrics related to glycaemic control are obtained to assess the effectiveness of the evaluation. Additionally, dysglycemia can cause macrovascular and microvascular diseases, which can increase mortality rates, reduce quality of life, and increase treatment costs. It is important to note that these complications are objective and supported by evidence [32].
Dysglycemia creates an oxidative and inflammatory metabolic environment that can cause intravascular complications in diabetics, affecting the vessels, kidneys, heart, eyes, and neurological system [21]. This process is known as the toxic effect of hyperglycaemia [29]. Therefore, investing in glycaemic control strategies is crucial to reducing the morbidity and mortality of diabetes.
The second NDH concerns deficient community health, which is related to the failure of the diabetes harm reduction programme. This is evidenced by the fact that 40.2% of the elderly have poor adherence to medications, which is associated with GDS-tested depression (Fig. 2). Antidepressants, as a continuous pharmacological class of use, were less frequently mentioned by elderly evaluated (0.6%), suggesting that depression may not have been adequately evaluated and treated.
Health professionals face the challenge of ensuring that the user adheres to the diabetes treatment. It is important that they assess the risks of nonadherence, develop strategies to facilitate medication use, and provide ongoing support and adherence assessment at each consultation [33].
Continuous evaluation is justified, particularly in the presence of dysglycemia, as this population is at risk of low health literacy due to low levels of education. Furthermore, most people who do not adhere to drug treatment have depression and cognitive impairment and, therefore, need the supervision of a caregiver for drug treatment [27].
Studies on factors related to nonadherence to drug treatment by elderly diabetics are limited. However, available studies report low adherence rates (27.3%) [34] and suggest that disbelief in the effectiveness of drugs used to control the disease [33, 34], the type of medication prescribed (with patients prescribed insulin at increased risk of nonadherence) [27], and intolerance to the volume or frequency of the medication are associated with nonadherence [33].
During each consultation, it is crucial to identify the factors or risks that contribute to nonadherence to medication treatment among elderly diabetic patients. This information is necessary to tailor interventions and assess the individual's ability to manage his condition, with the ultimate goal of achieving glycaemic control. It is insufficient to simply prescribe medications without considering the patient's autonomy and the ability to adhere to the treatment plan.
Clinical trials have demonstrated the effectiveness of interventions aimed at improving medication adherence in elderly diabetic patients. These interventions include telephone-based interventions, pharmacist participation, educational processes, and case management [33].
Recent research suggests that regular antidepressants should be prescribed medically to elderly people with depression and diabetes. This is because they reduce the risk of macrovascular complications and all-cause mortality. Selective serotonin reuptake inhibitors (SSRI) or tricyclic/tetracyclic antidepressants are recommended. It is important to note that this recommendation is based on objective research findings and not subjective evaluations [35].
Referring to the model presented in Fig. (2), it is necessary to structure and operationalise a line of care for elderly diabetics in the evaluated PHC. This will break the cyclical subprocess that promotes depression and increase adherence to older people's medications. As a result, better glycaemic control will be achieved, reducing emergency service visits, hospitalisations, and costs. Furthermore, the risk of frail elderly syndrome will be mitigated. The term “dynamic state of unstable equilibrium” refers to the vulnerability of elderly individuals who experience deterioration in one or more health domains (physical, functional, psychological, or social), which can lead to adverse health effects, particularly disability. This is a nursing diagnosis related to Class 2 in Domain 1 - Health Promotion and, therefore, requires interventions at the PCH level [30].
Finally, identifying the prevalence of frailty and the factors associated with it can help implement appropriate interventions early to improve the quality of life of older people by reducing the damage caused by diabetes [36].
5. STUDY LIMITATIONS
Limitations include that due to the relatively high prevalence of the outcome, some estimates may be overestimated by adjusting a logistic regression model. Furthermore, the unknown pattern of occurrence of missing data may contribute to some extent to the existence of systematic information error. Another limitation is related to the fact that the study sample was non-probabilistic, which requires cautious generalisation.
6. CONTRIBUTIONS TO NURSING, HEALTH CARE, AND PUBLIC POLICY
This research indicates the need to strengthen primary care so that community health nurses can carry out their role in mitigating the adverse effects of type 2 diabetes in the elderly. Lack of community health care can lead to a failure to detect depression and poor compliance with disease treatment, increasing the risk of unstable blood glucose levels, metabolic syndrome, subsequent frailty, and early mortality in the elderly population.
The findings of this study indicate the need to alleviate the psychological burden associated with depression among older people with type 2 diabetes in the context of primary care and the community. It is imperative to extend the scope of psychosocial intervention and shared tasks within collaborative care to improve the recovery of this demographic. In this regard, a low-intensity psychosocial intervention, primarily conducted by non-mental health professionals, has demonstrated remarkable efficacy in facilitating recovery from depression among elderly Brazilians. The authors advocated for the intervention, as it requires minimal resources to narrow the disparity in depression treatment among the elderly in other low- and middle-income countries [37].
CONCLUSION
Poor adherence to medications increases the risk of depression, as evaluated by GDS twice, in older people with diabetes in primary care in a municipality in the state of São Paulo, Brazil.
During the screening process for risk factors associated with depression in older people, it was observed that older people with type 2 diabetes in primary care with EDH were at risk for unstable blood glucose levels due to poor adherence to medications in their diabetes control plan. This was evidenced by 40.2% of the elderly who exhibited poor adherence to medications.
These conditions can increase the risk for frail elderly syndrome due to the deficient community health services. Specifically, the primary care programme that addresses type 2 diabetes is incomplete and may not fully prevent related health problems.
Primary care must implement a care pathway based on best practices for the clinical assessment of older patients with diabetes. This will provide community nurses with the necessary working conditions to exercise clinical judgment, supported by NANDA-I Taxonomy II.
It is of the utmost importance to expand the scope of psychosocial intervention and shared tasks within collaborative care to improve the mental health of this older demographic.
AUTHORS’ CONTRIBUTION
The authors confirm their contribution to the paper as follows: HRN, GCB, SMB; study conception and design: HAM; data collection: EAS; data analysis and interpretation of results. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ADL | = Activities of daily living |
| BFA | = Brief Functional Assessment |
| BHU | = Basic health units |
| HCN | = Health Care Network |
| BMQ | = Brief Medication Questionnaire |
| BP | = Blood pressure |
| FHU | = Family Health Units |
| GDS | = Geriatric Depression Scale |
| HBA1c | = Glycated haemoglobin |
| IADL | = Instrumental activities of daily living |
| NCDs | = Noncommunicable diseases |
| NDH | = Nursing diagnostic hypothesis |
| OR | = Odds ratio |
| Prh | = Probability of Repeated Hospitalisations |
| STROBE | = Strengthening the Reporting of Observational Studies in Epidemiology |
| SUS | = Unified Health System from Brazil |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was evaluated and approved by the Research Ethics Committee of the Botucatu Medical School, UNESP, Brazil, under CAAE 10027719.6. 0000.5411 and opinion: 3.224.330
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Data were collected after the research participants signed the informed consent form.
AVAILABILITY OF DATA AND MATERIALS
The database for this research is with the authors and, if necessary, they can make it available on request. This article is the result of a doctoral thesis defended at the Postgraduate Postgraduate Academic Programme in Nursing, São Paulo State University (Unesp), Botucatu Medical School. Thesis deposited in the UNESP repository, link: https://repositorio.unesp.br/items/ a6294 e54-9a78-468e-8e0d-533e562538d7


