All published articles of this journal are available on ScienceDirect.
Role of the Nursing Professional in Euthanasia: A Qualitative Systematic Review
Abstract
Background
Until the date of the search, Euthanasia was legally accepted in 5 countries: the Netherlands, Belgium, Luxembourg, Canada and Colombia.
Objective
We aimed to identify the role of nurses in euthanasia based on articles published both nationally and internationally between 2014 and 2022.
Methods
Qualitative and quantitative studies, editorials, literature reviews and Colombian regulations were included. Publications that did not meet the criteria of the Strengthening the Reporting of Observational Studies in Epidemiology statement and the Spanish Critical Appraisal Skills Programme were excluded. In total, 57 articles were evaluated and 19 were selected. Appropriate copyright principles were followed in accordance with Colombian Law 23 of 1982.
Results
With the data obtained, 4 thematic categories were developed as follows: reception and management of euthanasia requests and regulations in Colombia; emotional accompaniment and effective communication with the patient and family; participation in euthanasia preparations and administration of medications; and management of requests and administration of medications.
Conclusion
Nursing plays an important role in the care of the patient requesting euthanasia, from the reception and management of the request to the administration of the lethal drugs.
1. INTRODUCTION
Euthanasia is defined as “the administration of lethal drugs by a physician with the specific intention of ending the life of a patient at the explicit request of the patient” [1]. Currently, this practice is legally performed only in five countries: the Netherlands, Belgium, Luxembourg, Canada, and Colombia [2]. Of these, Colombia is protected under Resolution 1216 of 2015, that legalizes euthanasia under the right of dignified and voluntary death to all individuals with autonomy and decision criteria and having an incurable or terminal illness, excluding the pediatric population aged <6 years and individuals with mental disorders [3]. The countries that continue to reprimand this procedure believe that this practice defies the professional oath and bioethical convictions [2] of the healthcare personnel involved, such as medical, nursing, psychology, physiotherapy, occupational therapy and pharmacy professionals [4].
Euthanasia is a controversial topic of discussion because of the meaning of this term and its perception. This practice in healthcare requires healthcare professionals to inform themselves and make use of conscientious objection, which is considered the right of a physician or any healthcare personnel to refuse to perform the deliberate act of ending the life of a patient who requests it in accordance with the law because they consider that such an act is against their ethical, moral, philosophical and religious convictions and that performing this act would significantly damage their conscience and moral integrity [2]. In this regard, conscientious objection arises as a legal right resource and protection mechanism for healthcare professionals who disagree with the implementation of this practice because their objection is owing to an affectation to their conscience. Healthcare professionals should not be pressured by the state or their colleagues. On the contrary, they should be free to express their thoughts and points of view [5].
Considering this subject and taking into account that the nursing professional is fundamental for the application of euthanasia, the literature reflects differences in the attitude toward this intervention according to the presence of the thematic content in the training process. A study conducted in Israel among 210 individuals, including 120 nursing students, showed that almost one-third of them were against euthanasia based on religious grounds and less than half were neutral regarding the subject. This research concluded that nursing students may change their attitude toward euthanasia from negative to positive after gaining clinical experience because it is strongly influenced by their exposure to terminally ill patients [1].
By contrast, another study conducted in Turkey involving 300 nursing students in their fourth year of training concluded that 97.7% of them were aware about euthanasia and 88.7% stated that they had received this information at the university. Furthermore, 34% of the students reported that euthanasia is morally correct, although it is legally prohibited in that country. This shows that teaching the concept of euthanasia during the training stage strengthens the critical and autonomous thinking of students, which will then serve them during their professional stage [6].
The role of nursing professionals is vital in the care of patients requesting euthanasia because their presence and assistance are necessary during drug administration; moreover, these professionals provide emotional and psychological support to the patient and family, which are holistic and humanized actions performed by them as part of comprehensive healthcare services. However, the role and willingness of nursing professionals to participate in this practice varies according to the country and department where they are employed [7]. Therefore, the objective of the present review is to identify the role of nursing professionals in euthanasia based on the articles published between 2014 and 2022 and to provide information that benefits professionals and students in training so that they have additional tools if they are confronted with a request for euthanasia during the provision of their healthcare services.
2. MATERIALS AND METHODS
2.1. Systematic Literature Search
A qualitative systematic review was conducted between May and October 2022 by including articles from the following databases: SAGE Journals, Springer Link, Science Direct, Scopus and Dialnet. The review was conducted to answer the following research question defined with the PICO (participant, interventions, comparators, outcomes) method: what is the role of the nursing professional in euthanasia? (Table S1). The following key terms were used: nursing, nursing student and euthanasia; these terms were previously verified in the Health Sciences Descriptors—DeCS library. Other keywords such as dignified death, nursing role and conscientious objection were also applied because they generated better search results. In addition, the Boolean operator (AND) was used to create the following search equations: [(euthanasia) AND (nursing) AND (conscien- tious objection)], [(euthanasia) AND (dignified death) AND (nurse’s role)] and [(Students Nursing) AND (euthanasia) AND (conscientious objection)] (Table S2). This systematic review was registered in PROSPERO - Prospective International Register of Systematic Reviews under the registration number CRD42022362848.
2.2. Inclusion and Exclusion Criteria
Qualitative and quantitative studies, editorial articles and literature review articles published between 2014 and 2022 in English and Spanish, as well as the current Colombian regulations on the subject, were included. These publications were included because the scientific research on the topic discussed is recent and these are the types of publications in which the topic is subsequently interpreted via theoretical approaches by comparing articles of this nature with research articles. Under- graduate theses that were not in accordance with the research question or objective and studies that did not comply with the scientific stringency of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for observational or cross-sectional studies and the Critical Appraisal Skills Programme Español (CASPe) for literature reviews and qualitative studies were excluded.
2.3. Data Collection and Analysis
First phase: A search was conducted for articles in the databases selected according to the research objective and selection criteria. Second phase: The selected articles were critically reviewed to evaluate the methodological stringency of each type of design, except for editorial articles, based on the CASPe tools for qualitative studies and literature reviews and the STROBE format for observational or cross-sectional studies. The selection of articles for analysis is depicted in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram - PRISMA (Fig. 1). Third phase: The information was recorded in a database prepared using Microsoft Excel where the following data of the selected articles were included: bibliographic reference, country and year of publication, database, study objective, methodology, and main results (Table 1). Fourth phase: Considering the objective of the present systematic review, the evaluation, analysis and interpretation of the content of the articles was performed, following which the articles were grouped according to the thematic categories developed in the studies.
2.4. Ethical Aspects
The investigation follows the principles of the Helsinki Declaration, which designates the ethical principles for medical research on human beings. The ethical principles of beneficence, non-maleficence, autonomy, justice, truthfulness, solidarity, loyalty and fidelity, which guide the deontological responsibility of the nursing professional in Colombia, were also applied.
Furthermore, according to Resolution 8430 of 1993, which establishes the scientific, technical and adminis- trative norms for healthcare research in Colombia, the present research was classified in the non-risk category and the authors’ rights were respected by referencing and citing the authors of the articles during the research process, according to the Law 23 of 1982 of Colombia.

PRISMA 2020 flow diagram.
| Bibliographic Reference | Purpose | Methods | Results |
|---|---|---|---|
| Crusat-Abelló, E., & Fernández-Ortega, P. (2021). Nurses' knowledge and attitudes towards euthanasia internationally and nationally: a review of the literature. Enfermería Clínica (English Edition), 31(5), 268-282. doi:10.1016/j.enfcli.2021.01.004 [8]. | To review the available evidence on the attitudes and knowledge of the nurses regarding euthanasia. |
A search was conducted in the PubMed (including Medline), CINAHL, Scopus, PsycINFO, Web of Science and CUIDEN databases using the terms “attitudes” and “knowledge” of nurses both nationally and internationally regarding euthanasia. | Internationally, euthanasia has been legalised in the Netherlands, Luxembourg, Canada and Belgium, the latter of which also provides for child euthanasia; in these countries, nurses are qualified to handle euthanasia requests. |
| Busquets-Surribas, M. (2021). The ethical relevance of nursing care in euthanasia and assisted suicide. Enfermeria clinica, 31(5), 266-267. doi:10.1016/j.enfcli.2021.08.001 [9]. | To critically analyse the ethical relevance of nursing care in euthanasia and assisted suicide. | Editorial. | Studies conducted in countries with experience in the provision of euthanasia, such as Belgium, the Netherlands and Canada, show that nurses are an indispensable link between the applicant and their family. |
| Green, G., Reicher, S., Herman, M., Raspaolo, A., Spero, T., & Blau, A. (2022). Attitudes toward euthanasia-dual view: Nursing students and nurses. Death Studies, 46(1), 124–131. doi:10.1080/07481187.2020.1716887 [10]. | To identify differences between caregivers’ (nurses and students) attitudes, religiosity and care of the terminally ill patient versus individuals requesting euthanasia. | Participants consisted of 210 nurses and nursing students who conducted nursing training across the country. | Nurses and nursing students play a unique and important role with respect to terminally ill patients and the euthanasia process. |
| Francke, A. L., Albers, G., Bilsen, J., de Veer, A. J. E., & Onwuteaka-Philipsen, B. D. (2016). Nursing staff and euthanasia in the Netherlands. A nationwide survey on attitudes and involvement in decision-making and the performance of euthanasia. Patient Education and Counseling, 99(5), 783–789. doi:10.1016/j.pec.2015.11.008 [1] | To provide an insight into the attitudes and involvement of Dutch nurses regarding euthanasia. | The study sample was recruited from an existing nationwide research panel of registered nurses and certified nursing assistants. | Overall, 7% of nurses indicated that they were present during euthanasia to assist the physician and 10% stated that they were present to support the patient or family members. Regarding their participation in euthanasia preparations, <3% mentioned that they had brought the lethal drugs from the pharmacy, connected the infusion line, dissolved the drugs and/or prepared the syringe. |
| Terkamo-Moisio, A., Kvist, T., Kangasniemi, M., Laitila, T., Ryynänen, O.-P., & Pietilä, A.-M. (2017). Nurses’ attitudes towards euthanasia in conflict with professional ethical guidelines. Nursing Ethics, 24(1), 70–86. doi:10.1177/0969733016643861 [11]. | To raise awareness that nurses play a unique and important role in the euthanasia process in countries where it is legalised. | An electronic questionnaire was designed for this study. The questionnaire consisted of four components: demographic characteristics, work-related characteristics, attitudes toward euthanasia, and the Centrality of Religion Scale (CRS). | Compared with physicians, nurses were considered to be more involved in the end-of-life care of patients owing to their greater presence at the patient’s side and frequent confrontation with the patient’s suffering. |
| Vieira-Galán, O. (2021). Euthanasia, an opportunity to decide when. Enfermeria clinica, 31(5), 263-265. doi:10.1016/j.enfcli.2021.08.002 [12]. | To apply the right to die with dignity from a legal point of view based on the recent approval of the law governing euthanasia in the United States and Spain. |
Editorial. | Nursing professionals are a necessary component in the assurance and evaluation commissions provided by euthanasia law because they are guaranteed the opportunity to proactively and successfully participate in individual patient advocacy. |
| Van Humbeeck, L., Piers, R., De Bock, R., & Van Den Noortgate, N. (2022). Flemish healthcare providers’ attitude towards tiredness of life and euthanasia: a survey study. Aging & Mental Health, 26(1), 205–211. doi:10.1080/13607863.2020.1870205 [13]. | To explore the legal understanding and attitudes of nurses and physicians in both acute and chronic geriatric care (Flanders, Belgium) regarding euthanasia in the context of life-weariness among the elderly. | A survey of 194 physicians and 151 nurses in a hospital in Belgium showed that 50% of the staff were aware of the legal basis for the euthanasia process. | Nurses showing greater understanding receive the request for euthanasia because they play a vital role during the various stages of the euthanasia care process: listening attentively to the request, being actively involved in the discussion of the request with colleagues, being involved in decision making, being present or providing assistance during the procedure and supporting the patient and family members. |
| Pesut, B., Thorne, S., Schiller, C. J., Greig, M., & Roussel, J. (2020). The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nursing, 19(1), 12. doi:10.1186/s12912-020-0404-5 [14]. | To better understand the implications of a legislated approach to assisted dying in terms of nurses’ experiences and nursing practice. | Semi-structured interviews were conducted with 59 registered nurses and nurse practitioners. The interviews were audio-recorded, transcribed and managed using qualitative analysis software. | Nurses in this study described great variability in how MAiD had been enacted in their work context and the supports available to guide their practice. The experiences of the registered nurses with assisted dying suggested that they play a central role in negotiating initial assisted dying consultations, which provide important care for patients and family. |
| Verhofstadt, M., Van Assche, K., Sterckx, S., Audenaert, K., & Chambaere, K. (2019). Psychiatric patients requesting euthanasia: Guidelines for sound clinical and ethical decision making. International Journal of Law and Psychiatry, 64, 150–161. doi:10.1016/j.ijlp.2019.04.004 [15]. | To analyse the five Belgian guidelines that have recently been issued with respect to the Belgian practice of patients with psychiatric illnesses requesting euthanasia owing to psychological suffering. | Five recent initiatives offering guidance on euthanasia requests by patients with psychiatric illnesses in Flanders were analysed. They included the need for at least two positive professional opinions from at least two psychiatrists, an a priori assessment system and a two-track approach focusing on the assessment of the patient’s request for euthanasia and the continuation of that individual’s treatment. | The Euthanasia Act stipulates that if there is a nursing team that has regular contact with the patient, the treating physician should discuss the patient’s request for euthanasia with the nursing team or members of that team. In addition to the nursing team, they recommend the inclusion of other caregivers to delve deeper and compare the patient’s background and current living context for identifying overlooked patient wishes in the euthanasia request. |
| Wilson, M., Oliver, P., & Malpas, P. (2019). Nurses’ views on legalizing assisted dying in New Zealand: A cross-sectional study. International Journal of Nursing Studies, 89, 116–124. doi:10.1016/j.ijnurstu.2018.03.012 [16]. | To investigate the views of nurses on the legalisation of assisted dying in various clinical conditions, the willingness to participate in legally assisted dying and the possible deterrents and facilitators of this participation. | A self-selected sample of 475 New Zealand nurses responded to an anonymous online survey disseminated through newsletters and websites of relevant medical and nursing professional bodies. | Nurses spend more time at the patient’s side providing end-of-life care to them compared with any other professional group; moreover, nurses show strong support for assisted dying. Nurses were often delegated tasks during the assisted dying process. |
| Terkamo-Moisio, A., Gastmans, C., Ryynänen, O.-P., & Pietilä, A.-M. (2019). Finnish nurses’ attitudes towards their role in the euthanasia process. Nursing Ethics, 26(3), 700–714. doi:10.1177/0969733017720850 [17]. | To describe nurses' attitudes toward their role in the euthanasia process in Finland. | The questionnaire used included five components: demographic characteristics, work-related characteristics, CRS, nurses' attitudes, and nurses' attitudes toward their role in the euthanasia process. | Overall, 85.2% of the nurses considered that their perceptions should be considered when making decisions about euthanasia. When euthanasia is performed, the main role of nurses is to provide support to the patient and family members. |
| Demedts, D., Roelands, M., Libbrecht, J., & Bilsen, J. (2018). The attitudes, role & knowledge of mental health nurses towards euthanasia because of unbearable mental suffering in Belgium: A pilot study. Journal of Psychiatric and Mental Health Nursing, 25(7), 400–410. doi:10.1111/jpm.12475 [18]. | To determine the attitudes, role and knowledge about euthanasia for unbearable mental suffering (UMS) among nurses employed in mental healthcare. | A cross-sectional survey was conducted with a convenience sample of four psychiatric hospitals in Belgium (n = 133). | Nurses played an important role in the healthcare team and were highly involved in daily patient care. Owing to the nature of their work, they were often the first to receive a request for euthanasia. Nurses were also more familiar with the psychosocial context of the patient than the physician. |
| Lavoie, M., Godin, G., Vézina-Im, L.-A., Blondeau, D., Martineau, I., & Roy, L. (2016). Psychosocial determinants of nurses’ intention to practice euthanasia in palliative care. Nursing Ethics, 23(1), 48–60. doi:10.1177/0969733014557117 [19]. | To identify the psychosocial determinants of nurses’ intentions to practice euthanasia in palliative care if it were legalised. | An anonymous questionnaire was prepared. A random sample of 445 nurses from the province of Quebec, Canada, was selected to participate in the study. |
Although physicians prescribe treatments, it is nurses who often perform the act of administering the medication. It has been reported that cases of euthanasia were occasionally being performed by nurses in the Netherlands, although they were not legally authorised to do so. |
| Vijayalakshmi, P., Nagarajaiah, Reddy, P. D., & Suresh, B. M. (2018). Indian nurses’ attitudes toward euthanasia: Gender differences: Gender differences. Omega, 78(2), 143–160. doi:10.1177/0030222816688576 [20]. | To investigate sex differences among nurses’ perceptions of attitudes toward euthanasia. | A non-probabilistic quantitative cross-sectional design was conducted among nurses working in a tertiary care centre. | Various studies and anecdotal experiences showed that nurses were involved in the care process of euthanasia, i.e., in the request and administration of lethal drugs with the specific intent to end a patient’s life at the explicit request of the patient. |
| Yazdanparast, E., Davoudi, M., Ghorbani, S. H., Akbarian, A., & Chenari, H. A. (2022). Investigating the relationship between moral sensitivity and attitude towards euthanasia in nursing students of Birjand University of Medical Sciences. Clinical Ethics, 17(2), 205–210. doi:10.1177/14777509211016294 [21]. | To assess the relationship between moral sensitivity and attitudes toward euthanasia among nursing students at Birjand University of Medical Sciences in 2020. |
Of the 156 nursing students at Ferdows Nursing School, 144 participated in the study based on the selection criteria. The students completed a demographic information questionnaire, a moral sensitivity questionnaire and an attitude toward euthanasia questionnaire. | Nursing students’ attitudes toward euthanasia were at a low or negative level; this was attributed to their lack of experience in the clinical setting. By contrast, nurses were often the first caregivers to be explicitly involved in the euthanasia process when patients request it. In addition, they were highly motivated to participate in the procedure because they believe that it helps and benefits the individual during the final stages of life as they spend a great deal of time with the patient and family, observing the patient’s suffering and pain. |
| Wilson, M., Wilson, M., Edwards, S., Cusack, L., & Wiechula, R. (2021). Role of attitude in nurses’ responses to requests for assisted dying. Nursing Ethics, 28(5), 670–686. doi:10.1177/0969733020966777 [22]. | To assess the effects of nurses’ attitudes regarding their interaction with normative and control beliefs on the intention to respond to a request for legally assisted death. |
An online survey of 377 Australian registered nurses was conducted. | Compared with nurses who did not support assisted dying, those who supported this practice possessed stronger beliefs in patient rights, perceived social expectations to refer the request, and had stronger control over that intention. |
| Hosseinzadeh, K., & Rafiei, H. (2019). Nursing Student Attitudes toward Euthanasia: A Cross-Sectional Study. Nursing Ethics, 26(2), 496–503. https://doi.org/10.1177/0969733017718393. [23] | To examine the attitudes of a sample of Iranian nursing students toward euthanasia. | Data were collected using a checklist of demographic variables and a self-administered questionnaire that included a definition of euthanasia and 11 closed-ended questions that sought to record the participants’ level of agreement with euthanasia based on a Likert scale. | Overall, >50% of the students in this study agreed or strongly agreed that administering medications in the case of euthanasia can be performed by nurses. |
| Ministry of Health and Social Protection (2021). Resolution 0971- 01 July 2021. In Political Constitution of Colombia 1991 [24]. | The procedure for the reception, processing and reporting of euthanasia requests is established, as well as the guidelines for the organisation and operation of the Committee to grant effect to the Right to Die with Dignity through euthanasia were created. | Regulations | For the proper exercising of the Right to Die with Dignity, the Ministry of Health and Social Protection, in compliance with the orders issued by the Constitutional Court, has generated regulations concerning the actions to be taken by healthcare providers and health administrators when faced with a request for euthanasia, as happened with Resolution 1216 of 2015. |
| Ministry of Health and Social Protection (2015). Resolution 1216- 20 April 2015. In Political Constitution of Colombia 1991 [3]. | The fourth order of Ruling T-970 of 2014 of the Honourable Constitutional Court is complied with regarding the guidelines for the organisation and operation of committees to grant effect to the Right to Die with Dignity. | Regulations | Within the determinations adopted in Ruling T-970, it ordered the Ministry of Health and Social Protection to “issue a guideline and arrange everything necessary for hospitals, clinics, IPS, EPS and healthcare service providers in general to form the interdisciplinary committee referred to in this ruling and to comply with the obligations issued in this decision” within 30 days from the date of communication of the aforementioned ruling. |
3. RESULTS
The chief data obtained from various studies is summarized in Table 1.
3.1. Distribution of Articles in the Databases and based on the Language
The distribution of articles in the different databases and their languages is shown in Fig. (2); a higher number of articles—17 articles, which accounts for 89.47% of the articles—was published in the English language. Regarding the databases, a total of 8 articles were obtained from SAGE Journals, thereby making them the predominant database; 3 articles were selected from the Manual Review database (Fig. 2).
3.2. Distribution of Articles by the Type of Article and Year of Publication
There was a prevalence of qualitative articles in all publication years; moreover, the highest number of articles was published in 2021, with a total of four articles, followed by 2017 and 2020 with three articles each (Fig. 3).
3.3. Distribution of Articles based on Country
The distribution of articles based on country is shown in Fig. (4); a total of four articles were published in Belgium, two articles each in Finland, Iran, Colombia and Canada and one article each in India, Israel, Australia and New Zealand (Fig. 4).
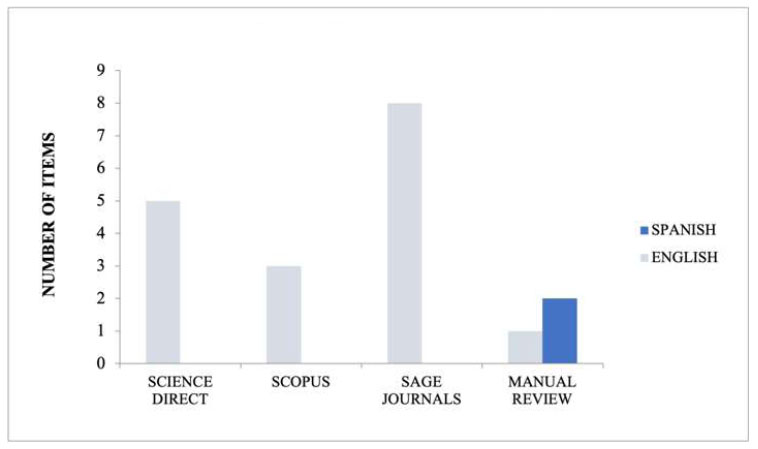
Distribution of articles in the databases and based on the language.

Distribution of articles by type of article and year of publication.
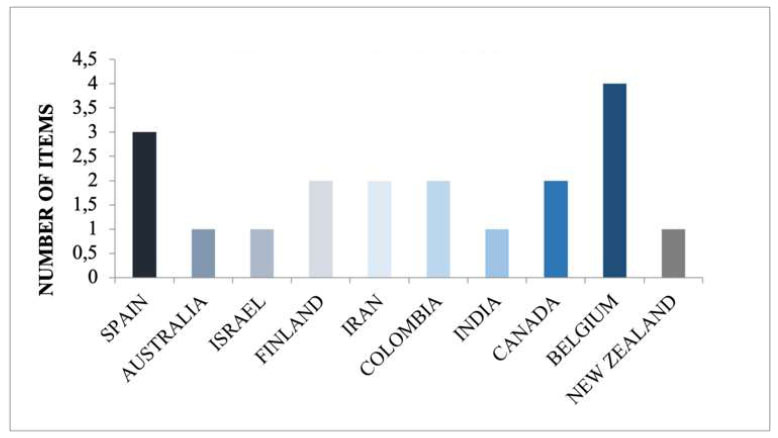
Distribution of articles based on country.

Identification of thematic categories.
4. DISCUSSION
The present literature review included scientific articles published between 2014 and 2022; 17 articles and 2 Resolutions based on the Colombian legal framework were selected for the review. The reviewed articles identified four thematic categories: the reception and management of euthanasia requests and regulations in Colombia; emotional support and effective communication with the patient and their family; involvement in preparation for euthanasia and the administration of medications; and, finally, the management of requests and administration of medications. These categories empha- size the crucial role of nursing staff in providing care management throughout the various stages of life, ensuring continuous support during moments of great vulnerability for the patient and their family, particularly in the end-of-life process. This approach fosters a well-being context that encourages the expression of the patient's wishes, ensuring comprehensive care that respects their dignity.
The thematic categories identified in the publications based on the role of nursing in euthanasia are described ahead (Fig. 5).
4.1. Reception and Management of Euthanasia Requests and Regulations in Colombia
Among the articles reviewed, five demonstrated that nursing professionals are qualified to manage a request for euthanasia because they are the first referents who are consulted when the patient and their family decide and make a request for this practice [8, 9, 18, 21, 22]. In addition, nursing professionals play an important role in the different stages of assisted death from the moment the request is received because they are actively involved in discussions with colleagues and participate in decision-making. This is reflected in three articles that confirm that medical professionals consult and discuss the request for euthanasia with the nursing team to identify overlooked processes before the request for legally assisted death [12, 14, 15].
In Colombia, euthanasia is covered by Resolution 0971 of 2021 [24], which regulates the actions to be performed by healthcare service providers and health administrators when this procedure is requested within the framework of Resolution 1216 of 2015; this procedure is also in compliance with the fourth order of Judgement T-970 of 2014 of the Honorable Constitutional Court in relation to the guidelines for the organization and operation of the committees to enforce the right to die with dignity [3], which clarifies that within the Colombian regulations, the role of the nursing professional when confronted with the request for euthanasia is unclear. In addition, Article 17 of Resolution 0971 of 2021 mentions that the reception and request for euthanasia in the IPS (Healthcare Service Provider Institution) is delegated to the physician and a committee composed of a physician specialized in the patient’s pathology, a lawyer and a clinical psychologist or psychiatrist.
4.2. Emotional Support and Effective Communication with the Patient and Family
Four articles were found in the documents reviewed that concur that nursing professionals are the most involved in patient care; these articles highlight that the primary role of the nurse during the euthanasia procedure is to provide a means of effective communication and emotional support to the patient and family [10, 13, 17]. In addition, one of the articles highlights that nursing professionals—apart from being an emotional support to the patient—are the ones who show greater understanding in a request for euthanasia because they are involved in various functions such as listening attentively to the request, taking active measures to discuss the request with colleagues, participating in decision making and witnessing or assisting in the procedure [13].
4.3. Participation in Preparations for Euthanasia and Administration of Medication
In Belgium in 2015, the results of a study showed that 7% of nurses reported being present during the euthanasia procedure to assist the physician in preparations such as transporting lethal drugs from the pharmacy, connecting the drugs to the infusion line, diluting and preparing the drugs, switching on the drip valve, and the administering the lethal drugs [1].
By contrast, a study conducted in Finland in 2017 concluded that when euthanasia is performed, the main role of the nursing professional is to provide emotional support to the patient and their family. However, the nursing staff also occasionally participate in preparatory activities, such as infusion cannula insertion or euthanasia preparation, which are not considered part of their responsibilities; this assistance is justified if the physician responsible for the procedure is inexperienced [17].
In addition, another study noted that although physicians prescribe the treatments, it is the nursing staff who are often delegated to the act of administering the drugs [16]; in fact, in the Netherlands, it has been reported that the euthanasia procedure is sometimes performed by nurses despite them not having the legal authorization to do so. For example, a recent study in Belgium indicated that 12% of the nursing staff administer lethal drugs prescribed by physicians in cases of euthanasia and even in cases where no explicit request was made by the patient [19].
In the analysis of these articles, four referred to the role of nurses during the process of administering these drugs. It is necessary to emphasize that emotions are involved in this situation because these drugs cause the death of the patient, even when it is at the explicit request of the patient [1, 16, 17, 19].
4.4. Management of Medication Requests and Administration
Among the articles reviewed, it was observed that only one of them, which was conducted in India, conveyed that nursing professionals are involved both in the administration of lethal drugs and management of the euthanasia request to ensure communication with other healthcare specialties participating in this patient intervention [20].
5. LIMITATIONS AND STRENGTHS
Among the limitations encountered was that it was difficult to identify articles published exclusively with nursing professionals who had already graduated, so studies that investigated this topic in university nursing students were included. In addition, taking into account the ethical conflicts present in this practice, the number of studies related to the subject is small, which implies that the total number of studies included is limited.
The strengths of this study are that despite being a recent topic, with implicit ethical and legal limitations, a process of consolidation of all its theoretical component was initiated, to generate responsible practices by nursing personnel, who perform direct care to patients who may request this type of intervention, increasing their foundation and critical thinking, for decision making within this area of health.
CONCLUSION
It has been identified that the nursing professional plays an important role in the care of the patient who requests euthanasia; their role is focused on the following activities: the reception and management of the request, emotional accompaniment to the patient and family, participation in the preparations and the administration of lethal drugs.
The nursing discipline should strengthen research on this subject to support the role the nursing professional plays when they encounter this procedure within a legal framework, thereby highlighting the care that is given to the individuals who request euthanasia.
Training of nursing personnel regarding legally assisted dying is necessary and should be addressed from the academic training stage to influence their perception, which changes and consolidates according to the level of knowledge and experience acquired in the care area.
AUTHOR’S CONTRIBUTION
B.C.D.C.: Wrote the paper; A.P.C.: Studied the concept and design; S.M. V.M. and M.I. A.A.: Collected the data.
LIST OF ABBREVIATIONS
| CASPe | = Critical Appraisal Skills Programme Español |
| STROBE | = Strengthening the Reporting of Observational Studies in Epidemiology |
| PRISMA | = Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
AVAIALABILITY OF DATA AND MATERIALS
The source of the data and materials mentioned in the manuscript are fully described in the document and in the supplementary material.
FUNDING
This research did not receive any specific grants from public, commercial or non-profit sector funding agencies.


