All published articles of this journal are available on ScienceDirect.
Medication Adherence, Blood Pressure Control, Knowledge, Self-care and Self-efficacy among Tunisian Hypertensive Patients
Abstract
Objectives
The aim of this study was to investigate the associated factors with adherence to antihypertensive therapy and to explore the association between medication adherence, blood pressure control, knowledge about hypertension (HTN), self-care, and self-efficacy in hypertensive patients.
Methods
A cross-sectional study was conducted among 750 hypertensive patients in Tunisia. The data collection tool was a 5-section questionnaire including an information sheet, the Girerd medication adherence scale, the HTN Knowledge Level Scale (HK-LS), the Self-care of HTN Inventory (SC-HI), and the Self-Efficacy for Managing Chronic Disease 6-Item Scale (SEM6S).
Results
A low and moderate level of medication adherence has been observed in 83.2% of the participants. Uncontrolled blood pressure was detected in 73.1% of cases. Only 11.5% have a good level of knowledge about HTN. Concerning Self-care practices, 48.8% of patients have inadequate practices of maintenance, 48.8% have inadequate practices of monitoring, and 83.9% have inadequate practices of management. The self-efficacy for managing HTN was weak in 42.1% of the participants.
In multivariate analysis, low medication adherence was associated with the number of antihypertensive pills/day (ORa=2.668; CI95%= (1.447- 4.918) if ≥ 4 pills/day), side effects (ORa=1.834; CI95%= (1.263- 2.665); p=0.001), uncontrolled hypertension (ORa=2.74; CI95%= (1.798- 4.18); p<0.0001), insufficient self-efficacy for managing HTN (ORa=1.773; CI95%=(1.252- 2.512); p<0.0001), and insufficient self-care maintenance (ORa=2.220; CI95%=(1.562- 3.1570); p<0.0001).
Conclusion
Low medication adherence was associated with uncontrolled blood pressure, more anti-hypertensive pills, side effects, lower self-efficacy, and lower self-care maintenance. Nursing interventions improving the management skills of hypertensive patients may be beneficial in controlling the disease and its subsequent consequences.
1. INTRODUCTION
Hypertension (HTN) is an international health concern. It affects 1.28 billion adults aged 30–79 years worldwide [1, 2]. It is considered one of the main modifiable risk factors for cardiovascular diseases (CVDs). In fact, high blood pressure (BP) is one of the major risk factors for ischemic heart disease, stroke, chronic kidney disease, dementia, and other causes of CVDs [3, 4].
Nowadays, there are many advances in therapeutic strategies for HTN, with demonstrated advantages in decreasing cardiovascular morbidity and mortality [5], and medication adherence is crucial to achieving BP goals. Consequently, partial or total medication non-adherence is a major concern in the long-term management of HTN [6].
On the other hand, hypertensive patients are additionally instructed to improve their lifestyle, such as a healthy low-salt diet and weight loss. Regular physical activity has been identified as the most crucial implementation for managing uncontrolled BP [7]. Therefore, a systematic review has proven that self-care practices are low among patients with HTN [7].
Furthermore, good knowledge about HTN and therapeutic processes may allow controlled BP, a good level of medication adherence, a healthy lifestyle, and improved self-efficacy for managing a chronic disease [8].
Thus, this study aimed to investigate the associated factors with adherence to antihypertensive therapy and to explore the association between medication adherence, PB control, knowledge about HTN, self-care, and self-efficacy for managing HTN among hypertensive patients.
2. METHODS
2.1. Study Design and Setting
A cross-sectional study was conducted between May and July 2021 among hypertensive outpatients followed up at the « National Social Security Fund » polyclinic in Sfax, Tunisia.
2.2. Patient Selection
A randomized, systematic sampling was used. The patients were selected from the list of appointments in the department of General Medicine. The inclusion criteria included diagnosis of HTN, age over 18 years, and use of antihypertensive medications for at least a year. The exclusion criteria included pregnancy, communication disorders, or untreated mental disease.
2.3. Data Collection Instrument
The data collection tool was a 5-section questionnaire in Arabic.
2.3.1. The First Section
The first section was an information sheet, which focuses on the major factors that may influence patients with chronic illnesses to adhere to their treatment plan. We identified age, gender, education level, and socioeconomic factors like occupation and socio-economic level. According to the “Africa Housing Finance Yearbook 2019,” three socioeconomic level categories were defined: low (0DT to 403 TD), moderate (404 TD to 999 TD), and high (1000 TD and above) [9].
We also noticed the antecedents, disease-related aspects like disease complications, systolic and diastolic BP, and the duration of HTN.
Treatment-related factors included items like the number of antihypertensive pills taken, the total number of pills taken, and side effects.
2.3.2. Patients' Medication Adherence
Patients' medication adherence was assessed using the 6-item Girerd scale. This scale consists of six questions with binary answers. The total score ranges from 0 to 6. If the answer is ‘no’ to all the questions (score = 0), adherence is considered high. If the answer is ‘yes’ to one or two questions (score = 1 or 2), there is moderate adherence. If three or more answers are ‘yes’ (score ≥ 3), adherence is considered low [10].
2.3.3. Participants’ Knowledge about HTN
Participants’ knowledge about HTN was assessed using the Hypertension Knowledge-Level Scale. It contains 22 items divided into 6 dimensions: definition of HTN, treatment, medication compliance, lifestyle, diet, and complications.
Each true response was coded as 1 point (maximum score is 22), and scores were presented in the current study as a percentage out of 100. The higher the score, the higher the knowledge about HTN [11]. A score of ≥ 75% was considered good, and a score between 50 and 75% was considered moderate.
2.3.4. The Level of Self-care Practices
The level of self-care practices was assessed using the Self-care of Hypertension Inventory (SC-HI). This inventory contains 23 items divided into three subscales: maintenance, monitoring, and management.
Each subscale was scored identically and distinctly from 0 to 100. The final score was calculated as 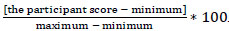 .
.
A score of 70 or above indicates developed self-care [12, 13].
2.3.5. Self-efficacy for Managing HTN
Self-efficacy for managing HTN was assessed using the Self-Efficacy for Managing Chronic Disease 6-Item Scale. This scale measures the confidence of chronic disease patients in doing certain functions. Each item ranges from “not at all confident [1]” to “completely confident [10]” on a 10-point scale. The subscale was scored from 0 to 100 using percentage conversion. A higher mean score of self-efficacy indicated greater self-efficacy [14]. A score less than 66/100 indicated weak self-efficacy [14].
2.4. Data Collection
Prior to the consultation, an interview was conducted in an isolated space to guarantee comfort. The respondents were interviewed in Arabic, and the investigator used a clear language.
It took twenty to thirty minutes for the interview, the BP measurement, and the clinical examination of the patient.
An uncontrolled BP was defined as a systolic BP ≥140 mmHg or a diastolic BP ≥90 mmHg.
2.5. Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences version 24.0. The normality of data distribution was tested using the Kolmogorov-Smirnov test. Mean and standard deviation were used to represent quantitative data when normality was present, otherwise, the median and interquartile range were used. The frequencies were used to describe qualitative variables.
In the univariate analysis, the Chi-square test was used to test the association between qualitative variables, and the ANOVA test or the Kruskal-Wallis test was used to test the association between quantitative and qualitative variables, according to the conditions of application. The correlation between two quantitative variables was tested by the R coefficient of Pearson. The R coefficient was considered high if it was >0.7 and weak if <0.3.
For multivariate analysis, we considered a binary variable (low adherence versus moderate or high adherence). This analysis was done with a binary logistic regression model to identify the independent predictors of a low level of medication adherence. In this model, we introduced all variables with p<0.2 in the univariate analysis.
The significance threshold was fixed at p <0.05.
2.6. Ethical Considerations
This study was approved by the Research Ethics Committee of the Protection of Persons. Permission from the general medicine department head was acquired before the data collection. Measures have been taken to respect the rights and freedom of participants. They were informed of the aim of the study and the terms of participation through a consent form. Freedom regarding participation in the study was clearly stated. The confidentiality of the data obtained and the anonymity of the participants was respected.
3. RESULTS
A total of 750 hypertensive patients were included in this study.
3.1. Socio-demographic Characteristics
The male-to-female sex ratio was 0.46. The characteristics of the study participants (n = 750) are shown in Table 1.
3.2. Clinical Data
Medical antecedents were noticed in 609 patients (81.2%). In 73.1% of cases, BP was uncontrolled. Other clinical characteristics were resumed in Table 2.
3.3. Medication Adherence, Knowledge about Hypertension, Self-care, and Self-efficacy
Among the 750 patients, only 126 (16.8%) have a good level of medication adherence.
Concerning the level of knowledge, the median score was 54.5%, ranging from 18.1% to 100%.
| Variables | Total Sample (n = 750) |
|---|---|
| Age (years) | - |
| Mean (SD*) | 63.8 (8.8) |
| Sex (n, %) | - |
| Male | 239 (31.9) |
| Female | 511 (68.1) |
| Level of education (n, %) | - |
| Illiterate | 155 (20.7) |
| Primary | 404 (53.8) |
| Secondary | 165 (22.0) |
| University | 26 (3.5) |
| Socio-economic level (n, %) | - |
| Low | 180 (24.0) |
| Moderate | 541 (72.1) |
| High | 29 (3.9) |
| Occupation (n, %) | - |
| Unemployed** | 620 (82.6) |
| Employed | 130 (17.4) |
| Variables | N (%) |
|---|---|
| Medical Antecedents (n, %) | - |
| Total | 609 (81.2) |
| Diabetes | 404 (53.9) |
| Dyslipidemia | 346 (46.1) |
| Other cardiovascular diseases | 89 (11.9) |
| Other medical antecedents (asthma, hypothyroidism, …) | 151 (20.1) |
| Number of antecedents | - |
| 1 | 306 (40.8) |
| 2 | 232 (30.9) |
| ≥ 3 | 71 (9.4) |
| Body Mass Index (kg/m2) Median (IQR*) | 27.37 (25.2) |
| Duration of hypertension (years) Median (IQR*) | 10.00 (5.0) |
| Systolic blood pressure (mmHg) Median (IQR*) | 147.00 (140.0) |
| Diastolic blood pressure (mmHg) Median (IQR*) | 84.00 (76.0) |
| Uncontrolled blood pressure (n, %) | 548 (73.0) |
| Complications of hypertension (n, %) | - |
| Total | 106 (14.1) |
| Heart Attack | 62 (8.3) |
| Kidney failure | 31 (4.1) |
| Stroke | 15 (2.0) |
| No. of anti-hypertensive pills/day (n, %) | - |
| 1 | 203 (27.1) |
| 2 | 232 (30.9) |
| 3 | 242 (32.3) |
| ≥ 4 | 73 (9.7) |
| No. of total pills/day (n, %) | - |
| 1-5 | 447 (59.6) |
| 6-10 | 271 (36.1) |
| ≥ 11 | 32 (4.3) |
| Side effects (n, %) | 177 (3.6) |
| Variables | |
|---|---|
| Medication Adherence (n, %) | - |
| High | 126 (16.8) |
| Moderate | 377 (50.3) |
| Low | 247 (32.9) |
| Hypertension Knowledge- Level Scale (n, %) | - |
| Good level of knowledge | 86 (11.5) |
| Moderate level of knowledge | 368 (49.0) |
| Low level of knowledge | 296 (39.5) |
| Self-care of Hypertension Inventory (/100) | - |
|
Self-care Maintenance score Median (IQR*) >70 (n, %) |
52.00 (40.00) 385 (51.2) |
|
Self-care Monitoring score Median (IQR*) >70 (n, %) |
44.44 (27.77) 385 (51.2) |
|
Self-care Management score Median (IQR*) >70 (n, %) |
47.05 (35.29) 121 (16.1) |
| Self-Efficacy for Managing Chronic Disease (/100) | - |
| Median (IQR*) | 53.00 (47.00) |
| < 66 (n, %) | 316 (42.1) |
Concerning the self-care management score, adequate practices for the management dimension were observed in 16.1%. The self-efficacy for managing HTN was weak in 42.1% of cases (Table 3).
3.4. Related Factors to Medication Adherence in Univariate Analysis
3.4.1. Socio-demographic Factors
The univariate analysis demonstrated that the level of medication adherence was associated with the level of education and the socio-economic level (Table 4).
3.4.2. Clinical Data Factors
The univariate analysis demonstrated that the level of medication adherence was associated with the duration of hypertension, the control of the BP, medical antecedents, the number of pills, and side effects (Table 5].
3.4.3. Association of Knowledge about Hypertension, Self-care, and Self-efficacy to Medication Adherence among Hypertensive Patients
The univariate analysis demonstrated that the level of medication adherence was associated with knowledge scores, self-care scores, and self-efficacy for managing chronic disease scores (Table 6).
The coefficient of correlation (R) was higher with maintenance and management dimensions of the self-care inventory (Table 6).
3.5. Related Factors to Medication Adherence in Multivariate Analysis
In multivariate analysis, low medication adherence was associated with uncontrolled hypertension, the number of antihypertensive pills per day, side effects, insufficient self-efficacy, and insufficient self-care maintenance (Table 7).
| Variable | Low (n=247) | Moderate (n=377) | High (n=126) | P-value |
|---|---|---|---|---|
| Age (years), Mean (SD) | 64.26 (8.83) | 63.79 (8.81) | 63.28 (9.20) | 0. 316 a |
| Sex (n, %) | - | - | - | - |
| Male | 78 (32.6) | 121 (50.6) | 40 (16.7) | 0.990 b |
| Female | 169 (33.1) | 256 (50.1) | 86 (16.8) | - |
| Level of education (n, %) | - | - | - | 0.002 b |
| Illiterate | 71 (45.8) | 65 (41.9) | 19 (12.3) | - |
| Primary | 127 (31.4) | 208 (51.5) | 69 (17.1) | - |
| Secondary or University | 49 (25.7) | 104 (54.5) | 38 (19.9) | - |
| Socio-economic level (n, %) | - | - | - | 0.002 b |
| Low | 79 (43.9) | 84 (46.7) | 17 (9.4) | - |
| Moderate | 161 (29.8) | 277 (51.2) | 103 (19.0) | - |
| High | 7 (24.1) | 16 (55.2) | 6 (20.7) | - |
| Occupation (n, %) | - | - | - | 0.398 b |
| Unemployed | 205 (33.1) | 316 (51.0) | 99 (15.9) | - |
| Employed | 42 (30.8) | 61 (49.2) | 27 (20.0) | - |
| Variable | Medication Adherence | |||
|---|---|---|---|---|
| Low (n=247) |
Moderate (n=377) |
High (n=126) |
P-value | |
| Duration of hypertension (years), Median (IQR) | 11.00 (10.00) | 10.00 (11.00) | 7.00 (10.00) | <0.0001a |
| Systolic blood pressure (mmHg), Median (IQR) | 152.00 (20.00) | 146.00 (19.00) | 143.00 (17.00) | <0.0001 a |
| Diastolic blood pressure (mmHg) Median (IQR) | 85.00 (12.0) | 83.00 (15.0) | 82.00 (12.0) | <0.0001 a |
| Controlled blood pressure (n, %) | - | - | - | <0.0001 b |
| Yes | 35 (17.3) | 116 (57.4) | 51 (25.2) | |
| No | 247 (32.9) | 377 (50.3) | 126 (16.8) | |
| Body Mass Index (kg/m2) Median (IQR) | 27.88 (5.28) | 27.43 (5.11) | 26.52 (4.79) | 0. 101 a |
| Complication of hypertension (n, %) | 38 (15.4) | 52 (13.8) | 16 (12.7) | 0.753 b |
| Medical antecedents (n, %) | - | - | - | 0.015 b |
| Yes | 211 (34.6) | 306 (50.2) | 92 (15.1) | |
| No | 36 (25.5) | 71 (50.4) | 34 (24.1) | |
| No. of anti-hypertensive pills (n, %) | - | - | - | <0.0001 a |
| 1 | 44 (21.7) | 106 (52.2) | 53 (26.1) | |
| 2 | 75 (32.3) | 120 (51.7) | 37 (15.9) | |
| 3 | 92 (38.0) | 122 (50.4) | 28 (11.6) | |
| ≥ 4 | 36 (49.3) | 29 (39.7) | 8 (11.0) | |
| No. of total pills (n, %) | - | - | - | <0.0001 a |
| 1-5 | 118 (26.3) | 221 (49.3) | 109 (24.3) | |
| 6-10 | 114 (42.2) | 140 (51.9) | 16 (5.9) | |
| ≥ 11 | 15 (46.9) | 16 (50.0) | 1 (3.1) | |
| Side effects (n, %) | - | - | - | <0.0001 b |
| Yes | 82 (46.3) | 77 (43.5) | 18 (10.2) | |
| No | 165 (28.8) | 300 (52.4) | 108 (18.8) | |
| Variable | Medication Adherence | P-value | Rb | P-value | ||
|---|---|---|---|---|---|---|
| Low (n=247) |
Moderate (n=377) | High (n=126) | ||||
| Hypertension Knowledge Level Scale | - | - | - | - | ||
| Median (IQR*) | 50.00 (9.09) | 54.54 (18.18) | 54.54 (18.18) | <0.0001a | 0.16 | <0.0001 |
| Self-care of Hypertension Inventory (/100) | - | - | - | - | ||
|
Maintenance, Median (IQR*) |
44.00 (20.00) | 52.00 (16.00) | 56.00 (16.00) | <0.0001a | 0.36 | <0.0001 |
|
Monitoring, Median (IQR*) |
38.89 (38.89) | 44.44 (27.78) | 50.00 (33.33) | 0.006 a | 0.15 | <0.0001 |
|
Management Median (IQR*) |
41.17 (23.53) | 52.94 (23.53) | 52.94 (23.53) | <0.0001a | 0.26 | <0.0001 |
| Self-Efficacy for Managing Chronic Disease (/100) | - | - | - | - | ||
| Median (IQR) | 50.00 (14.00) | 53.00 (11.00) | 56.00 (12.00) | <0.0001a | 0.25 | <0.0001 |
| Variable | ORa | C.I. 95% | P-value |
|---|---|---|---|
| Number of Antihypertensive Pills/day | - | - | 0.006 |
| 2 | 1.609 | 1.018- 2.543 | 0.042 |
| 3 | 1.898 | 1.215- 2.966 | 0.005 |
| ≥ 4 | 2.668 | 1.447- 4.918 | 0.002 |
| Side effects | 1.834 | 1.263- 2.665 | 0.001 |
| Self-are maintenance insufficient | 2.220 | 1.562- 3.157 | <0.0001 |
| Self-efficacy insufficient | 1.773 | 1.252- 2.512 | <0.0001 |
| Controlled hypertension | 0.364 | 0.239- 0.556 | <0.0001 |
4. DISCUSSION
The current study showed that only 16.8% have good medication adherence, and 32.9% have low medication adherence. Failure to adhere to HTN medication is a serious public health concern that represents a substantial risk for complications, disability, and death [13].
In reality, low or poor adherence reduces medication's therapeutic benefits. It has a detrimental impact on the efficacy, safety, and cost of medicines, as well as the reduced efficacy and efficiency of HTN treatment [15].
Previous research found widely varying levels of medication adherence. A study conducted in six Indonesian hospitals among 693 hypertensive patients revealed that the majority (76.2%) had poor adherence, while just 7.6% had good adherence [16]. Another study conducted in Saudi Arabia showed that 36.3% of the participants had high levels of adherence, while the remainder of the participants (63.7%) had low or medium adherence [17]. Moreover, a systemic review of 92443 people showed that the pooled rate of non-adherence to antihypertensive medication in low- and middle-income countries was high (63.35%) [18]. A recent systematic review conducted in Nepal, a low-resource country, revealed that 49% of patients did not take their antihypertensive drugs as prescribed forms [19] (Table 8).
According to our study, low adherence was substantially associated with uncontrolled hypertension, a higher number of antihypertensive pills per day, side effects, insufficient self-efficacy, and insufficient self-care maintenance.
The Indonesian study [16] showed that low adherence was associated with rural settings, university education, and low income [16]. The Saudian study also demonstrated that low and medium adherence were significantly higher among married participants, older patients, and those residing in a village, while a correlation was observed between medication adherence and illness perception [17].
According to the systemic review [18], non-adherence rates were higher among well-controlled BP, females, older adults, and those with lower levels of education [18]. The study conducted in Nepal showed that rural areas had a higher rate of non-adherence (56%) compared to urban areas (42%). Non-adherence was also frequently associated with forgetfulness, carelessness, the cost of prescriptions, a high number of comorbidities, and the usage of alternate prescription forms [19].
Systematic reviews focused on the factors that increase non-adherence and classified them into five groups, according to the World Health Organization [19, 20].
The first category represents socioeconomic criteria such as income, ethnicity, and educational attainment [19, 20].
The second category includes aspects specific to the patient, such as age, gender, and marital status, including single status, younger age, low educational attainment, and unemployment, such as low health literacy and awareness, lack of knowledge of HTN, attitude towards HTN, self-efficacy, and social support [19, 20].
The third category consists of disease-related factors such as the disease's duration, low sickness perception, and comorbidities [19, 20].
The fourth category includes therapy-related factors such as treatment duration, frequency of intake, and daily pill number, as well as inconsistent drug regimen schedules [19, 20].
Finally, issues relating to the healthcare system, such as pharmaceutical expenses and health insurance were included [19].
In fact, health-care system factors such as an effective patient-provider connection, accessibility to medical services, use of specialty clinics and programs for HTN, and health insurance were found to be positively connected with adherence [20].
The current study also indicated that just 11.5% of participants had good knowledge of HTN, while the rest (49.1% and 39.5%, respectively) had a moderate or low level of knowledge. Consistent with these findings, a systematic review of low- and middle-income countries found that low drug adherence is explained by a lack of knowledge [21]. Furthermore, a cross-sectional study conducted in Iran indicated that health literacy could predict self-efficacy (beta = 0.262, p =0.001) and self-care behaviors (beta = 0.639, p <0.0001) [22].
On the other hand, self-care is an important part of managing chronic diseases continuously. A comprehensive self-care strategy can be regarded as having three key principles: maintenance, monitoring, and management.
In our study, we noticed a median score of 52% for the median scores for the maintenance dimension, a median score of 44% for the monitoring dimension, and a median score of 47% for the management dimension. In a Polish study of 250 HTN patients using the same scale (SC-HI), the mean scores were highest for maintenance (mean 56.73%), monitoring (mean 62.47%), and management (mean 64.17%) [23].
Actually, increasing self-efficacy appears to be critical to support the continuous self-care habits of individuals with essential hypertensive disease. The concept of implementing behavioral changes to self-manage chronic illness has gained traction in the field of lifestyle medicine. A systematic review found that self-efficacy is a key variable in the efficient management of chronic illnesses, and higher levels of self-efficacy were associated with self-care practices and taking medications as recommended [7].
Our study found that self-efficacy to manage HTN was weak in 42.1% of cases. A study of 516 hypertensive patients in a low-income rural area of China found that 3.9% of patients have low self-efficacy, 81.8% have medium self-efficacy, and 14.3% have high self-efficacy [24]. A meta-analysis of 7 studies in HTN patients from Asian and African nations found that individuals with good self-efficacy are twice as likely to adhere to medicine as those with low self-efficacy (OR= 2.11; 95% CI= 1.27 to 3.52; p<0.004) [25].
These results were coherent with the correlation analysis. In our study, we found a significant correlation between medication adherence and self-efficacy (r = 0.25, p <0.0001). A study carried out in China revealed a substantial positive association between self-efficacy and medication adherence (r = 0.591, p < 0.001) [26].
Thus, our study highlighted many problems concerning medication adherence, knowledge about HTN, self-care, and self-efficacy among hypertensive patients in our country. The large sample size and the use of specific Arabic scales to evaluate every one of these problems in patients with HTN are the strongest points. However, we must recognize some limitations of this study. First, the cross-sectional nature of the study did not allow us to verify the temporal sequence between medication adherence and the complications of HTN or the lack of control of BP. On the other hand, data collection was conducted during the COVID-19 pandemic, which may have an impact on people with chronic diseases in terms of improving access to the healthcare system and resources. However, in reality, for hypertensive individuals, the pandemic did not create new barriers but rather exacerbated existing ones [27, 28]. Finally, the data was gathered from only one healthcare center.
As a result, our findings, representing the main problems of hypertensive patients treated in the “National Fund for Social Security” polyclinic, can help caregivers focus their actions toward hypertensive patients to increase the efficacity of the management of their disease. Therefore, caregivers have to pay special attention to patients who are at risk of suffering from uncontrolled BP. In addition to the BP measure, an innovative approach, such as Electronic Health Records Data, can be used to stratify patients based on their risk of exhibiting uncontrolled HTN [29]. Then, tailored individualized interventions are implemented for patients’ needs, which will ultimately be useful in controlling HTN and enhancing patients' management skills [30].
CONCLUSION
The findings of this cross-sectional study showed that hypertensive patients suffer from several problems concerning therapeutic compliance, knowledge, and self-management of hypertension. Caregivers should prioritize evaluating patient characteristics that affect disease management. Their place is essential to improving therapeutic education of hypertensive patients, especially by using new approaches, such as Electronic Health Records Data.
AUTHOR’S CONTRIBUTIONS
F.T., I.T., J.J., H.S.: Study conception and design; F.T: Data collection; F.T., J. J., H.S.: Analysis and interpretation of results; F.T., I.T: Draft manuscript.
LIST OF ABBREVIATIONS
| HTN | = Hypertension |
| CVDs | = Cardiovascular diseases |
| SC-HI | = Self-care of hypertension Inventory |
| BP | = Blood pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Research Ethics Committee of the Protection of Persons (CPP SUD No. 0427/2023).
HUMAN AND ANIMAL RIGHTS
. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All patients were informed of the aim of the study and the terms of participation through a consent form.


