All published articles of this journal are available on ScienceDirect.
From Drama to Transformation as a Person and an Emergency Unit Professional in the Pandemic: A Grounded Theory Approach
Abstract
Background
Pandemic flows have proven increasingly challenging, signaling the need for more effective global policies that benefit healthcare worker safety.
Objectives
To understand the health staff's interactional experience in an emergency unit with the COVID-19 pandemic and to develop a theoretical model representative of this experience.
Methods
A qualitative research with theoretical saturation through analysis of the 15th non-directive interview, according to Grounded Theory, was developed with physicians, nurses, and nursing technicians in an emergency unit who experienced the pandemic's beginning.
Results
The experience unfolded into subprocesses: Considering oneself, at the beginning of the pandemic, as the leading actor of a drama (A); Looking for strategies to cope with the pandemic (B); Transforming as professional and person (C). From dramatic leading role to professional and personal improvement of healthcare staff in emergency services during COVID-19.
Conclusion
The model indicated a staff waking up to occupational risks with pathogens in the interface with symbols of the devastating and dramatic concreteness of the SARS-CoV-2 virus and insufficient informational, material, human, and psychosocial resources, encouraging them to use standard precautions even after the pandemic.
1. INTRODUCTION
The spread of the new coronavirus, SARS-CoV-2, the causal agent of the emerging infectious disease COVID-19, occurred quickly between continents. Consequently, there was little time for countries' health systems, regardless of their levels of development, to adjust to their populations' demands, in addition to providing better working safety conditions for healthcare professionals who, regardless of the risks, guaranteed care for people with severe and critical COVID-19, which overcrowded Emergency and Urgent Network (RUE) services.
Between December 2019 and January 2020, the virus left the Chinese province of Hubei (origin) to head toward Europe and its Asian neighbors [1]. On January 30, 2020, the World Health Organization (WHO) declared the spread of the virus COVID-19 as an outbreak, and that same year, on March 11, it was considered a pandemic [2].
During this period, the rest of the world followed the dramatic globalization of the pandemic through the media, especially what was happening in China and Europe, and in Italy. Healthcare professionals became increasingly frightened by the significant number of Chinese co-workers who were becoming infected and dying. By the beginning of March 2020, in China alone, more than 3,300 healthcare professionals were infected, with 22 deaths, as well as in Italy, where 20% of healthcare professionals were infected and hospitals no longer had enough places to admit patients with Severe Acute Respiratory Syndrome (SARS) [3].
Much of the reason for this high number of infected healthcare professionals globally exposed how unprepared healthcare institutions were and, consequently, their professionals, with the ability to benefit from standard precautions in the face of epidemics or pandemics, placing thousands of them at occupational risk [4].
Standard precautions aim to reduce the risk of transmitting pathogens through blood or other sources, whether known or unknown and should always be used when caring for all patients. Among the most important components of these precautions are hand hygiene, the use of personal protection assessed based on risk analysis, and the contact that will be made with blood or other body fluids or pathogens. The quantitative and qualitative availability of human and material resources, along with the leadership and training of healthcare professionals, patients, and visitors, is essential to improving the safety climate in healthcare settings [5].
In Brazil, since October 2007, the Ministry of Health (MH) and the Brazilian National Health Regulatory Agency (ANVISA - Agência Nacional de Vigilância Sanitária), with support from the Pan American Health Organization (PAHO), have reproduced WHO guidelines on standard precautions for infection control, including warning about their use as a way of responding to pandemics and epidemics, reducing risks and improving patient and healthcare staff safety [6].
Moreover, due to all the adversities imposed, such as healthcare professionals' exposure to the COVID-19 pandemic, on September 2, 2020, PAHO and WHO recorded the largest number of these infected profes- sionals in the Americas: around 570 thousand, with 2.5 thousand deaths from the disease. Brazil alone accounted for almost 54% of those infected, totaling 307 thousand. Nursing professionals, especially nursing technicians and assistants, were the most affected. Furthermore, the WHO recorded 2,500 deaths of healthcare professionals on the continent, 289 of which were in Brazil, corresponding to 11.6% [7].
Such a context is a public health concern, which was emphasized by other research, with results summarized by a recent review study pointing to the psychological and occupational impacts of successive pandemics on healthcare professionals. It was emphasized that the war environment, created by these successive events in recent times, has increased frontline healthcare professionals' vulnerability. They often experience feelings of helpless- ness and, consequently, impotence with a lack of control over environmental phenomena perceived as devastating. Faced with this scenario, professionals appear fragile in the face of the inexorability of risks and threats to their integrity, making professional practice in this context (world) meaningless. This cognitive process has been associated with depressive symptoms and conditions [8].
Given the context, the question emerged: how was the emergency service healthcare professionals' initial experience during the COVID-19 pandemic?
Given the context, the question emerged: how was the emergency service healthcare professionals' experience during the COVID-19 pandemic?
The question is justified as successive seizures of healthcare professionals' work processes due to global flows of pandemics proved to be challenging, validating the need for effective global policies to benefit mental and physical health, i.e., to preserve healthcare worker safety when assuming new events.
This article aims to understand the health staff's interactional experience in an emergency unit during the COVID-19 pandemic and to develop a theoretical model representative of this experience.
2. MATERIALS AND METHODS
2.1. Ethical Aspects
This research project was carried out after approval by a Research Ethics Committee, obtaining informed consent from the actors to participate in the research. Furthermore, to preserve their anonymity, after the interviews' audio recordings were transcribed in full, the digital files were deleted and were identified alpha- numerically: N (Nurse), P (Physician), and T (Nursing technician/Assistant).
The interviews were carried out individually and in a private room at the service, where only the interviewee and the interviewer were present upon appointment after a work shift. One of the researchers trained to perform the data collection technique was the interviewer, who worked as a clinical nurse on-site, but without any management authority over the staff.
2.2. Theoretical-methodological Framework and Study Design
This qualitative research, with a comprehensive approach, uses Grounded Theory (GT) [9] as a methodological framework and Symbolic Interactionism [10] as a theoretical framework. Furthermore, this study followed the Consolidated criteria for Reporting Qualitative research (COREQ) guidelines to check the quality and transparency of this study design [11].
2.3. Research Setting and Actors
The study was carried out with a health staff composed of medical professionals, nurses, nursing technicians, and/or assistants, crowded into one of the main entry points of RUE called Central Municipal Emergency Room (PSMC), in a municipality in the state of São Paulo.
It is noteworthy that the staff's experience refers to the beginning of the pandemic, between July and August 2020, before the second wave of the disease took hold in November of the same year [12].
Furthermore, to preserve PSMC's aim as the main reference for treating highly complex cases of patients in critical condition and, at the same time, welcoming and assisting victims of the pandemic, especially those that progressed into serious and critical cases, the Municipal Health Department, in mid-April 2020, occupied a building attached to PSMC, transforming it into a COVID-19 Center (PAC). This was configured as a reference for severe acute respiratory syndrome (SARS) care in the municipality. With this strategy, the 17-bed PSMC now offers 52 beds, 24 for stabilization and 28 for wards, i.e., it increased bed capacity by 67%.
2.4. Data Source
Data collection took place through primary data, using the non-directive (in-depth) interview technique, with the guiding question: how was your experience during the COVID-19 pandemic?
2.5. Data Analysis: Methodological Framework
At the end of the interviews, they were transcribed and subjected to manual analysis by one of the researchers and validated by the second one, who has training and experience in operationalizing the GT methodological framework steps [9].
At the end of the interviews, they were transcribed and subjected to manual analysis by one of the researchers and validated by the second one, who has training and experience in operationalizing the GT methodological framework steps [9].
(1st) Microanalysis is a detailed line-by-line analysis required to generate initial categories (with their properties and dimensions), suggesting relationships between them and a combination of open and axial coding.
(2nd) Open coding is a data analytical process through which concepts, their properties, and dimensions are identified. At this stage, a large amount of coded data was reduced by naming groupings of items (codes) with similar meanings and, consequently, elaborating concepts. A concept is an abstract representation of an event, object, action, or interaction that a researcher identifies as being significant in the data. In the methodological framework used, categories are concepts derived from data that represent phenomena. Concepts begin to be constituted when an analyst begins the process of grouping or classifying them into more abstract terms and categories.
(3rd) Axial coding is the process of systematically relating categories to their subcategories according to their properties and dimensions. This stage of analysis is important for constructing a theory.
(4th) Selective coding is the process of theory integration and improvement. In integration, categories are organized around a central concept through various techniques, such as describing the story, using diagrams, classification, and review notes.
As recommended by this type of research, data collection and analysis took place concomitantly until theoretical saturation was obtained, based on the analysis of the 15th interview. Furthermore, this study used the two strategies recommended by the methodological frame- work for validating the discovered model, recommending comparison of it with raw data, as well as presenting it for assessment by actors [9]. In both strategies, the model proved to disregard actors' experiences (Fig. 1).
2.6. Data Interpretation: Theoretical Framework
Data interpretation (experience and theoretical model) took place in the light of Symbolic Interactionism, an approach distinct from psychology that studies life and human action in groups. This framework is based on the concepts of symbol, self, mind, taking the role of the other, human action, and social interaction [10].
3. RESULTS
3.1. Research Actor Characterization
The health staff consisted of 15 actors, six nursing technicians, four nurses, and five physicians. Of these, nine were women, and six were men aged 25 to 64 years with three to 38 years of experience.
3.2. The Interactional Process Experienced by Emergency Unit Healthcare Staff during the COVID-19 Pandemic
Data analysis, according to GT, allows us to understand the interactional experiences of healthcare professionals working in emergency and urgent services during the COVID-19 pandemic and to establish theoretical relationships between the components (categories and subcategories). This is an explanatory and analytical process of actions and interactions relating to experience, which unfolds into three subprocesses: Considering oneself, at the beginning of the pandemic, as the leading actor of a drama (A) Looking for strategies to cope with the pandemic (B) Transforming as professionals and person (C) (Chart 1).
Considering oneself, at the beginning of the pandemic, as the leading actor of a drama (A) surmises from the initial circumstances of commotion in the face of the psychological distress generated by healthcare professionals in emergency and urgent services because they perceive themselves as well as the institution where they work to be unprepared to deal with COVID-19 patients. Therefore, they reveal feelings of fear, insecurity, and unpreparedness by the institution and the professionals themselves. This subprocess aggregates five categories, from A1 to A5.
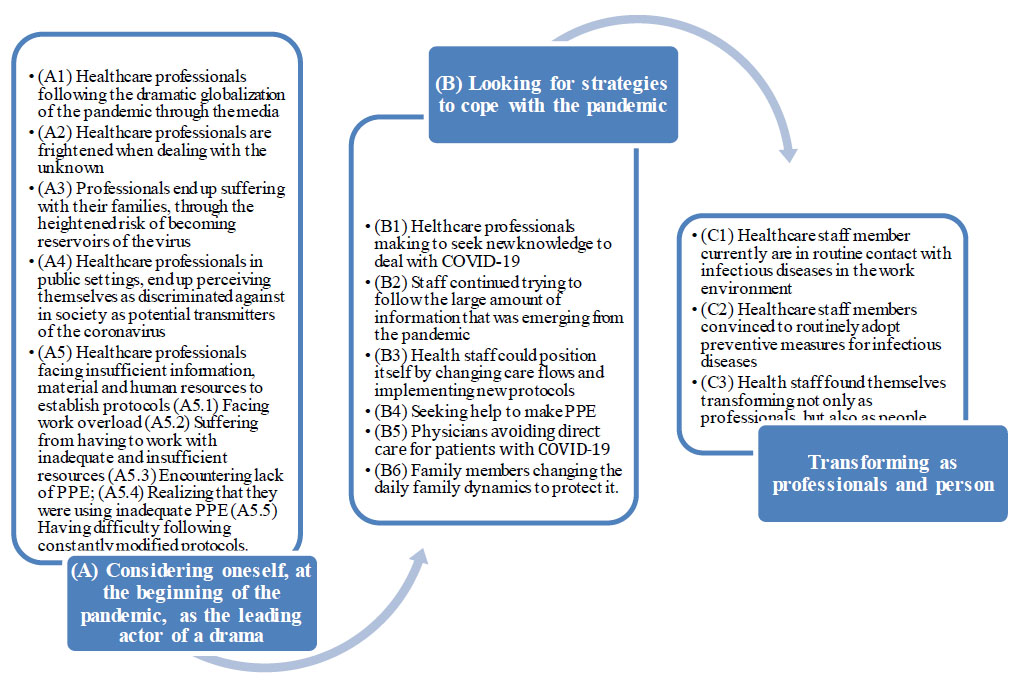
Core category (theoretical model) - From Dramatic Leading Role to Professional and Personal Improvement of Healthcare Staff in Emergency Services during the COVID-19 Pandemic. Central emergency room in the city of the state of Sao Paulo, Brazil, 2022.
| Subprocess | Categories | Subcategories |
|---|---|---|
| (A) Considering oneself, at the beginning of the pandemic, as the leading actor of a drama | (A1) Healthcare professionals following the dramatic globalization of the pandemic through the media | |
| (A2) Healthcare professionals are frightened when dealing with the unknown | ||
| (A3) Professionals end up suffering with their families through the heightened risk of becoming reservoirs of the virus | ||
| (A4) Healthcare professionals in public settings end up perceiving themselves as discriminated against in society as potential transmitters of the coronavirus | ||
| (A5) Healthcare professionals facing insufficient information, material, and human resources to establish protocols | (A5.1) Facing work overload | |
| (A5.2) Suffering from having to work with inadequate and insufficient resources | ||
| (A5.3) Encountering a lack of PPE | ||
| (A5.4) Realizing that they were using inadequate PPE | ||
| (A5.5) Having difficulty following constantly modified protocols | ||
| (B) Looking for strategies to cope with the pandemic | (B1) Healthcare professionals are making efforts to seek new knowledge to deal with COVID-19 | |
| (B2) The staff continued trying to follow the large amount of information that was emerging from the pandemic | ||
| (B3) Health staff could position itself by changing care flows and implementing new protocols | ||
| (B4) Seeking help to make PPE | ||
| (B5) Physicians avoiding direct care for patients with COVID-19 | ||
| (B6) Family members changing the family life’s daily dynamics to protect it | ||
| (C) Transforming as professionals and person | (C1) Healthcare staff members currently find themselves in routine contact with infectious diseases in the work environment | |
| (C2) Healthcare staff members were convinced to routinely adopt preventive measures for infectious diseases | ||
| (C3) Health staff found themselves transforming not only as professionals, but also as people |
Commotion began with healthcare professionals following the dramatic globalization of the pandemic through the media (A1), mainly in European countries such as Italy. The news broadcasted, the virus’s high transmissibility, healthcare service overload, a significant increase in deaths and contamination, and deaths of healthcare professionals. Following these news reports provides an emotionally exhausting experience with a disease that was yet to arrive but which was already generating suffering, such as fear, anxiety, and dread, portrayed in scenes in China and European countries, as reported:
[...] In the beginning, it was very hard for me. When it started around March here in Brazil, there was already news about what was going on in the world. It was right at the time when Italy was experiencing healthcare service overload, deaths at home, deaths and more deaths in hospitals, professionals being infected, and the media placing a lot of emphasis on this. This generated a lot of anxiety for us. I was very anxious, very insecure [...] (N4).
The virus continued to spread across the planet and reached Brazil, and healthcare professionals are frightened when dealing with the unknown (A2). They were in a state of continuous alert, given the need to quickly find ways to protect themselves from the threat that the new coronavirus posed to them, co-workers, and family. They state that:
[...] Responsibility increases every day, as we deal with an unknown disease, without proven medication for its treatment [...]. We are in the dark, trying to see the light at the end of the tunnel to cure our own family and friends [...] (P5). [...] In the beginning, we were a little lost, there were no protocols, there was no routine, and there was a huge lack of material, equipment, and Personal Protective Equipment (PPE) to work with [...] (T2).
Faced with the threat of the unknown and insecurities at work, professionals end up suffering with their families through the heightened risk of becoming reservoirs of the virus (A3). These professionals, as well as their families, spend their days in an emotional state, shaken by their awareness of increased exposure to the risk of them and their families becoming infected. Moreover, to protect them, some decide to adopt social isolation from their own families, as described:
[...] As for social life, lack of contact with family and friends who are not in the healthcare field was very hard, and we had to get used to it [...]. What affected me most was social isolation. Having to stay away from family and friends, as I am a potential transmitter [...] (T5). […] My family is very concerned; they are afraid of getting infected, and of me getting sick, and because of this, we are taking several precautions [...] (P1).
Furthermore, when healthcare professionals in public settings end up perceiving themselves as discriminated against in society as potential transmitters of the coronavirus (A4), according to a report:
[...] I have noticed that, from the moment we are identified as healthcare professionals, we are discriminated against as if we were transmitters of the disease. They think we are a source of contamination. That is wrong because the population takes much less care of themselves than us. They do not know about forms of prevention and dissemination [...] (N1).
With increased transmissibility and worsened cases, healthcare professionals face insufficient information, material, and human resources to establish protocols (A5). This category brings together five subcategories: facing work overload (A5.1); suffering from having to work with inadequate and insufficient resources (A5.2); encountering a lack of PPE (A5.3); realizing that they were using inadequate PPE (A5.4); having difficulty following constantly modified protocols (A5.5). They reported:
[...] A new outsourced staff was hired with completely unprepared people, and we had to provide support, and we continued to do so [...] (N2). With an entirely new and inexperienced staff, we must do our best to meet the increased demand, due to professionals arriving unprepared. [...] Equipment, such as respirators and monitors, was initially obsolete and old. Some were recovered, and others arrived new. This gave us a certain relief because we suffered in anticipation of imagining that this equipment could be insufficient, and we were afraid that the day would come to choose who would use it [...] (N3). [...] We suffered from a lack of PPE at the beginning of the pandemic, and this left us in a panic, and we ended up buying a lot of things to protect ourselves with money from our pockets [...] (N4). [..] The service is a little precarious due to low-quality inputs and PPE, as they are not recommended by ANVISA [...] (T5). [...] There were protocols and more protocols, and I had just read one, and another arrived, changing the previous one [...] (N2). [...] We were a little lost. In the beginning, there were no longer protocols and a routine for precautions, with a lack of material, equipment, and PPE to work with [...] (T2).
Looking for strategies to cope with the pandemic (B) is the second subprocess of the experience, which brings together actions to overcome stressful circumstances, which unfolds into six categories, from B1 to B6.
Faced with the need to improve care for patients affected by the disease, healthcare professionals are making efforts to seek new knowledge to deal with COVID-19 (B1), a movement to acquire technical-scientific knowledge to face the disease and minimize imminent risks, as reported:
[...] We had little training on offer, having to seek knowledge and work as multipliers with the staff. It was all new and uncertain [...] (N3).
Furthermore, due to the great emphasis given to the pandemic and the speed at which research was being conducted and new information emerged, such new information simultaneously generated some insecurity in the health staff regarding its reliability and whether it was being produced free of commercial and political interests. Thus, this staff continued trying to follow the large amount of information that was emerging from the pandemic (B2), as reported:
[...] What we were reading and watching was that it was milder than H1N1, but contagion was much faster, and we did not have a vaccine or specific medications for treatment. Several studies on vaccines and medications emerged some to use chloroquine and others to no longer use chloroquine, so this was generating more confusion and anxiety as we didn't know what and which study to consider [...] (N4).
New actions were necessary to face the pandemic so that the health staff could position itself by changing care flows and implementing new protocols (B3) as one of the strategies to structure health units to the new reality of COVID-19 so that an outbreak would not occur of the disease among patients and employees, as reported:
[...] Healthcare services had to adapt in a hurry, organize care flows, physical structure, develop protocols, all very quickly [...] (N4).
The disappearance of PPE on the market aroused fear and risk of contamination among professionals, and they mobilized themselves seeking help to make PPE (B4). This was the solution found, given the difficulty of purchasing and the scarcity of products in the market, which was also not prepared to meet the demand of a pandemic of this magnitude, as explained by the following confession:
[...] We had help from several groups of volunteers to make PPE and it was a movement that as touching. We managed to produce more than a thousand aprons and masks with donations and help from seamstresses. It was awesome! [...] (N4).
We saw physicians avoiding direct care for patients with COVID-19 (B5), especially among those who belonged to the risk group, seeking to protect themselves from the vulnerability of becoming a reservoir for the virus. Hence, many of them moved away from front-line care, ceasing to perform certain functions and some even refusing to work due to fear and insecurities, as reported:
[...] I am in the risk group and I took some measures to preserve myself, which was to leave the direct COVID-19 care area. Hospitals set up specific wards for COVID care and I did not volunteer to work in any of these places, and where we are now, in the Emergency Room, I stopped working as a clinician. I only had surgeon care as a measure to reduce the chance of directly treating a patient with COVID-19. I know that we will end up assisting and we already have, but it is part of our profession to assist people who are infected with a disease. I only avoided caring for those patients who have a high probability of being infected with COVID-19, so I opted for areas with less exposure [...] (P1).
However, frontline professionals caring for patients with COVID-19 who are concerned about the health of their family members find themselves changing the family life's daily dynamics to protect it (B6). These professionals gave up daily interaction with their families as a protective measure for them or changed to more careful habits with their clothes and footwear from their services so that they did not enter the house, advising their families to leave their homes ventilated. They reported:
[...] In my case, as I live with older adults and people at risk, I ended up leaving home to protect my family. I went to live with co-workers [...] (T2). [...] Removing shoes and clothing before entering the house to protect our home and loved ones [...] (P5). [...] We are avoiding very close contact, leaving the house well-ventilated, but this is the most we can do, living in the same house [...] (P4).
Moreover, as these healthcare professionals' experience progresses, from first going through great suffering to coping actions in the second moment, it contributes to the outcome of the experience so that those who remained on the frontline caring for COVID-19 patients saw themselves transforming themselves as professionals and person (C). This is the third subprocess of this experience, portrayed in professionals' ability to adapt to changes, overcome obstacles, and resist the adversities imposed by COVID-19 once the disease becomes part of routine work, as well as leaving lessons for continuity of professional practice and as a person. This subprocess groups three categories, from C1 to C3.
Staff members assess that, even in the difficult experience continuum, they managed to adjust to the situation that became part of their daily work routine. They had to forcefully adapt to using protocols which were not followed as preventive measures until then in their daily work to protect themselves from COVID-19. In this regard, experiencing the COVID-19 pandemic made staff members consider themselves in routine contact with infectious diseases. They recognized that, with the COVID-19 pandemic, they began to protect themselves more from occupational risks with infectious diseases. Moreover, healthcare staff members currently find themselves in routine contact with infectious diseases in the work environment (C1), stating that:
[...] It is not the first epidemic or a pandemic I am facing, as we have had others like H1N1 and SARS, but they did not have the repercussions on our city and region that the COVID-19 pandemic did. For me, it has become part of the routine of those who are in the healthcare system, and therefore, they must be prepared to face this type of situation sooner or later [...]. We are in direct contact with patients with infectious diseases who often do not tell us that they are infected, such as tuberculosis patients who we are in contact with without any protection. Now, in this pandemic, we are protecting ourselves from all patients potentially infected by COVID-19, trying to protect ourselves more and take more care in care than in other situations [...] (P2).
Furthermore, it is on the frontline of care for people with COVID-19 that healthcare staff members reflect on how much they failed to protect themselves from occupational risks with infectious diseases so that they were convinced to routinely adopt preventive measures for infectious diseases (C2) and, therefore, be more prepared for new endemics or pandemics, mainly due to the current ease that people have in moving between countries and continents, as described by P2:
[...] It is a new phase in people's lives in the modern world. We will increasingly face pandemics, diseases that will affect several countries and the entire world, due to people's commuting being much easier. It is very easy to travel from one country to another and from one continent to another, something that wasn't so common, and this makes it easier for diseases to spread more quickly around the world [...]. Anyone who is starting in the healthcare system now will go through other similar situations. I think it is a new phase in medicine dealing with infectious diseases, especially those of viral origin, which spread very quickly and easily [...].
Faced with the fragility of life exposed to the new coronavirus, the health staff found themselves transforming not only as professionals but also as people (C3). They began to value their experiences and everyday life more, as they report:
[...] It is an experience, a stressful period, but we are learning every day to value the things we have, always trying to live in the now because we do not know what tomorrow is like with this new disease [...]. On a personal level, it alerted us, and we began to see life differently, with different eyes. [...] (T3). [...] The most important factor was the behavioral change not only of healthcare professionals but of the population in general, so this will last, it will stay, and I believe it will improve other possible adverse situations like this, such as hand washing, more frequent use of PPE [...] (P3).
3.3. Discovering the Core Category
A core category was discovered through the reordering of the components (categories and subcategories) of the subprocesses, using a combination of techniques such as narrative, diagramming, classification, and review notes, as presented in Subsection 3.2. The central category proved to encompass all the components organized in the subprocesses, thus constituting the experience process entitled: From Dramatic Leading Role to Professional and Personal Improvement of Healthcare Staff in Emergency Services during the COVID-19 Pandemic (Fig. 1).
4. DISCUSSION
The disregarded theoretical model (process) of the emergency unit healthcare staff's interactional experience with the COVID-19 pandemic linked three subprocesses (A, B, and C), which signaled a positive outcome and promotion of a change in safety culture in the service regarding exposure to pathogenic agents. However, it shows how challenging it is for these professionals to adhere to standard precautions regarding the pathogenic microbiological world, invisible to the naked human eye. The experience learned shows that humans, even though they are healthcare professionals, begin to check the materiality/concreteness/existence of this microorganism when interacting with symbols relating to the signs and symptoms of disease active in individuals and, therefore, present in that scenario. SARS-CoV-2 in individuals progressed into severe, critical, and lethal forms. This makes us understand why non-symptomatic people contribute greatly to the virus spreading quickly. Changing a service's safety culture is understood as the sum of the understandings, attitudes, and behaviors of all employees about safety in the workplace, essential for the effectiveness of any worker health and safety program [13].
Experience shows that the health staff began to be aware of this change based on the insecurity and impotence resulting from interactions with media scenes before the pandemic arrived in Brazil, which were soon reproduced in their work. However, even so, these interactions were not enough to maintain a safe attitude. This only happened considering the experience, i.e., the concrete lethality of SARS-CoV-2 in severe and critical forms of COVID-19 for patients, healthcare professionals, and family members. Furthermore, these feelings were exacerbated when they were faced with insufficient information, material, and human resources to establish protocols.
It was in the symbolic interaction with the concreteness of the risk of imminent death that this staff sought strategies for coping with the pandemic (subprocess B). This occurred so that they would reconfigure their self to the fact of perceiving themselves in continuous contact with infectious diseases at work, convincing them that, for their safety, extended to their family, they need to continue adhering to standard precautions, regardless of whether the COVID-19 pandemic has ended (subprocess C).
Furthermore, the model makes it possible to predict that, despite a positive outcome, to reduce contamination and deaths among healthcare professionals in new epidemics/pandemics, it is necessary to invest institu- tionally in strategies for training health staff skills in the technical-scientific dimensions of standard precautions and quantitative-qualitative material and human resources to face new epidemics/pandemics. Furthermore, it is essential to develop psychosocial resources to deal with the invisibility of pathogenic microorganisms, for which humans and healthcare professionals are not prepared. This deduction is based on the reestablishment of security awakened in subprocess C, resulting from A and B. These point to staff moving towards coping strategies (subprocess B) after considering themselves, at the beginning of the pandemic, as actors in a drama (subprocess A).
In Symbolic Interactionism, the self is a social object about which actors act and, like all social objects, is (re)defined in interaction as new experiences are experienced. Hence, definitions and judgments are highly dependent on social definitions that actors encounter during their lives [10].
Symbols belong to a social class to represent something and, to be symbolic, actors manipulate symbols in their interactions, and the mind is the symbolic interaction of humans with their self. The mind is the action that uses symbols and directs them to the self. It is individuals trying to do something, to act in their world, i.e., the world is transformed into definitions because of the mind. Action is a response not to objects but to individuals' active interpretation of those objects [10].
It is known that using standard precautions contributes to reducing unnecessary risks associated with health and, consequently, to an organizational safety climate in compliance with recommended measures. Furthermore, the availability of the correct staff and materials, leadership, and training of healthcare professionals, patients, and visitors/companions are essential to increase this climate of safety in healthcare services [6].
It is also important to highlight the role of Standard Operating Procedures as management instruments that must be constructed together with the staff, aiming at standardized care for patients based on evidence-based practice, subsidized by continuing education in health and not in occasional activity. This process allows profes- sionals to develop security for care, convinces them that the institution is concerned, and makes it favorable to develop a culture of safety in healthcare environments. In this process, it is of structural importance to adapt facilities in terms of human and material resources, both quantitative and qualitative, to develop interventions in nursing professionals' daily practice [14].
Furthermore, understanding experience and a disregarded model by this study point to other devastating effects of the COVID-19 pandemic, now on interpersonal and, consequently, psychosocial relationships, not only on the general population but on healthcare professionals as actors in this research who worked in emergency and urgent services with direct care for patients.
These professionals experience challenges in both their personal and professional lives. They not only have to alter the dynamics of their family life due to their anxieties and the concerns of their loved ones, but they also face societal stigma when people recognize them as healthcare professionals and potential carriers of the virus.
According to Symbolic Interactionism, human action arises from interaction with the self and with the other/others, and when we interact, we become social objects for each other. We use symbols, direct ourselves, engage in mental action, make decisions, change directions, share perspectives, define reality and the situation, and even play the role of the other [10].
Hence, healthcare professionals, as part of this society, also configured themself by symbolically recognizing themselves as reservoirs and potential transmitters of the virus. Consequently, they consider themselves at risk for spreading the microorganism when interacting with their family members, co-workers, and wherever they travel. Thus, healthcare professionals defined themselves in the context of interactions at work, with family members, and in public settings as a social object symbolically represented as a reservoir and potential transmitter of the SARS-CoV-2 virus; therefore, they could easily perceive themselves as discriminated against outside of work.
Stigma is considered a harmful structural force that devalues members of groups that have undesirable characteristics. As stigma is created and reinforced by society through social interactions, researchers explored it related to the new coronavirus, initially after the US president pronounced it on March 16, 2020, as “Chinese virus” or “China virus”. The results show that this stigma is perpetuating [15].
These authors also emphasize that, similarly, stigmatization related to persons affected by the contagious disease included family members, caregivers, and friends who are in contact, in addition to frontline healthcare professionals and COVID-19 treatment centers. They warn of harmful and unfavorable results in the psychosocial sphere, extended to the public health system due to non-adherence and distrust of this potentially stigmatized population, which increases the risk of transmissibility and makes contact tracing and case monitoring difficult [15].
An ethnographic study on social discrimination and stigma in the community of healthcare professionals in Athens, Greece, during the COVID-19 pandemic, pointed to the main emotions experienced by healthcare professionals when they were transferred to COVID-19 clinics, such as fear, anxiety, anguish, anger, and insecurity. These feelings became worse when the family environment treated them with fear and hesitation. Their social environment tended to shun them, leading them into a state of self-isolation [16].
This study concluded that healthcare professionals faced discriminatory behavior and, therefore, were stigmatized both by their families and social environment and by other healthcare professionals. Faced with this scenario, government officials struggled to deal with the situation, maintaining a balance between healthcare professionals' safety and well-being, as they were not prepared for a pandemic of such magnitude [16].
With similar concerns, institutions came together (CIFRC, UNICEF, and WHO) to develop a guide to prevent and treat social stigma and discriminatory behaviors towards people with certain ethical backgrounds as well as against anyone who has had contact with the virus. This material associates the level of stigma with three main factors: 1) it is a new disease for which there are still many unknowns; 2) we are often afraid of the unknown; and 3) it is easy to associate this fear with others [17].
According to the institutions proposing this guide, it is understandable that there is confusion, anxiety, and fear among the public. Unfortunately, these factors also fuel harmful stereotypes. The evidence clearly shows that stigma and fear around communicable diseases make it difficult to respond. What works is building trust in reliable health services and advice, in addition to showing empathy with those affected, understanding the disease itself, and adopting practical and effective measures to keep themselves and their loved ones safe [17].
A limitation of this study was the fact that the healthcare staff's experiences from other emergency and urgent services were not involved, but as data collection took place during the beginning of the pandemic, access to other services was difficult.
One of the contributions of this research was to highlight the need for effective global policies to benefit mental and physical health and preserve healthcare worker safety when new epidemics/pandemics are assumed, especially for nursing staff members, as they are the most affected.
CONCLUSION
The initially proposed objectives were achieved, enabling the understanding of the health staff's experience at the beginning of the COVID-19 pandemic. The model indicated a staff waking up to occupational risks with pathogens in the interface with symbols of the devastating and dramatic concreteness of the SARS-CoV-2 virus and insufficient informational, material, human, and psychosocial resources, encouraging them to use standard precautions even after the pandemic.
Through this theoretical model, it is possible to predict that adopting policies that keep staff on the frontlines of endemic diseases and pandemics prepared with informational, material, and people resources could be a strategy to be operationalized to provide safety to these professionals and in the future reduce suffering and rates of mortality in similar experiments.
AUTHOR’S CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ANVISA | = Brazilian National Health Regulatory Agency |
| CIFRC | = Reference Centre for Psychosocial Support |
| COREQ | = Consolidated criteria for Reporting Qualitative research |
| GT | = Grounded Theory |
| N | = Nurse |
| P | = Physicians |
| PAC | = COVID-19 Centre |
| PAHO | = Pan American Health Organization |
| PPE | = Personal Protective Equipment |
| PSMC | = Central Municipal Emergency Room |
| RUE | = Emergency and Urgent Network services |
| SARS | = Severe Acute Respiratory Syndrome |
| T | = Nursing technician/assistant |
| UNICEF | = United Nations International Children's Emergency Fund |
| WHO | = World Health Organization |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was assessed and approved by the Research Ethics Committee of Centro Universitário Sagrado Coração (UNISAGRADO) under CAAE 31786420.0.0000.5502 and Opinion 4.036.507,Sao Paulo, Brazil.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Data were collected after research participants signed the informed consent form.
AVAILABILITY OF DATA AND MATERIALS
This article comes from a master's thesis, deposited in full in the Institutional Repository of the São Paulo State University (UNESP), link: https://repositorio.unesp.br/items/ea8fbe5a-6aaf-4281-93c5-3d1696771e96.


