All published articles of this journal are available on ScienceDirect.
Facebook Challenge: Integration of Breastfeeding for Sick Babies and E-Training to Enhance the Knowledge of Healthcare Workers
Abstract
Background
Although the Thailand Breastfeeding Center has supported breastfeeding for sick babies since 2014, it has been found that breastfeeding in infants is still 40% lower than national targets.
Objective
This research aimed to test the effectiveness of online breastfeeding training through social media to further the knowledge of healthcare workers.
Methods
A quasi-experimental research study of a sample group of 60 workers was conducted between the neonatal step-down unit and the postpartum care unit. Research instruments consisted of breastfeeding e-training through a Facebook platform, knowledge testing on the breastfeeding of sick newborns, an online training satisfaction assessment form, data analysis by frequency and percentage, averaging, and testing by t-test, chi-square, and the Fisher exact test.
Results
The mean and standard deviation of knowledge before training in the experiment and control group were 22.40±2.11and 23.43±3.32, respectively. After the intervention, the experimental group was 31.93±1.98, and the control group was 24.06±2.14. It was found that the average knowledge score pertaining to the breastfeeding of high-risk neonates in the group that had undergone online training was higher than the group that had undergone ordinary supervision (p< 0.001).
Conclusion
It can be seen that asynchronous e-training may be one alternative for the knowledge development of healthcare workers in promoting breastfeeding for families with sick newborns.
1. INTRODUCTION
Currently, the birthrate of premature infants worldwide is still quite high, estimated to be 11% of live births, numbering approximately 15 million annually. It is currently impossible to reduce this number below the specified target [1, 2]. In one case of premature infants, healthcare costs were as high as 1,680,000 baht per infant. These babies were later discharged from the hospital. It was then necessary to monitor their growth and development until they were two years of age [3]. In the past 15 years, the American Academic of Pediatrics has been systematically setting standards of care for high-risk neonates by putting emphasis on providing care to promote efficient breathing, promoting infant nutrition that is appropriate and age-based, pain management, prevention of infection and prevention of complications while undergoing care [4]. Currently, there are various guidelines to reduce mistakes made during procedures in the care of newborns with health problems. Examples include creating individualized care plans for premature infants to prevent respiratory failure (a bundle of care), as well as the use of technology in nursing to reduce errors in the administration of medication [5-9].
Nonetheless, the particular task of promoting the breastfeeding of premature infants and sick babies as a means of providing their optimum nutrition is difficult to achieve for a number of reasons. For example, primigravidas who do not have previous experience in breastfeeding, teenage mothers, inadequate electric breast pump supply and breastmilk expression after maternity leave, or some families with beliefs that pose obstacles to breastfeeding their premature children [7]. This plummets the breastfeeding rate of premature infants to only 28-40%. Accordingly, the American College of Nurse-Midwives (ACNM) recognizes breastfeeding as a sensitive issue that requires midwifery to play a vital role in the promotion and continuation of breastfeeding [8]. Nowadays, ACNM supports the practice of midwifery by promoting education and research, establishing midwifery as the standard of care. It has developed a comprehensive health education to support breastfeeding and facilitate the healthcare system to follow lactation friendly policies [9, 10]. While the Ministry of Public Health has stipulated that mothers should breastfeed their newborns to supply at least 50% of their total feeding and try to increase the rate of breastfeeding in order to meet the stated criteria by the year 2025 [11], it can be seen that the breastfeeding of premature infants in Thailand continues to be below 50%. One major reason is the lack of continuity in the milk expression and breastmilk collection and the long-term hospitalization of the child at the neonatal intensive care unit. This leaves the mothers with inadequate milk supply until their newborns are discharged while the healthcare staff, for its part, lacks the knowledge and skills it needs to help those mothers with premature infants by encouraging breastfeeding [12, 13]. This situation is consistent with the nature of professional development in the work of breastfeeding, where there is limited instructional media. There is a lack of any conveyance of information that is both concrete and thorough. Further, it is a consequence of organizing training sessions or academic conferences to enable a healthcare worker to promote breastfeeding of a sick newborn every two years while limiting the number of participants in each training session.
Moreover, the spread of the COVID-19 virus, which has been ongoing since 2019, has impacted the training or academic conferences in numerous places, forcing them to halt. As a result, professionals had less opportunity to access knowledge development. Meanwhile, providing nursing services is being offset by breastfeeding problems in the premature infants group that continue to occur almost every day. Public health is thus faced with a new challenge to find an alternative way to develop basic knowledge in its healthcare workers pertaining to the breastfeeding of sick babies.
It was found from a literature review that online training is one method that has been shown to be effective. It helps to increase one’s perspective and promote the ability of healthcare workers to carry out their duties properly and according to the standards [14]. Online training takes on several formats, including synchronous and asynchronous e-training, which have different advantages and disadvantages. Synchronous online training is similar to providing traditional face-to-face training. It is appropriate for the healthcare workers affiliated with hospitals.
Meanwhile, those working in a primary care hospital, such as general practitioners and practical nurses, will be subjected to time limitations, and the nature of their work will require them to provide services outside of their respective areas. Accordingly, the online training that would be appropriate for the workers in this group will have the features of asynchronous e-training [15]. For this reason, the researchers have applied an unlimited online training format, this time for use in their online training as a means of furthering knowledge in the area of breastfeeding in sick babies. About 90% of the healthcare workers strongly agreed that e-training saved their time and unlimited access. Currently, in Thailand, there is no online training available in the area of breastfeeding for sick babies, and there is the highest need to require e-training, second contraindication of medication during breastfeeding or lactation [16, 17]. After testing an online training system for the development of immunization workers in Thailand, a statistically significant increase in the average knowledge score of these workers was found, as opposed to those who underwent regular supervision [18]. Accordingly, the objective of this research was to study the effectiveness of an online training program designed to promote breastfeeding in sick newborns.
2. OBJECTIVES
This work aimed to study the effectiveness of an online training program designed to promote the breastfeeding of sick newborns on the knowledge scores of healthcare workers.
3. MATERIALS AND METHODS
3.1. Study Design & Setting
This research applied a quasi-experimental design with a two-group pretest-posttest design. This study was carried out at the Thammasat University Hospital, Thailand, where there is a baby-friendly hospital under the mother-child relationship project.
3.2. Sample & Sample Size Determination
The sample groups consisted of 30 workers, each selected by simple randomization. The inclusion criteria in this study included healthcare workers who performed breastfeeding services for families with sick babies and could use a basic smartphone. There was one exclusion criterion, namely, having previously passed the online breastfeeding training curriculum for healthy infants. The sample size was calculated using the G*Power 3.1.9.2 computer program [19], which has a power of 0.80 and stipulates a statistical significance level of 0.05 and an effect size (ES) of 0.5. This ES was obtained by calculating the research influence size pertaining to breastfeeding training [20], thus resulting in an ES = 0.82. The minimum sample group size was set at 24 to offset drop-outs from the sample group. It was, therefore, necessary to increase the sample group by 20% to compensate for the rate of attrition [21]. The present research thus required a total of 60 people for its sample group.
3.3. Data Collection
Once the volunteers had willingly agreed to participate in the program, the healthcare workers in the intervention group were handed an online training manual on the breastfeeding of sick babies. The instructions were provided on logging into the online system for self-study along with testing prior to class with a 35-question knowledge test on breastfeeding. The volunteers were allowed to independently select their study times, as the researchers opened the online system every two weeks to facilitate discussions and questions on any doubts they may have had pertaining to their online study. When the volunteers had completed three units of self-study by the end of week 8, the researchers then tested them for the knowledge they had acquired following their online learning and assessed their sense of satisfaction with the online system. Regarding the healthcare workers who participated in the control group, they underwent regular supervision in their work of providing breastfeeding services. They kept their appointments to test their knowledge of breastfeeding in week 1 and week 8, together with the intervention group. While testing the online training program, the researchers exclusively allowed the entry of the intervention group into the training system but did not allow the control group to enter the online training system until after week 8. Detailed participant recruitment is presented in Fig. (1).
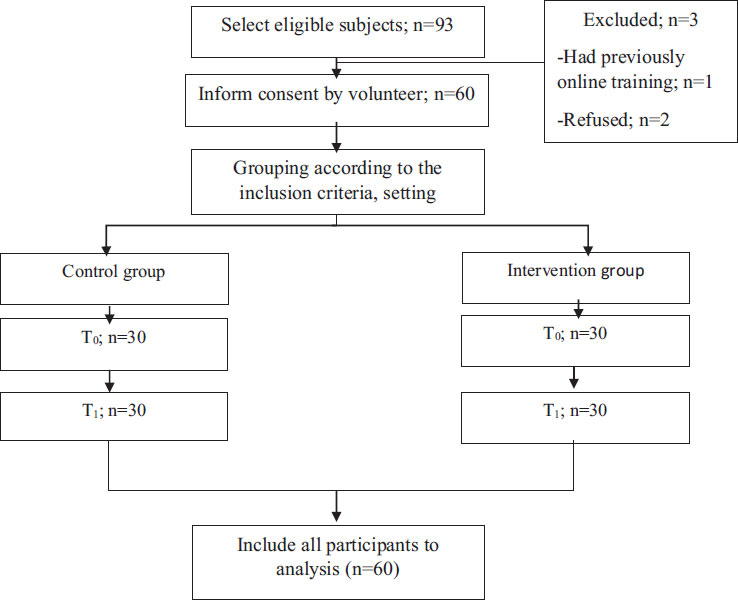
Note: T0=Before intervention, T1= 8-week after online training.
3.4. Intervention: Online Training System on the Breastfeeding of Sick Babies
This intervention was created by researchers based on a literature review and research related to the subject of breastfeeding in sick babies by following the ADDIE principles of digital media development [22] and the ‘10-step breastfeeding in sick babies’ concept of Spazts (2004) [23]. The aforementioned program was posted on the online social media platform Facebook for education and consisted of three learning units. Each learning unit was checked for content validity by five experts who evaluated a net content validity index of 0.96. When tested for their feasibility by five breastfeeding personnel, improvements were found in their language, content, and imagery, so they were easy to understand prior to their actual use.
3.5. Instruments
The Breastfeeding of Sick Babies knowledge questionnaire was developed from a review of the literature by Spazts (2004) and Al-Hially (2010) [23, 24]. The questionnaire consisted of 35 true-false questions. The content validity index of this instrument was 0.88. After being tested with ten members from the sample group, it was then used to calculate the reliability of this tool set by using Cronbach’s alpha coefficient at a level of 0.05, which was found to be 0.66
The satisfaction of the online training system questionnaire was based on the social media satisfaction evaluation form for breastfeeding by Kaewsuk et al. (2022) [25]. It consisted of 23 items arranged on a 5-point Likert scale. The total scores ranged from 23 to 115, with higher scores indicating higher satisfaction with the online training system. The content validity index of this questionnaire was 1.00, and the Cronbach’s alpha coefficient was 0.90.
The demographic datasheet record consisted of personal data of the workers, including age, current job position, experience in providing breastfeeding services, and other online training.
3.5. Data Analysis
The demographic data were reported in terms of means and percentages. The analysis of the difference in knowledge before and after online learning was carried out by the independent t-test, while other personal information of the two groups was analyzed by Chi-square and Fisher’s exact test. Additionally, satisfaction with the online training system was analyzed through descriptive statistics with averages.
3.6. Ethical Considerations
This research program was approved for its ethical standards by the Human Research Ethics Committee in the Field of Science of Thammasat University (TUEC 058/2022). All participants were informed of the research objectives, research protocol, and significance of the research before the intervention. They had the right to be involved in and withdraw from the study voluntarily at any time.
4. RESULTS
A total of 60 healthcare workers participated in this research program. The characteristics of the intervention group and those of the control group are shown in Table 1. All the characteristics between groups had no significant differences.
| Variable | Control (N = 30) |
Intervention (N = 30) |
t | p-value |
|---|---|---|---|---|
| Number (%) | Number (%) | - | - | |
| Age (M±SD) | 30.27±5.67 | 29.87±7.06 | 0.242 | 0.810 |
| History of breastfeeding service experience | - | - | - | - |
| No | 23 (73.7) | 27 (90) | - | 0.166a |
| Yes | 7 (23.3) | 3 (10) | - | - |
| Length of time of service for breastfeeding promotion (M±SD) | 4.33±3.59 | 5.07±3.72 | -0.776 | 0.441 |
| Educational level | - | - | - | - |
| Less than a diploma or a diploma | 5 (16.7) | 7 (23.3) | - | 0.648b |
| Bachelor’s degree | 24 (80) | 21 (70) | - | - |
| More than or equal to a Master’s degree | 1 (3.3) | 2 (6.7) | - | - |
| Type of occupation | - | - | - | - |
| Registered nurse | 20 (66.7) | 23 (76.7) | - | 0.390a |
| Practical nurse | 10 (33.3) | 7 (23.3) | - | - |
| History of breastfeeding training experience | - | - | - | 0.438a |
| No | 16 (53.3) | 14 (43.3) | - | - |
| Yes | 14 (46.7) | 16 (56.7) | - | - |
| Type of professional development | - | - | - | 0.761a |
| Academic conference | 2 (6.7) | 1 (3.3) | - | - |
| On-the-job training | 5(16.7) | 8 (26.7) | - | - |
| In-service training | 6(20) | 4 (13.3) | - | - |
| Self-learning | 1 (3.3) | 3 (10) | - | - |
| History of e-training | - | - | - | - |
| No | 20 (66.7) | 23(76.7) | - | 0.390a |
| Yes | 10 (33.3) | 7 (23.3) | - | - |
| Knowledge Score | Baseline | Final Score | ||||
|---|---|---|---|---|---|---|
| M ±SD | t | p-value | M ±SD | t | p-value | |
| Control | 23.43±3.32 | 1.436 | 0.156 | 24.06±2.14 | 14.831 | < 0.001 |
| Intervention | 22.40±2.11 | - | - | 31.93±1.98 | - | - |
| Knowledge Score | Possible Range | Control | Intervention | p-value | ||
|---|---|---|---|---|---|---|
| Baseline M ±SD |
Final M ±SD |
Baseline M ±SD |
Final M ±SD |
|||
| Benefit of breastfeeding for sick babies | 0-13 | 9.80±1.84 | 10.96± 1.24 | 9.16±1.51 | 8.53 ±1.43 | < 0.001 |
| Benefit of breastfeeding for mother | 0-6 | 5.43±1.07 | 5.36±0.92 | 5.20±0.99 | 6.00 | < 0.001 |
| Breastfeeding precautions | 0-16 | 8.20±1.90 | 10.13± 1.99 | 8.03±1.58 | 14.96±1.12 | < 0.001 |
Table 2 demonstrates that the knowledge scores before training between groups were not significantly different (p > 0.01). At eight weeks, there was a significantly higher knowledge score in the intervention group, which had undergone the online training. The contrast between the two groups was found to be statistically significant (p < 0.001). When analyzing by aspect, it was found that awareness of breastfeeding precautions, or where the mother must be careful in breastfeeding, was higher than in the control group. An exception occurred in which the knowledge scores on the benefits of breastfeeding for sick babies in the control group were higher than in the intervention group, as shown in Table 3.
The overall sense of satisfaction of sample groups with their use of the online training system was at a very high level (M = 4.31). For the most part, they were quite satisfied with the content and objectives of the media with its academically principled accuracy and reliability (M = 4.31). Furthermore, it showed that online media could explain its content concisely and clearly. Nonetheless, the sample group suggested that the program should make some improvements in the integrity of the background colors and font characters for the sake of clarity in online learning (M = 4.20).
5. DISCUSSION
Given the impact of online training via Facebook at eight weeks of experimentation, it was found that the healthcare workers who received the online training achieved higher average scores on their knowledge of breastfeeding than the group receiving regular supervision (p < 0.001); it could be explained by the fact that online training was not subjected to time constraints and is a significant method that helps to foster the knowledge of breastfeeding in healthcare worker. These findings are consistent with previous studies demonstrating that vaccine-management online training impacted the knowledge and performance of immunization workers, and online training impacted the breastfeeding rate in healthy infants six months after training [12, 26]. Moreover, a literature review revealed that breastfeeding training programs have focused on all healthcare professionals who support breastfeeding. For instance, a lactation education program for resident obstetricians demonstrated improvements in knowledge and confidence [27, 28]. These findings reflect that training in work-related knowledge continues to be a necessity for professionals performing their duties since their body of knowledge is constantly changing [29, 30].
Nonetheless, although online training was widely popular in professional development during the past COVID-19 outbreak situation, some programs use online training as a communication channel for new knowledge and various practices in order to comply with standards in the care of service recipients. Every program must be based on motivating a learner of all ages to access the technology and to integrate it with the work of professional development thereafter [31-33]. Accordingly, this online training program on promoting the breastfeeding of sick newborns is being instilled into a variety of media in order to create an incentive for people to learn from it consistently. For the most part, content based on the concept of ten-step breastfeeding in sick babies has been transmitted through an interesting infographic and animation clip. Similarly, the digital media guidelines of Saeedi et al. (2021) have stated that good online training media should include explanatory content, infographics, and animations, which would help promote a better learning atmosphere than verbal explanations [2]. Hence, organizing programs to make them suitable to the content will help encourage the students to make their own decisions to study.
Furthermore, although knowledge development in the more conventional format of routine supervision has its strong point, the workers could not make direct inquiries about the problems they frequently encountered with the lactation nurses. Instead, they learned to solve their problems immediately on the job site. Therefore, it was a matter of developing expertise by transferring knowledge into practice [34]. As an example, setting up a forum of discussion to exchange knowledge about breastfeeding, together with periodically sending healthcare workers to attend online classes, results in a positive attitude toward acting to promote breastfeeding. A comprehensive view of this subject reveals that the breastfeeding rate during the first six months differed in regularity from the group whose members did not receive online training. This disparity was found to be statistically significant [35]. However, one unfavorable aspect was that the work was being supervised in a way that might focus on problems often found in families of premature infants and, thus, might be causing little content coverage based upon the 10-step ladder principle of encouraging the breastfeeding of sick babies. This finding is in line with the present research, in which it was found that the use of the traditional face-to-face technique resulted in people becoming accustomed to receiving information on the benefits of breastfeeding, affecting both the mother and sick newborns. The use of this method also resulted in knowledge test scores in week 8 that did not differ between the two groups. Moreover, in the breastfeeding networking group based on the mother-child bond, there has been a campaign to promote periodic breastfeeding from shortly before birth to just before discharge. In terms of guidelines for the breastfeeding of sick babies, the various contraindications that apply to a mother with sick babies are different from the healthy infants. Consequently, it was found from the research results that the group receiving online training had knowledge scores on the contraindications or limitations of the mother that were higher after their training than before their training, unlike the group that underwent regular supervision. Accordingly, all important contents of the online program on this occasion were in compliance with the 10-step ladder principle.
Moreover, Facebook was used as a medium for disseminating the entire body of knowledge by observing the 10-step ladder principle for mothers with sick babies. Thus, using Facebook for education and online training for professional development helps reduce the complexity of accessing e-training compared to learning management systems. For these reasons, the experimental (or intervention) group provided feedback to the online system, indicating a high level of satisfaction (M = 4.51), as well as satisfaction toward attending the training sessions without being constrained by time limitations. After completing their self-study per the training objectives, the practitioners were then able to participate in discussions and exchanges of problems they encountered while providing breastfeeding services. Our findings were congruent with previous study results, which showed a significant difference in breastfeeding knowledge after using the WeChat mini-program-based online intervention. Further, there was publishing courseware and quick responses for sharing breastfeeding experiences among the mothers of preterm infants [36].
Currently, online training, blending the internet with the classroom, is helping to foster a personal relationship between the student and teacher. Further, large-group online learning focuses mainly on content and is mostly used to review content or to practice various tests aimed at developing successful learning results, which the field of health sciences has adapted for its own use quite widely [37]. The developing nations, in particular, are now developing online training systems or specialized online study courses. A survey found that 64.50% of practitioners use the online training system because it benefits knowledge development in the practice of medicine. However, 71.10% are hesitant about their safety due to the attacks in the cyber world [38].
Consequently, a good instructional media design that can be used advantageously must consider the difficulty of logging into the online training system, including the protection of the personal information of the students as prescribed by law in the Computer Act. It also consider the readiness of the equipment to provide easy access to the system, and such equipment could be a computer or a cell phone. In addition, a content-layout design that would present the content in an interesting and easy-to-follow format for continuous learning must also be included [37].
CONCLUSION
It may be concluded that the online training system on breastfeeding sick babies through closed-system online social media affects the knowledge development of the healthcare workers, resulting in an increase by the eighth week. This knowledge increase is particularly notable in the area of contraindications or precautions regarding the behaviors of mothers breastfeeding their sick newborns. Accordingly, the workers should be supported and encouraged to access online training to promote breast feeding sick babies as it enriches the newborns with nutrition before being discharged from the hospital.
IMPLICATIONS FOR NURSING AND SUGGESTIONS
This new option of E-training should be implemented in the area of Breastfeeding Promotion for Sick Babies to increase the rate of breastfeeding in the vulnerable group. However, it should be noted that the E-training course does not improve breastfeeding promotion skills and attitudes. Thus, future research should explore the effect of E-training on the behavior and skills of healthcare workers for breastfeeding sick babies.
ABBREVIATIONS
| ACNM | = American College of Nurse-Midwives |
| ES | = Effect Size |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Human Research Ethics Committee of Thammasat University (Science) (HREC-TUSC) #COA No. TUEC 058/2022.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Participation in this study was voluntary, and informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.


