All published articles of this journal are available on ScienceDirect.
Model of Coping Mechanism of Adolescents with Parental Loss due to COVID-19: A Study using PLS-SEM Analysis
Abstract
Background
The COVID-19 pandemic in Indonesia has led to a significant increase in mortality, with the death toll reaching 161,000, the second highest in Southeast Asia. The province of DKI Jakarta alone has reported 12,531 deaths, with 60% occurring among individuals aged 31–50 years. This high mortality rate has profoundly affected the role of parents, leaving adolescents to face considerable social and psychological challenges. The loss of a parent due to COVID-19 can severely disrupt an adolescent’s life, leading to heightened stress and anxiety as they struggle to cope without parental support. This study aims to identify the factors influencing the coping mechanisms of adolescents who have lost a parent due to COVID-19 and to examine the associated symptoms of stress and anxiety.
Methods
This study employs an explanatory survey design, focusing on adolescents in DKI Jakarta. The sample comprises 516 adolescents, selected through purposive sampling based on the criterion of having lost a parent due to COVID-19. Data analysis is conducted using structural equation modeling (SEM) with partial least squares (PLS).
Results
The research findings indicate that 60.3% of the respondents were female adolescents, 90.1% were from low-income families, and 66.5% lived in nuclear families. Most adolescents had lost their fathers (71.9%), with 24.2% reporting traumatic experiences and 75.2% having endured the loss for more than 12 months. The coefficient of determination (R2) was categorized as strong, with a value greater than 0.67. Hypothesis testing of the inner model using path coefficients revealed the following significant relationships: 1) between focal stimulus variables, stressor assessment variables, and coping mechanism variables (p-value < 0.05); 2) between focal stimulus variables, stressor assessment variables, coping source variables, coping mechanism variables, and stress (p-value < 0.05); and 3) between focal stimulus variables, stressor assessment variables, and coping mechanism variables with anxiety (p-value < 0.05).
Conclusion
Practical recommendations are proposed to enhance adolescents’ coping mechanisms in managing stress and anxiety resulting from loss. These include developing effective coping strategies, providing training on coping mechanisms for loss, and offering counseling services. The model demonstrates a sufficiently strong interaction between triggering factors, coping mechanisms, and psychological impacts, which contributes to strengthening adolescents’ resilience to loss during this critical period.
1. INTRODUCTION
The COVID-19 pandemic has subjected adolescents to significant hardships and suffering, representing their first encounter with such a global crisis, leaving them uncertain about how to respond [1, 2]. The psychological consequences of the pandemic on adolescents are profound, as evidenced by studies such as [3, 4], which reported that 53.8% of adolescents experienced moderate to severe stress, 28.8% exhibited symptoms of moderate to severe anxiety, and 8.1% showed signs of moderate to severe depression. These findings align with the research conducted [5] on 586 adolescents, which revealed that 20% experienced anxiety, 16.7% experienced acute stress, and 6.2% experienced post-traumatic stress disorder (PTSD) during the COVID-19 pandemic. These data underscore the traumatic impact of the COVID-19 pandemic on adolescents.
The traumatic experiences faced by adolescents during the COVID-19 pandemic are driven by various factors, including separation from family during self-isolation, disharmonious family relationships, and significant concerns about the death of family members [6, 7]. Adolescents require familial support to cope with loss and maintain their mental well-being [8]. One of the most devastating aspects of the COVID-19 crisis was the sudden death of close family members, often denying the chance to say farewell. The loss of parents represents one of the most transformative experiences for children and adolescents [9, 10]. These three studies emphasize the profound trauma children often endure under critical conditions, especially when losing parents who serve as their primary support system. However, these studies have not fully explored the grieving process and sadness from the perspective of children, nor have they adequately addressed how such losses might alter their worldview.
Research indicates that the death of parents can have profound and long-term effects on adolescents, leading to outcomes such as traumatic grief, depression, poor educational performance, and a higher risk of unintentional death or even suicide compared to their non-bereaved peers [11, 12]. This aligns with research conducted on children with traumatic experiences two years prior due to natural disasters. Among these children, 43.1% reported emotional or anxiety-related issues, 46.9% experienced depression, and 47.3% exhibited reduced attention spans [13, 14]. This research highlights the phenomenon of delayed grief in adolescents who may appear outwardly normal but experience significant internal changes months after the loss, often becoming trapped in their thoughts without realizing it. This condition warrants further investigation to better understand the internal processes adolescents undergo when they experience loss but are unable to express it freely, in line with the loss theory by Kübler-Ross [15, 16].
The development of coping mechanisms in adolescents dealing with loss is based on three fundamental theories: Hildegard Peplau's interpersonal theory (1989) serves as the overarching framework for the research, Callista Roy's adaptation theory [17, 18] explains the adolescent adaptation process in facing loss, and Stuart Laraia's stress adaptation theory [19] describes the formation of adaptive coping mechanisms. The nurse’s role, as depicted in Peplau’s theory, begins with the orientation phase, where a relationship of mutual trust is established with the adolescent. This is followed by the working phase, which involves the development of coping mechanisms and culminates in the evaluation phase, where signs of stress and anxiety are assessed.
The focal stimulus is the main triggering factor for stress symptoms and adolescent anxiety to adapt quickly after the sudden and unexpected loss of a parent due to COVID-19. Adolescents are unprepared to face sudden loss, which can affect their psychological, physical, and social conditions [20]. In addition to the focal stimulus, the contextual stimulus further exacerbates its impact. This includes adolescent demographic factors, experiences related to loss, and other health histories that contribute to the overall stress response [21].
The residual stimulus refers to environmental factors that contribute to additional stress symptoms and anxiety. The impact of the residual stimulus is indirect but should be considered in the formation of coping mechanisms, such as academic achievement and household crowding. Focal, contextual, and residual stimuli can influence coping mechanisms when occurring simultaneously. Another crucial factor is stressor assessment, wherein adolescents evaluate and interpret the significance of losing a parent to COVID-19. This assessment involves understanding the event’s meaning in relation to their mental health, encompassing cognitive, affective, physiological, behavioral, and social responses.
Coping sources are necessary for adolescents to help resolve problems. Successful application of these strategies can enable adolescents to manage future challenges effectively. In this study, the identified coping sources include social support, health insurance, material assets (savings), personal ability (problem-solving skills), and positive beliefs about health services. A study conducted across various age groups showed that 46.4% of adolescents with loss-related stressors needed counseling, and 55.5% had received pharmacological assistance since the loss occurred [22]. Coping sources are crucial for adolescents because the sudden loss of a parent due to COVID-19 is a traumatic experience.
Coping mechanisms are cognitive and behavioral processes that regulate external and/or internal demands exceeding an individual’s resources [23]. For adolescents, coping with loss involves both cognitive and behavioral strategies to address stressors that arise when external and/or internal demands surpass their available resources [24, 25]. According to [25], coping is a process in which individuals attempt to manage the perceived difference between the demands and resources they assess in a stressful situation.
Coping mechanisms are executed in two ways: 1) problem-focused coping, where adolescents try to solve problems by making changes or taking some action. This coping aims to reduce the demands of a stressful situation or increase the resources to face it [26, 27]. Problem-focused coping is done with the hope of resolving long-term issues because adolescents believe their resources can change the current situation. 2) Emotion-focused coping includes thoughts and actions that alleviate emotional pressure, aiming to control emotional responses to stressful situations. Adolescents can manage emotional responses through both behavioral and cognitive approaches, which may include techniques such as memory alteration or distortion of reality [28].
Stress is a nonspecific body response to a need that arises at a particular time. Stress can increase the need for readjustment, while a stressor is a pressure that produces stress, whether positive or negative. World Health Organization (WHO) [29] states that stress is a reaction or response of the body to psychosocial stressors in the form of mental pressure or life burden [30]. It can be concluded that stress is the result of tension between an individual’s reaction to difficulties or challenges and their ability to handle and resolve the stressful situation.
Anxiety is a disorder associated with various negative consequences in terms of social and personal adjustment [31]. Furthermore, there is evidence indicating that adolescent anxiety disorders are not a temporary phenomenon and, if not addressed, will persist into the next developmental stage, adulthood [30]. Therefore, it is essential to identify adolescents with anxiety as early as possible and to provide them with appropriate interventions.
2. SUBJECTS AND METHODS
2.1. Study Design
Explanatory research with a cross-sectional approach involves the simultaneous collection of data on dependent and independent variables over a specific period [32, 33]. The dependent variables are coping mechanisms, stress, and anxiety. Independent variables are factors that form a dependent variable, such as focal stimulus: loss and grief; contextual stimulus: age, sex, family income, family type, number of losses, time of loss, and academic grade; residual stimulus: traumatic experience; and stress or assessment and coping source variables.
2.2. Setting
The research was conducted in Junior High Schools, Senior High Schools, and Vocational High Schools across five areas of DKI Jakarta: East Jakarta, Central Jakarta, West Jakarta, South Jakarta, and North Jakarta. The study was conducted for six months from January to July 2023.
2.3. Subjects
The sample in this study consisted of adolescents aged 12–19 years who had experienced the loss of a parent due to COVID-19 and were experiencing mild to moderate anxiety. The exclusion criterion was that the adolescent was either married or experiencing severe anxiety.
2.4. Sample Size
Researchers determine the sample size based on the relationship between variables using the Lameshow formula [33] to test the average hypothesis of one sample. The sample size is based on previous research regarding the effect of grief therapy on the psychological condition of adolescents who have lost their parents, as the same research [34], with a significance level of α = 5% (Zα = 1.64) and a power of 95% (Z1-β = 1.28). The expected means are μo = 1.87 and μa = 1.429. After accounting for a 10% non-adjustment response (NAR), the final sample size needed is 516 adolescents.
3. TOOLS
3.1. Focal Stimulus Questionnaire (loss and grief)
The loss questionnaire utilizes the Persistent Complex Bereavement Inventory (PCBI) [33] designed to assess loss symptoms, consisting of 16 items evaluated on a 5-point Likert scale ranging from 0 (none; not at all) to 6 (severe; almost every day). PCBI was tested on 30 respondents in the East Jakarta region, with all items declared valid, having values greater than the critical value (>0.367). PCBI was deemed reliable with a Cronbach's alpha of 0.904. The grief questionnaire employs the Grief Cognitions Questionnaire for Children (GCQ-C) for grieving children aged 8–18 years [35]. Scores on GCQ-C assess negative thoughts related to loss, impacting daily functioning. The questionnaire comprises 20 items on a Likert scale ranging from 0 (almost never) to 2 (always). All GCQ-C items were validated with values exceeding the critical value (>0.367) and demonstrated reliability with a Cronbach’s alpha of 0.912.
3.2. Stressor Appraisal Questionnaire
The stressor assessment instrument is derived from the Stress Appraisal Measure (SAM), initially developed as the same research [36, 37]. The primary purpose of this instrument is the anticipatory evaluation of the danger or benefit arising from a situation (loss of a parent), consisting of 28 items. The instrument uses a Likert scale with the following ratings: 1 (not applicable to the current situation), 2 (slightly applicable to the current situation), 3 (moderately applicable to the current situation), 4 (very applicable to the current situation), and 5 (extremely applicable to the current situation). All SAM items were deemed valid, with their values exceeding the critical threshold of 0.367. Additionally, the items demonstrated high reliability, with a Cronbach’s alpha of 0.928.
3.3. Coping Source Questionnaire
The coping sources consist of five indicators: social support, personal ability, health assurance, savings, and positive beliefs. Health assurance, savings, and positive beliefs are categorical and utilize the Guttman scale (1 = yes/available; 2 = no). The social support questionnaire employs the Multidimensional Scale of Perceived Social Support (MSPSS) [38]. MSPSS is an instrument designed to measure the perceived adequacy of social support experienced by children and adolescents facing challenging situations. The instrument comprises 12 items originating from three sources: family (4 items), friends (4 items), and significant others (4 items). The Likert scale is utilized with response options ranging from 1 (strongly disagree) to 7 (strongly agree). All MSPSS items are deemed valid with values exceeding the critical value (>0.367) and are declared reliable with a Cronbach's alpha of 0.838. Lastly, the personal ability questionnaire uses the Adolescent Decision-Making Questionnaire (ADMQ) to evaluate the decision-making concept undertaken by adolescents who have experienced the loss of a parent [39]. This instrument consists of 30 items using a 4-point Likert scale from 0 (not at all true) to 3 (almost always true). As for health assurance, savings, and positive beliefs, the Guttman scale is applied (1 = Yes, 2 = No). All ADMQ items are considered valid with values greater than the critical value (>0.367) and are declared reliable with a Cronbach’s alpha of 0.952.
3.4. Coping Mechanism Questionnaire
The coping mechanism consists of two indicators: problem-focused coping and emotion-focused coping. The questionnaire “The Problem-Focused Style of Coping (PF-SOC)” by [40] comprises 18 items, with each item rated on a Likert-type scale: 1 (almost never), 2 = (sometimes), 3 (often), and 4 (always). All PF-SOC items are declared valid with values greater than the critical value (>0.367) and are considered reliable with a Cronbach’s alpha of 0.944. The questionnaire “Emotional Approach Coping Items” consists of 15 items on a Likert scale: 1 (never), 2 (sometimes), 3 (often), and 4 (always). The questionnaire comprises two subscales: emotional processing and emotional expression. All Emotional Approach Coping Items are considered valid with values greater than the critical value (>0.367) and are declared reliable with a Cronbach's alpha of 0.912.
3.5. Stress Questionnaire
The Perceived Stress Scale (PSS) is a classic stress assessment instrument developed by [41, 42]. It is used to understand situations that affect feelings and stress in adolescents. The PSS consists of 10 items, with scores ranging from 0 to 40. It utilizes a Likert scale with positive questions (4, 5, 7, 8) scored inversely: 4 (never), 3 (almost never), 2 (sometimes), 1 (often), and 0 (always). All PSS items are confirmed as valid with values greater than the critical value (>0.367) and are declared reliable with a Cronbach’s alpha of 0.857.
3.6. Anxiety Questionnaire
The anxiety questionnaire uses the Zung Self-Rating Anxiety Scale/SAS instrument [43, 44, 45]. The ZRAS instrument consists of 20 questions, with details of 12 psychological questions and 8 physiological questions. The instrument uses a Likert scale with scores ranging from 1 to 4. A score of 1 indicates “never,” while a score of 4 signifies “almost every time.” The interpretation of scores on this questionnaire is as follows: A total score of 20–39 indicates “not anxious,” a score of 40–47 suggests “mild anxiety,” a score of 48–55 represents “moderate anxiety,” and a score of 56–80 signifies “severe anxiety.” The questionnaires for PCBI, GCQ-C, SAM, MSPSS, ADMQ, PF-SOC, PSS, and Zung were originally designed in English and then translated into Indonesian (the respondents’ native language). The questionnaires were sent to English-speaking professionals for review and revision to ensure alignment with the original content.
3.7. Ethical Consideration
The research received ethical clearance on February 21, 2023, under approval letter number KET-021/UN2. F12. D1.2.1/PPM.00.02/2023. Additionally, it received a research recommendation from the Special Capital Region Education Office of Jakarta, with letter number e-0087/HM.03.03.
Respondents were aged 12–19 years, and the study was conducted in a school setting, placing adolescents in the vulnerable group. Therefore, the researcher first sought permission from the Vice Principal for Student Affairs and the counseling guidance teacher to involve adolescents in the study. This involved explaining the research objectives, the potential impact of completing the questionnaires on respondents' emotions, the voluntary nature of participation, and the importance of understanding the information provided [46, 47]. With approval from the school, the researcher conducted a meeting with adolescents who met the inclusion criteria. During this meeting, the researcher explained the research and sought consent from the adolescent’s guardians to participate as prospective respondents [47]. Adolescents who agreed to participate in the study provided informed consent by signing a consent letter.
Eligibility criteria were determined using purposive sampling techniques, based on specific inclusion criteria for selecting respondents. Two screenings were conducted: the first to identify adolescents who lost their parents due to COVID-19, and the second to select those with mild or moderate anxiety. Adolescents who met these criteria provided written consent, documented through an informed consent form, after receiving an explanation from the researcher.
Researchers carefully monitored participants’ responses, as completing questionnaires about parental loss can trigger psychological effects such as resurfacing sadness and negative thoughts. Respondents experiencing these issues were ethically excluded from continuing the questionnaire. To address anxiety, these individuals were separated from the group and given the opportunity to discuss their feelings, understand the causes of their anxiety, and practice stress management techniques, such as effective deep breathing exercises.
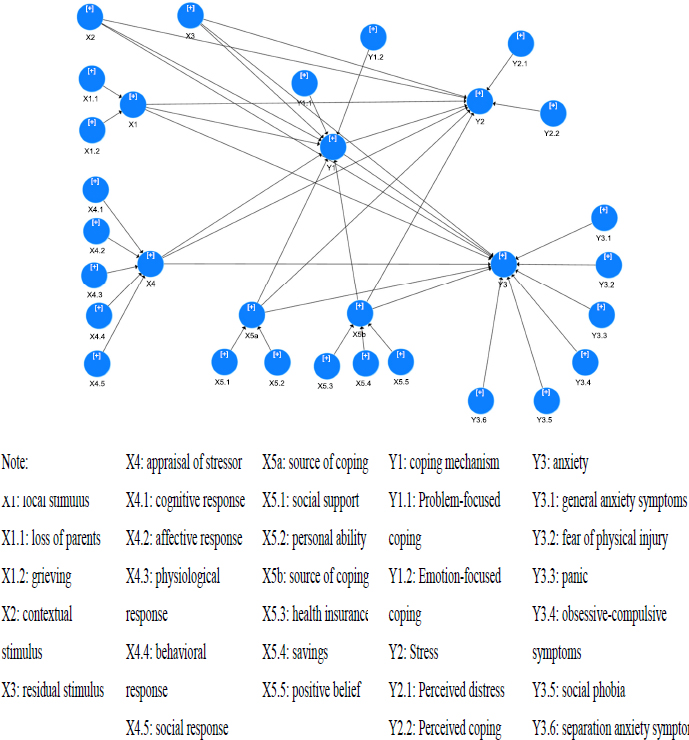
Research conceptual framework.
3.8. Data Analysis
After finishing collecting the data, the data is calculated and checked first, and editing, coding, data entry, and cleaning are performed so that the results are not biased. Descriptive analysis for categorical data is presented through frequency distribution, while numerical data is analyzed using measures such as mean, median, standard deviation (SD), minimum (min), and maximum (max). Inferential analysis was performed using partial least square (PLS) structural equation modeling (SEM). SEM aims to predict and test the relationship between variables, as well as to determine causality between variables. SEM can analyze multivariate statistics that are used to model the coping mechanisms of adolescents who have experienced the loss of a parent so that it can be seen that there is a relationship between variables in one conceptual model.
Analysis of sensitivity data in SEM-PLS does not ignore the outer loading results on each indicator that forms variables. A Waiver of outer loading provisions should be>0.6, which may lead to biased and inaccurate results. No data are lost because the sample is taken according to the inclusion criteria and has been added 10%.
4. RESULTS
The research framework is illustrated in Fig. (1).
4.1. Demographic Characteristics
Statistical results show that the majority of respondents were female adolescents aged 15–19 years, most of whom came from families with income below the DKI Jakarta (Regional Minimum Wage) namely IDR 4,901,798. The respondents mostly lived with their nuclear families, and the most common loss was that of a father, with a period of loss exceeding 12 months. Additionally, the adolescents reported no traumatic experiences or chronic illnesses (Table 1).
4.2. Measurement Model (Outer Model)
In structural equation modeling (SEM) methodology, the evaluation of the measurement model aims to predict the relationships between latent variables by assessing the validity and reliability of the model [48]. To test validity, there are two stages: convergent validity test and discriminant validity test. In confirmatory research, convergent validity is assessed by ensuring that the loading factors of each construct are greater than 0.6 and that the average variance extracted (AVE) is greater than 0.5.
4.3. Validity Test
As an initial step in data processing using the structural equation modeling method, validity testing is conducted on each indicator. The loading factor value is a measure of how well an indicator (item) measures the construct measured by factor analysis or factor analysis [49]. A loading factor value above 0.6 indicates that the indicator has a strong enough correlation with the measured factor and makes a significant contribution to measuring that factor. Based on this, for the subsequent analysis process, indicators of variables with a result of <0.6 will be deleted [50]. For an explanation of the loading factor values of each indicator, please refer to Table 2.
| Internal Risk Factor | - | Frequency | % |
|---|---|---|---|
| Age (years old) | 12–14 | 227 | 44 |
| 15–19 | 289 | 56 | |
| Sex | Male | 205 | 39.7 |
| Female | 311 | 60.3 | |
| Family income | Low (<Rp 4.901.798) | 465 | 90.1 |
| High(>Rp 4.901.798) | 51 | 9.9 | |
| Family type | Nuclear | 343 | 66.5 |
| Extended | 173 | 33.5 | |
| Number of lost parents | Dad | 371 | 71.9 |
| Mother | 135 | 26.2 | |
| Both | 10 | 1.9 | |
| Time of loss (month) | <12 | 128 | 24.8 |
| ≥12 | 388 | 75.2 | |
| Traumatic experience | No | 391 | 75.8 |
| Yes | 125 | 24.2 | |
| Academic grade | Increased | 245 | 47.5 |
| Decreased | 271 | 52.5 |
Table 2.
| Dimension | Variables | Indicator Description | Outer Loading |
AVE (>0.50) |
|
|---|---|---|---|---|---|
| Contextual stimulus | Age | - | Age | 0.194 | 1.000 |
| sex | - | sex | 1.000 | ||
| Family income | - | Family income | 0.148 | ||
| Family type | - | Family type | 0.014 | ||
| Number of losses | - | Number of losses | 0.289 | ||
| Time of lost parents | - | Time of lost parents | 0.021 | ||
| Academic | - | Academic | 0.805 | ||
| Medical history | - | Medical history | 0.423 | ||
| Order of children | - | Order of children | 0.032 | ||
| Focal stimulus | Loss | K1 | I feel a continuous longing for the deceased. | 0.600 | 0.995 |
| K2 | I experience deep and emotional sadness. | 0.694 | |||
| K5 | I find it hard to accept death. | 0.749 | |||
| K6 | I have disbelief about the loss. | 0.738 | |||
| K8 | I feel bitter or angry due to the loss. | 0.753 | |||
| K9 | I blame myself for the death of the deceased. | 0.720 | |||
| K11 | I wish to die to be with the deceased. | 0.700 | |||
| K12 | I find it difficult to trust others. | 0.712 | |||
| K13 | I feel alone or separated from others. | 0.717 | |||
| K14 | I believe that life is meaningless without the deceased. | 0.720 | |||
| K15 | I'm confused about my role and identity since the loss. | 0.698 | |||
| Grief | B1 | Since the loss, I consider myself weak. | 0.722 | ||
| B2 | I feel useless to anyone. | 0.774 | |||
| B3 | I think the world is bleak after their death. | 0.724 | |||
| B4 | I believe the world is no longer valuable after my parents' death. | 0.776 | |||
| B9 | I'm unsure about the future without parents. | 0.683 | |||
| B15 | My life seems to have little to offer. | 0.707 | |||
| B16 | My life feels worthless after my parents' death. | 0.809 | |||
| B17 | Sometimes I think something is wrong with me because I'm very sad about my parents' death. | 0.631 | |||
| Residual stimulus | Traumatic experience | - | Traumatic experience | 0.721 | 1.000 |
| Appraisal of stressor | X4.1 Cognitive response | Kog1 | This situation is truly hopeless. | 0.745 | 1.000 |
| Kog2 | This situation cannot be controlled by anyone. | 0.730 | |||
| Kog10 | This situation has long-term consequences for me. | 0.772 | |||
| Kog11 | This loss has a negative impact on me. | 0.706 | |||
| X4.2 Affective response | A3 | This situation makes me anxious. | 0.815 | ||
| A1 | This loss situation threatens my life. | 0.854 | |||
| X4.3 Physiological response | F1 | This loss makes me tense. | 0.822 | ||
| F3 | I am eager to overcome this situation. | 0.850 | |||
| X4.4 Behavioral response | Per2 | I can handle this situation. | 0.709 | ||
| X4.5 Social response | S6 | The problem of this loss cannot be solved by anyone. | 0.828 | ||
| S7 | I can overcome the problem of this loss. | 0.844 | |||
| Coping source | X5.1 Social support | DS3 | Family really helps me. | -0.875 | 0.983 |
| DS4 | I get moral help and support from my family. | -0.842 | |||
| DS11 | I can talk about problems with my family. | -0.802 | |||
| DS8 | Family is willing to help me make decisions. | -0.799 | |||
| X5.4 Personal ability | KD17 | I avoid making decisions. | 0.802 | ||
| KD18 | I postpone making decisions. | 0.789 | |||
| KD19 | I prefer to ask others to make decisions. | 0.767 | |||
| KD20 | I prefer to let others make decisions. | 0.739 | |||
| KD26 | When forced to make a decision, I can't think. | 0.605 | |||
| Coping mechanism | Y1.1 Problem-focused coping | MK_M7 | I'm busy thinking about problems and stressing about certain aspects. | 0.764 | 1.000 |
| MK_M9 | My past feelings hinder problem-solving. | 0.674 | |||
| MK_M14 | I'm carried away by emotions to assess and overcome problems. | 0.729 | |||
| MK_M16 | I have difficulty concentrating on my problems. | 0.736 | |||
| Y1.2 Emotion-focused coping | MK_E4 | I realize that my feelings are true and important. | 0.649 | ||
| MK_E5 | I let my feelings out freely. | 0.753 | |||
| MK_E6 | I take time to express emotions. | 0.801 | |||
| MK_E7 | I allow myself to express emotions. | 0.831 | |||
| MK_E8 | I feel free to express emotions. | 0.772 | |||
| Stress | Y2.1 Perceived distress | PD1 | I get angry at unexpected things. | 0.842 | 1.000 |
| PD2 | I feel unable to control important things in my life. | 0.821 | |||
| PD3 | I feel restless and pressured. | 0.836 | |||
| PD5 | I feel unable to complete things I should do. | 0.739 | |||
| Y2.2 Perceived coping | PC2 | I get angry because of problems I can't control. | 0.815 | ||
| PC5 | I feel overwhelmed by accumulating difficulties, making it difficult to cope. | 0.894 | |||
| Anxiety | Anxiety | GA1 | Angry because of something unexpected | 0.749 | 1.000 |
| GA3 | I feel restless and depressed | 0.813 | |||
| GA5 | I felt like everything that happened was in line with my expectations | 0.728 | |||
| GA9 | I was angry because of a problem I couldn't control | 0.801 | |||
| GA6 | I felt unable to finish the things I was supposed to do. | 0.802 | |||
| Variables | Cronbach's Alpha | Composite Reliability (rho_a) | Composite Reliability (rho_c) | R-Square | R-Square Adjusted | Q2 |
|---|---|---|---|---|---|---|
| Focal stimulus | 0.901 | 0.903 | 0.918 | 0.997 | 0.995 | 0.424 |
| Contextual stimulus | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 0.268 |
| Residual stimulus | 0.063 | 0.064 | 0.679 | 1.000 | 1.000 | 0.008 |
| Appraisal of stressor | 0.565 | 0.569 | 0.821 | 1.000 | 1.000 | 0.424 |
| Coping source | 0.849 | 0.870 | 0.897 | 0.999 | 0.983 | 0.615 |
| Coping mechanism | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 0.409 |
| Stress | 0,663 | 0.671 | 0.815 | 1.000 | 1.000 | 0.575 |
| Anxiety | 0.855 | 0.865 | 0.893 | 1.000 | 1.000 | 0.362 |
The loading factor values for each construct forming the variables are in accordance with the required standard, with a loading factor of ≥0.6 [51]. This means that all analyzed data are valid, and the testing of validity and reliability can proceed. The reliability results for each construct can be seen in Table 3.
Based on Table 3, the AVE values of all constructs have a value of >0.5 so it can be concluded that all construct variables are valid [48, 52]. The variables focal stimulus, contextual stimulus, residual stimulus, stressor assessment, coping source, coping mechanism, stress, and anxiety were influenced by strong outcome categories by exogenous variables with an R-square value of >0.6. There is a diversity of independent variables (focal, contextual stimulus, residual stimulus, stressor assessment, coping source) that can provide all the information needed to predict the dependent variable (coping mechanisms, stress, and anxiety). For example, focal stimuli were able to provide information about other variables, such as contextual stimuli, residual stimuli, stressor assessments, coping sources, coping mechanisms, stress, and anxiety by 99.7%.
The variables focal stimulus, stressor assessment, coping source, coping mechanism, stress, and anxiety demonstrate strong predictive relevance, as indicated by a Q2 value greater than 0.35. In contrast, the contextual stimulus exhibits moderate predictive relevance, with a Q2 value between 0.15 and 0.35, while the residual stimulus has weak predictive relevance, indicated by a Q2 value of less than 0.15.
4.4. Hypothesis Testing and Discussion
Hypothesis testing is conducted by examining the P-value results from the inner model analysis. Using α = 5%, a hypothesis is accepted if the P-value is less than 0.05. If the resulting P-value is greater than 0.05, the hypothesis is rejected. The structural model in this study can be seen in Fig. (1), and the results of the hypothesis testing can be observed in Table 4.
| Path Analysis |
β- Values* (+/-) |
t- Statistics (>1.96) |
P-Values (<0.05) |
Results | Conclusion |
|---|---|---|---|---|---|
| X1. Focal stimulus → X4. Appraisal of stressor |
0.677 | 24.859 | <0.001 | Positive, significant | Hypothesis accepted |
| X1. Focal stimulus → X5. Source of coping |
-0.202 | 3.271 | <0.001 | Negative, significant | Hypothesis accepted |
| X1. Focal stimulus → Y1 Coping mechanism |
-0.208 | 3.777 | <0.001 | Negative, significant | Hypothesis accepted |
| X1. Focal stimulus → Y2. Stress | 0.306 | 6.644 | <0.001 | Positive, significant | Hypothesis accepted |
| X1. Focal stimulus → Y3. Anxiety | 0.117 | 2.456 | 0.014 | Positive, significant | Hypothesis accepted |
| X2. Contextual stimulus → Y2. Stress | 0.121 | 3.653 | <0.001 | Positive, significant | Hypothesis accepted |
| X2. Contextual stimulus → Y3. Anxiety | 0.334 | 10.669 | <0.001 | Positive, significant | Hypothesis accepted |
| X4. Appraisal of stressor → X5. Source of coping |
0.145 | 2.551 | 0.011 | Positive, significant | Hypothesis accepted |
| X4. Appraisal of stressor → Y1. Coping mechanism | 0.340 | 6.590 | <0.001 | Positive, significant | Hypothesis accepted |
| X4. Appraisal of stressor →Y2. Stress | -0.146 | 3.132 | 0.002 | Negative, significant | Hypothesis accepted |
| X4. Appraisal of stressor →Y3. Anxiety | -0.229 | 4.966 | <0.001 | Negative, significant | Hypothesis accepted |
| X5. Source of coping → Y1. Coping mechanism |
0.082 | 2.097 | 0.039 | Positive, significant | Hypothesis accepted |
| X5. Source of coping → Y2. Stress | -0.089 | 2.744 | 0.006 | Negative, significant | Hypothesis accepted |
| Y1. Coping mechanism → Y2. Stress |
-0.291 | 8.059 | <0.001 | Negative, significant | Hypothesis accepted |
| Y1. Coping mechanism →Y2. Anxiety | -0.265 | 7.086 | <0.001 | Negative, significant | Hypothesis accepted |
Hypothesis testing in this study employs path coefficient parameters, where P-values and confidence intervals are closely related. A relationship between the variables exists if the hypothesis test results show a path coefficient (β) greater than 0, a t-statistic greater than 1.96, and a significance level of 0.05 (95% confidence interval). If the P-value is ≤0.05, the hypothesis is accepted; if the P-value is greater than 0.05, the hypothesis is rejected.
4.5. Structural Model Evaluation (Inner Model)
The structural model can be evaluated by examining the path coefficient parameters. Here are the hypothesis tests raised in this study:
The statistical analysis of the relationship between the focal stimulus and contextual stimulus yielded a positive path coefficient value of 0.331, a t-statistic value of 9.250 (>1.96), and a P-value of <0.001 (<0.05), indicating that the hypothesis regarding the relationship between the loss factor and the focal stimulus can be accepted. For the hypothetical relationship between the focal stimulus and the appraisal of stressors, the test results demonstrated a positive and significant influence, with a β-value of 0.677, a t-statistic of 24.859 (>1.96), and a ρ value of 0.000 (<0.05). Therefore, the first hypothesis, which states “There is a significant influence between focal stimulus on adolescent stressor assessment and parental loss due to COVID-19” is accepted. The results showed a direct effect on other hypotheses, where the focal stimulus (X1) had a negative and significant effect on the coping source (X5) with a β-value of 3.271, and on the coping mechanism (Y1), with a β-value of 3.777 (Table 5).
| Hypothesis | Original Sample (O) | Sample Mean (M) | Standard Deviation (STDEV) | t-Statistics (|O/STDEV|) | P-value | Significance |
|---|---|---|---|---|---|---|
| X2.S. Contextual → X1.S. Focal → X4. Appraisal of stressor | 0.244 | 0.226 | 0.026 | 8.544 | <0.001 | Significant |
| X2.S. Contextual → X1.S. Focal → X3.S. Residual | -0,045 | -0,044 | 0,019 | 2,416 | 0,016 | Significant |
| X2.S. Contextual → X1.S. Focal → X5. Source of coping | -0.067 | -0.069 | 0.023 | 2.865 | 0.004 | Significant |
| X2.S. Contextual → X1.S. Focal → Y1. Coping mechanism | 0.069 | 0.069 | 0.020 | 3.426 | 0.001 | Significant |
| X1.S. Focal → X4. Appraisal of stressor → Y1. Coping mechanism | 0.231 | 0.232 | 0.036 | 6.373 | <0.001 | Significant |
| X2.S. Contextual → X1.S. Focal → Y2. Stress | 0.101 | 0.102 | 0.019 | 5.355 | <0.001 | Significant |
| X1.S. Focal → X4. Appraisal of stressor → Y2. Stress | 0.099 | 0.098 | 0.032 | 3.052 | 0.002 | Significant |
| X4. Appraisal of stressor → Y1. Coping mechanism → Y2. Stress | -0.099 | -0.100 | 0.019 | 5.079 | <0.001 | Significant |
| X5. Source of coping → Y1. Coping mechanism → Y2. Stress | -0.024 | -0.024 | 0.012 | 1.999 | 0.046 | Significant |
| X2.S. Contextual →X1.S. Focal → Y2. Stress | 0.039 | 0.038 | 0.016 | 2.388 | 0.017 | Significant |
| X1.S. Focal → X4. Appraisal of stressor → Y2. Anxiety | 0.155 | 0.155 | 0.032 | 4.845 | <0.001 | Significant |
| X1.S. Focal → Y1. Coping mechanism → Y2. Anxiety | 0.055 | 0.055 | 0.017 | 3.399 | 0.001 | Significant |
| X4. Appraisal of stressor → Y1. Coping mechanism → Y2. Anxiety | 0.090 | 0.091 | 0.019 | 4.689 | <0.001 | Significant |
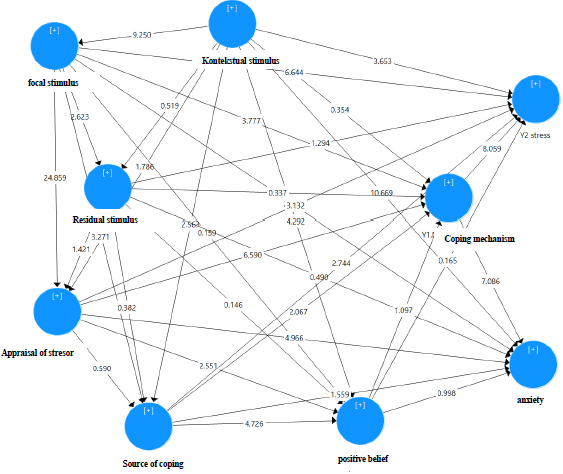
Inner model.
4.6. Final Research Model
After the estimated model meets the criteria of the Outer Model, the next step is structural model testing (inner model). The inner image of the model can be seen as shown in Fig. (2).
Based on the output image displayed in Fig. (2), the highest t-value that affects the formation of coping mechanisms in adolescents when parental loss occurs is the stressor assessment with a t-value of 6.590. This is followed by the focal stimulus, with a t-value of 3.777, and the coping source, with the smallest t-value of 2.097. Regarding the factors influencing the formation of adolescent stress following parental loss, the coping mechanism emerges as the most significant factor, with a t-value of 8.059. This is followed by focal stimuli, specifically loss and grieving, with a t-value of 6.644; the contextual stimulus (sex), with a t-value of 3.653; the stressor assessment, with a t-value of 3.132; and the coping source, with a t-value of 2.744. In terms of the factors influencing the onset of anxiety symptoms in adolescents following parental loss, the contextual stimulus (sex) is the most significant, with a t-value of 10.669. This is followed by coping mechanisms, with a t-value of 7.086; stressor assessments, with a t-value of 4.966; and the focal stimulus, with a t-value of 2.456.
5. DISCUSSION
The research results on the variable of focal stimulus factors (loss and grief) indicate that adolescents are still in the moderate range of scores, meaning that loss and grief still occur depending on the stressor experiences they encounter. Interestingly, the results of the loading factor of the PCBI loss questionnaire items show that adolescents still feel a continuous longing for the deceased, experiencing deep sadness and emotional pain due to loss, even though the research results indicate a history of loss of more than 12 months since the occurrence of COVID-19 in 2020–2022. Adolescents find it difficult to accept the death of their parents, feel disbelief or emotionally numb, and have a desire to die to be with the deceased. This is consistent with research conducted by [53, 54], which qualitatively reveals that memories of the deceased are deeply felt, adolescents are unable to meet the deceased for the last time, and funeral rituals are not conducted as usual. Another study [55, 56] found similar results that losing parents has a significant impact, leading to negative reactions such as denial, anger, and frequent denial when stressors occur. Based on this description, the threat of psychosocial problems after loss cannot be avoided. The sudden experience of loss due to COVID-19 is a first-time experience, and adolescents do not yet have effective coping mechanisms to deal with it.
Contextual stimulus factors have proven to be valid in influencing the formation of coping mechanisms, especially indicators of family type and traumatic experiences, as seen in the outer loading values. The majority of respondents lived in nuclear families where one or both parents died due to COVID-19. The loss of one or both parents results in an imbalance of roles in the family, as seen in Cait’s (2005) research that adolescents take on the role of caregivers to support living parents and replace the role of parents who have died. The sudden addition of the role of adolescents is not in accordance with their growth and development tasks, so adolescents must be able to adapt to the process of losing their parents. Economic needs become a primary topic when the head of the family dies. The economic condition of the respondents’ families is relatively low. The difficulty of the economic situation can influence adolescents’ views of the future. Traumatic experiences, such as previous parental loss, act as predisposing factors for adolescents to experience stress and anxiety. Another study states that the socioeconomic role of the left-behind family is heavy in influencing the development of children [57]. The loss of a father as the head of the family, a role model, and a decision-maker also affects the formation of adolescents’ coping mechanisms. Therefore, it is essential to delve deeper into the factors underlying adolescent stress and anxiety.
Adolescents’ academic scores have also decreased. Adolescents admit that academic demands at school are the biggest trigger for them. Adolescents are required to be able to excel and prepare themselves for college level to prove to the deceased the dreams that adolescents have achieved. The same research by [55, 56] shows similar results that environmental demands on adolescents’ success in academics is a factor that causes adolescents to experience stress and anxiety.
Most adolescents live in densely populated areas. A similar study conducted in Bangladesh measured the stress levels of adolescents living in crowded environments. The study found that 65% of adolescents experienced moderate stress due to living in crowded environments. Dissatisfaction with sleep quality is significantly related to stress symptoms. Symptoms of stress, such as feeling unable to control important things in life and decreased self-confidence, affect school academic performance. Housing density and academic grades represent conditions in which adolescents are vulnerable to stress, anxiety, and coping mechanisms.
The stressor assessment in this study is the largest independent variable influencing coping mechanisms, stress, and anxiety. Interesting items emerge from the outer loading results, where adolescents state that loss is a hopeless situation, creates tension, has negative impacts on adolescents, and cannot be controlled by anyone. The loss situation is interpreted as a threat to adolescent life because other problems arising from the loss cannot be solved by anyone. This result is in line with the study [57, 58] on adolescents in the Netherlands, which found that adolescents’ stressor assessments are influenced by cognitive or their understanding of their current problems and assess stressors as something to be solved, not avoided. Therefore, it is necessary to provide adolescents with an understanding of how to assess stressors effectively.
The coping resources that adolescents need to form adaptive coping mechanisms consist of social support, self-efficacy for health insurance, material assets, and positive beliefs about mental health services at community health centers. The results of this study show that the most significant social support comes from family and friends. Adolescents assess that social support and self-ability are still in the medium range, indicating that coping resources have not been fully achieved by adolescents. Similar results were also found in research conducted by [22], which revealed that the support received took the form of stronger emotional ties, the building of positive relationships, and a clear division of roles. However, a unique addition to this study is that adolescents require pharmacological assistance when their anxiety reaches severe levels. Based on this description, it is necessary to analyze what coping resources are needed to form a coping mechanism for dealing with the loss of a parent.
Adolescents use coping mechanisms when parental loss occurs in two ways: problem-centered coping and emotion-centered coping. Both methods are still in the moderate score range, indicating that they have not been maximally implemented. Based on the statistical results, the coping mechanism factor is a variable that plays a role in influencing stress and anxiety factors. A similar study was conducted [40, 58, 59] in Taiwan, explaining that adolescents use reflective, suppressive, and reactive coping strategies when solving their problems. In another study, adolescent’s problem solving by acknowledging emotions, letting feelings out freely, expressing emotions, and being free to express their emotions. Therefore, the coping mechanisms employed by adolescents in dealing with the loss of parents due to COVID-19 are not optimal, and efforts are needed to improve coping mechanism abilities.
CONCLUSION
To better understand the interaction mechanisms among the factors influencing coping mechanisms and symptoms of stress and anxiety, this research applied a quantitative method to test the mediating effects of coping mechanisms. After conducting validity and reliability tests, the collected data were further analyzed using structural equation modeling-partial least squares (SEM-PLS) to test the hypotheses. The final mediation model was constructed based on the compatibility of the analysis results, including focal stimuli, loss, and mourning influencing the formation of coping mechanisms. Among 12 contextual stimuli, only two, family type and traumatic experiences, formed coping mechanisms. The most significant impact on the formation of coping mechanisms comes from the assessment of stressors compared to other factors. Coping sources, such as social support and problem-solving experiences, play a role in the formation of coping mechanisms. Coping mechanisms, centered on both problem-solving and emotion, contribute to symptoms of stress and anxiety, and practical recommendations are made to enhance coping mechanisms and reduce symptoms of stress and parental anxiety in adolescents who have experienced parental loss.
The results of the study can be generalized to all provinces in Indonesia because DKI Jakarta is the capital of the country and represents all characteristics of adolescents in Indonesia. The tribes involved are from the islands of Java, Sumatra, Kalimantan, and Sulawesi. Research limitations: The number of samples that are not known from the data may affect the sampling process and the duration of the study.
Health center nurses are recommended to actively engage in the field, provide educational support, and address psychosocial issues such as stress and anxiety associated with loss.
FUTURE STUDY
Efforts to improve this study and mitigate potential biases, thereby enhancing the reliability of the findings, include the following:
1) A purposive sampling technique was employed to select suitable respondents.
2) Participants in the study were informed about the research objectives, data collection procedures, and confidentiality, which should reduce bias.
3) All questionnaire items were extracted and validated before distribution to the participants.
4) Validation and reliability testing of the data were conducted before hypothesis testing with a Cronbach’s alpha value of >0.6.
5) Structural equation modeling-partial least squares (SEM-PLS), as an advanced statistical method, was used to test multiple research hypotheses.
Therefore, the findings of this research should be considered reliable.
The mediating effects of coping mechanisms were confirmed in this study, but some findings may require further investigation. Future research is recommended to examine the differences between junior high school and senior high school adolescents regarding the formation of coping mechanisms and the symptoms of stress and anxiety. Other suggestions include exploring differences based on gender, and investigating whether male adolescents are more vulnerable to loss, which might increase their likelihood of experiencing stress and anxiety, or if the opposite is true.
AUTHORS' CONTRIBUTIONS
E.N, M, S.R.A, T.E contributed to the ideation, analysis, and writing of this manuscript, and D.L.T was assigned data collection. All authors have access to all children datasets. All authors have read and approved the published version of the manuscript.
LIST OF ABBREVIATIONS
| PTSD | = Post-traumatic Stress Disorder |
| WHO | = World Health Organization |
| NAR | = Non-adjustment Response |
| PCBI | = Persistent Complex Bereavement Inventory |
| SAM | = Stress Appraisal Measure |
| MSPSS | = Multidimensional Scale of Perceived Social Support |
| ADMQ | = Adolescent Decision-Making Questionnaire |
| PSS | = Perceived Stress Scale |
| SEM | = Structural Equation Modeling |
| AVE | = Average Variance Extracted |
| SEM-PLS | = Structural Equation Modeling-partial Least Squares |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research obtained ethical clearance on February 21, 2023, with approval letter number: KET-021/UN2. F12. D1.2.1/PPM.00.02/2023. This research also received a research recommendation from the Special Capital Region Education Office of Jakarta, Indonesia with letter number: e-0087 / HM.03.03.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIAL
All the data and supporting information is provided within the article.
FUNDING
This research was supported by a Research Grant from the University of Indonesia with the reference number: PENG-001/UN2.RST/PPM.00.00/2023.
ACKNOWLEDGEMENTS
Declared none.


