All published articles of this journal are available on ScienceDirect.
The Severity of Adverse Events is Associated with the Age of Hospitalized Patients: A Retrospective Study
Abstract
Background:
Adverse events (AE) are unintentional injuries or harm that occur during medical care. These represent a public health problem, and they are one of the main causes of death in the world.
Objective:
The objective of the study was to determine AEs derived from nursing care in hospitalized patients, as well as to estimate their frequency according to severity, follow-up, and type of care service.
Methods:
We undertook a retrospective study in hospitalized patients. EA by severity (no damage, irreversible damage, disability, and death), types (pressure ulcers (PUs), falls, phlebitis, and blood transfusion), and demographic data (age and gender) were taken into account. Damage severity was determined according to the guidelines of the Peruvian Ministry of Health.
Results:
We obtained 127 reports (55.9% women, mean age of 28+8 years). The main EA were PUs (57.5%), followed by phlebitis (20.5%) and falls (19.7%). Most of the AEs have been followed up, and almost all the AEs occurred during hospitalization. In addition, being older was associated with AE severity (p=0.002), as there were reports of 2 (1.6%) cases of death, and half of the cases resulted in the disability of patients > 48 years old.
Conclusion:
PUs were the most frequent AE. They affected younger patients, and their severity was associated with older age. It is important for health professionals to recognize and notify AEs in order to ensure the patients’ well-being; also, health institutions needs to be encouraged for improving their risk reduction programs.
1. INTRODUCTION
Adverse events (AEs) are injuries or any unintentional harm that occur during medical care, which are significant to a greater extent than the underlying pathology. They can occur during prolonged hospitalization or delayed discharge, and lead to health detriment, disability, or even patients’ death [1]. According to the World Health Organization (OMS), AEs are a public health problem as they are among the top 10 causes of death and disability worldwide and affect 4 in 10 patients during primary and ambulatory care [2].
In Latin America, during the Iberoamerican Study of Adverse Events (IBEAS), in 2007 and 2009, it was reported that every 10 patients admitted had an incident during their medical attention. In Peru, the project showed AEs to be related to a higher frequency of nosocomial infections (39.6%) and surgeries (28.9%). In addition, the services with the most prevalence were of Obstetrics and Intensive Care Unit (ICU), where 58.8% could have been prevented [3]. Similarly, in Spain, revisions of medical records revealed 39.6% of EAs to be surgery-related and 56.2% of the total to be preventable [4].
It is important to highlight that since nurses constitute the largest group in health facilities, they are involved in many complaints and claims related to care [5]. This information is relevant since it is estimated that 47% of ICU activities are planned, while 33% are reactive actions; thus, nurses are those who perform more interventions (84%) than physicians (4.7%) [6]. A study on health professionals’ perceptions (71.24% nurses) of AEs severity in Spain determined PUs to be the most important ones, with a percentage of 42.3%, followed by falls at 34.2%, and phlebitis at 23.5% [7]. A similar situation was described in Colombia, where PUs were the most common AE in 52.5%, phlebitis in 43.5%, and falls in 4.3% [1]. In Brazil, the most frequent AEs were found to be related to probes, drains, and catheters, with a prevalence of 61.36%, which could be considered to be related to phlebitis,; however, PUs accounted for 4.92% [8].
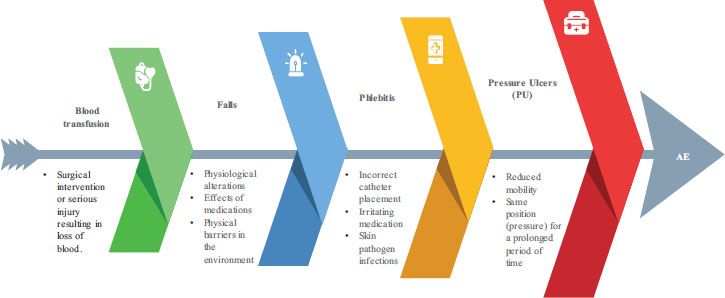
AEs are associated with a set of factors that determine their frequency (Fig. 1). It has been shown that the incidence of AEs is between 9.2% and 24.3%, depending on hospital type, size, and medical specialty. Another determinant factor is patient complexity, since critical patients’ services are the ones with the greatest number of AEs. These include coronary care units (18.1%), intensive care units (14.4%), and emergency departments (8.9%) [9]. Other studies have shown 40% of Aes to occur in surgical blocks; in Spain, at least 10.5% were reported to occur in general surgical services and 3% in major outpatient procedures [10].
In Peru, several studies [11-13] have estimated AEs frequency in specialist and inpatient areas; however, AE frequency is not reported in all healthcare settings, and nursing factors and care have not been associated with AE development. It is important to estimate the frequency, severity, and characteristics of AEs during hospitalization in order to assess the impact of AEs on hospitalization and improve the patient care processes.
Thus, the objective of the study was to determine the AEs derived from nursing care in Peruvian hospitalized patients. Furthermore, we sought to estimate the AE frequency by severity, follow-up, and healthcare service type.
2. METHODS
2.1. Study Design and Setting
We conducted a retrospective study with a quantitative approach on all the patients who attended the Hospital Nacional Dos de Mayo (Lima, Peru) in 2018. This tertiary hospital (category III-1) belongs to the Ministry of Health (MINSA). It provides medical care in all the medical and surgical specialties, and the hospital area has approximately 600 beds [14].
2.2. Population, Instruments, and Definition
Of the total hospitalized patients, 127 reports of AEs were recorded in the hospital database. An AE, according to MINSA 2015, is every accident that causes or could have caused harm to patients, and its severity is reported according to the grade of damage [15]. Grade 4 (when the death of the affected patient occurs), Grade 3 (when disability or permanent damage occurs), Grade 2 (when damage is reversible and/or generates a longer hospital stay), and Grade 1 (when no damage or alteration of the hospitalization has been generated) are the scales of the severity of AEs.
2.3. Variables, Data Processing, and Analysis
The variables reported include AE severity [15], type (pressure ulcers, falls, phlebitis, and blood transfusion), demographic data such as age and gender, and type of service. The data were recorded and tabulated directly using the SIGHOS (Hospital Management System) data exported to MS-Excel 2013 (Redmond, US) (Table 1).
| Variable | Category | Type of Adverse Event | - | p-value | |||
|---|---|---|---|---|---|---|---|
| PU | Falls | Phlebitis | Blood Transfusion | Total | |||
| Age group | 0- 11 | 5 (3.9%) | 1 (0.8%) | 3 (2.4%) | 1 (0.8%) | 10 (7.9%) | 0.001 |
| 12 -23 | 10 (7.9%) | 7 (5.5%) | 5 (3.9%) | 0 (0%) | 22 (27.9%) | ||
| 24- 35 | 32 (25.2%) | 11 (8.7%) | 11 (8.7%) | 1 (0.8%) | 55 (69.9%) | ||
| 36- 47 | 8 (6.3%) | 1 (0.8%) | 4 (3.1%) | 0 (0%) | 13 (16.5%) | ||
| 48- 59 | 9 (7.1%) | 1 (0.8%) | 3 (2.4%) | 1 (0.8%) | 14 (17.8%) | ||
| < 60 | 9 (7.1%) | 4 (3.1%) | 0 (0%) | 0 (0%) | 13 (16.5%) | ||
| Gender | Male | 57 (44.1%) | 2 (1.6%) | 11 (8.7%) | 2 (1.6%) | 72 (56.7%) | 0.072 |
| Female | 17 (13.4%) | 25 (18.1%) | 15 (11.8%) | 1 (0.8%) | 58 (45.7%) | ||
| Variable | Category | Type of Adverse Event | - | - | |||
|---|---|---|---|---|---|---|---|
| LPP | Falls | Phlebitis | Blood transfusion | Total | p-value | ||
| Follow up | With follow up | 57 (44.1%) | 20 (15.7%) | 20 (15.7%) | 3 (2.4%) | 100 (78.7%) | 0.102 |
| No follow-up | 16 (12.6%) | 5 (3.9%) | 6 (4.7%) | 0 (0%) | 27 (21.3%) | ||
| Severity | No damage | 56 (44.1%) | 15 (11.8%) | 18 (14.2%) | 2 (1.6%) | 91 (71.6%) | 0.002 |
| Reversible damage | 13 (10.2%) | 7 (5.5%) | 7 (5.5%) | 0 (0%) | 27 (21.3%) | ||
| Disability | 4 (3.1%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 6 (4.7%) | ||
| Death | 0 (0%) | 1 (0.8%) | 0 (0%) | 1 (0.8%) | 2 (1.6%) | ||
| Service | Hospitalization | 72 (56.7%) | 25 (19.7%) | 23 (18.1%) | 3 (2.4%) | 123 (96.9%) | 0.482 |
| Outpatient consultation | 1 (0.8%) | 0 (0%) | 2 (1.6%) | 0 (0%) | 3 (2.4%) | ||
In the initial analysis, we used descriptive statistics to determine the measures of central tendency (mean) and simple frequencies according to variable type. We determined data normality with the Kolmogorov-Smirnov test; in addition, we used the T-test with independent samples to demonstrate differences between the variables of the study and Spearman’s correlational test to establish a relationship between AEs and the other study variables. For all the tests, we considered a threshold of p<0.05 and a confidence interval of 95% as significant. Data analysis was performed with the IBM Statistical Package for the Social Sciences (SPSS) (Armork, US) v24.0 for Windows (Table 2).
3. ETHICAL ASPECTS
This study has followed the principles of the Helsinki Declaration, safeguarding the participants’ information [16]. In addition, this study has been approved by the Research Ethics Committee of the Universidad de Ciencias y Humanidades (Acta CIE Nº076-2019, May 29th, 2019).
4. RESULTS
The mean age of the 127 participants with AEs was 28±8 years (95%CI: 25.1 to 37.4). Of the total AE reports, 56% (72/130) affected males, and the most affected age group was from 24 to 35, with 43.4% (55/130); it was followed by the group from 12 to 23 years, with 17.3% (22/130); from 48 to 59 years, with 11.1% (14/130); from 36 to 47 years and > 60 years, both with 10.2% (13/130); and finally, from 0 to 11 years, with 7.9% (10/130). The main AEs were PUs, with 57,5% (73/127). They were reported as higher in males, with 44.1%, and in the age group from 24 to 35 years, with 25.2% (32/127). They were followed by phlebitis with 20.5% (26/127); falls with 19.7% (25/127); and transfusion with 2.5% (3/127).
Regarding AE severity, 71.7%º (91/127) did not have any harm; of them, 44.1% (56/127) corresponded to PUs; 11.8% (15/127) to falls; 14.2% (18/127) to phlebitis; and 1.57% (2/127) to blood transfusion. In addition, 21.3% (27/127) had permanent damage, 10.3% of them (13/127) were PUs, and 5.5% (7/127) were both falls and phlebitis. Furthermore, in 4.7% (6/127), we could observe disability, where 3.14% (4/127) corresponded to PUs and 1.57% (2/127) to falls. Finally, mortality was an adverse event in 1,6% (2/127) of the participants, where falls and blood transfusion were present in 0.78% (1/100) each. Finally, with regards to follow-up, 78.7% (100/127) had been followed up by the health personnel. Thus, 44.8% (57/127), 15.7% (20/127), 15.7% (20/127), and 2.36% (3/127) were followed up, having PUs, falls, phlebitis, and blood transfusion, respectively.
The mean age of the 127 participants with AEs was 28±8 years (95% CI 25.1 to 37.4). Of the total reports with AE, more than half affected males (56%) and the age group of 24 to 35 years (43.4%). The main AE was PUs with 57.5%, which was also higher in males (44.1%) and in the 24-35 age group (25.2%). It was followed by phlebitis (20.5%), falls (19.7%), and blood transfusion (2.5%). As regards the severity of AEs, almost three quarters were unharmed (71.7%), of which 44.1% corresponded to PUs, 11.8% to falls, 14.2% to phlebitis, and 1.57% to blood transfusion. Finally, regarding follow-up, almost 80% of the AEs had been followed up by the health personnel. The highest percentage corresponded to PPU (44.8%), followed by falls, phlebitis, and blood transfusion.
Significant differences were found between age groups (p=0.001) and among AEs of varying severity (p=0.002). Also, our results showed a significant association between AE severity and age group (p<0.05); thus, both cases (1.6%) of deaths and half of the cases of disability affected patients older than 48 years old.
5. DISCUSSION
This study determined the AEs derived from nursing care, and we found the most frequent AE to be PU, followed by phlebitis and falls, which mainly affected the age group between 24 and 35 years old, but increased the severity according to the patients’ age. In addition, a hundred reports were followed up by the health personnel; and with respect to EA severity, more than half did not have any harm, and PUs were the most frequent.
One of the strengths of this study is that we used an instrument standardized by MINSA to quantify AEs. Also, we included the determination of AE follow-up as an objective of this study, which is not done in previous studies [3, 4, 10, 11]. Moreover, an assessment explains that retrospective research methods facilitate data collection and are effective in estimating AE incidence [17].
Our findings showed PUs as the most common AE. This is consistent with studies conducted in Spain and Colombia, where PUs are the most frequent, with 42.3% and 52.5%, respectively [7, 8].. PUs are skin lesions usually over a bony prominence as a result of pressure [18]. They involve concerning morbidity and mortality in patients, which increases the risk of death by five-fold [19]. PUs cause physical and emotional suffering, not only for the patient but also for families, since they cause pain, deformity, body odor, intimacy loss, and low self-esteem. In addition, their treatment is expensive and accounts for 4% and 5% of healthcare expenditure in Europe and Spain, respectively [20]. Regarding these AEs specifically, other studies in Peruvian tertiary hospitals have shown that they tend to mainly affect the elderly (74.19%) and that their most common location is at the level of the sacrum (77%) [21]. Other location in which, we can see PUs is on the heels (57.6%); in Spain, their prevalence is 30.1% at the time of admission and 73.9% after discharge. It is estimated that their incidence is 9,5 new cases per 100 hospitalization days, and we can mention that old age, residence, and reduced outdoor mobility are among the main risk factors for developing pressure ulcers on the foot [22]. Even so, in British hospitals, we can find lower PU prevalence rates, between 10.6% and 13.2% [23], similar to another Peruvian study, where 12,9% prevalence was found [24].
On the other hand, our results are different from a study conducted in Brazil, in which the most frequent AE was related to probes, drains, and catheters (which would correspond to phlebitis), with 61.6% occurrence, and PUs were only present in 4.92% of the cases [8]. Studies have shown a high prevalence of phlebitis, as 52% of patients had at least initial signs due to poor assessment of the vein and increased time to intubation [24]. There are other factors that influence not only its occurrence but also its severity. A study found that out of those who had only one catheter, 71.4% had phlebitis, and 10% of those who had two catheters, had severe phlebitis [25].
Furthermore, despite the low frequency of falls (19.7%), we can highlight that the frequency of falls has decreased over the years as evident in the findings of the studies on falls in hospitals. In a Spanish hospital, a total of 445 falls between 2009 and 2013 were reported, in which the average age of the patients was 62 to 83 years. The year with the highest number of falls was 2009 with 86, which decreased to 55 in 2013 [26]. This is fundamental because we also have to take into account the level of knowledge AE professionals have. A study on nurses in Peru showed 55% and 45% to achieve optimal levels and questionable levels in AE prevention, respectively. Furthermore, 74% had a practical level of fall risk prevention, 77% had a questionable level of PU prevention, and 57% had an optimal level of medication management [11]. In this study, 78.8% of AEs were followed up. It is important to highlight that it is concerning when the patient makes the transition from hospital to home upon discharge, since regardless of the place of origin (urban or rural), up to 28% may experience AEs afterwards, and it is estimated that more than two-thirds are preventable [27]. Furthermore, a higher incidence of AEs has been found in patients who had their first follow-up visit within a week after transfer [28]. Thus, the importance of follow-up is clear since it allows us to understand the frequency, patterns, and trends of the different types of AE in order to identify, train and promote learning in health professionals and nursing interns so that they can provide quality care according to the patients’ needs [29, 30].
This study involves limitations. Firstly, only reports from a tertiary hospital were taken into account; hence the frequency of AEs may vary in other health facilities in rural, Andean, or Amazonian areas where differences can be seen [13]. Another limitation is that the most frequent anatomical locations of AEs were not specified [21], nor were the factors that influenced their aggravation or prolonged duration [25]. Despite these limitations, this study has determined the most frequent AEs, and their severity has been found to be associated with age groups.
CONCLUSION
Our results suggest the most frequent AEs derived from nursing care to be PUs, followed by phlebitis and falls. Most AEs were followed up and affected younger patients.
In addition, older age was associated with the severity of AE. Identifying and reporting AEs is significant because it will demonstrate to clinical teams the importance and impact of their errors on patient health, incentivizing healthcare entities to research and improve their risk reduction programs.
LIST OF ABBREVIATIONS
| AE | = Adverse Events |
| PUs | = Pressure Ulcers |
| IBEAS | = Iberoamerican Study of Adverse Events |
| ICU | = Intensive Care Unit |
| MINSA | = Ministry of Health |
| SPSS | = Statistical Package for the Social Sciences |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Universidad de Ciencias y Humanidades Research Ethics Committee on 29 May, 2019 (protocol code “Acta CIE Nº076-2019, May 29, 2019”).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Patient consent was waived due to data anonymization, which was performed by an external person before the datasets were delivered to the authors. Patient consent was also waived due to the retrospective observational nature of this study. The ethics committee exempted the need to seek a written informed consent.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Restrictions apply to the availability of these data, which were provided by the Hospital Nacional Dos de Mayo. This information is stored in the SIGHOS (Sistema de Gestión Hospitalaria).
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors acknowledge the team of COVID-19 nurses of the Hospital Dos de Mayo for their tireless work and the data collection that made this study possible.


