All published articles of this journal are available on ScienceDirect.
Effect of Ice Bag Application to Femoral Region on Pain and Vital signs in Patients with Acute Myocardial Infarction Undergoing Percutaneous Coronary Intervention: A Randomized Controlled Trial
Abstract
Background:
Patients with myocardial infarction (MI) undergoing percutaneous coronary intervention (PCI) experience a great deal of pain and discomfort in the femoral region induced by femoral catheter removal, which can stimulate the sympathetic system and affect some vital signs.
Objective:
The aim of this study was to determine the effect of ice bag application to femoral region on pain and vital signs in patients with acute MI undergoing PCI.
Methods:
This is a double-blind randomized controlled trial study. The sample of this study consisted of 60 patients with acute MI undergoing PCI, including 30 patients per group, selected by convenience sampling method and assigned to intervention and control groups by block randomization method. The intervention included the use of an ice bag in the femoral catheter insertion site. Data collection tools included demographic information form, Numerical Rating Scale (NRS), and vital signs form. Femoral site pain and vital signs were measured in both groups before, during, and after femoral catheter removal. The data were entered into SPSS ver. 22. Using descriptive statistics, Chi-square and Mann Whitney test, data were analyzed.
Results:
Two groups were matched in terms of all demographic and disease-related variables (p>0.05). Pain score was lower in intervention group than in control group during and after the intervention (p<0.0001). Also, systolic, diastolic blood pressure, and temperature scores of the patients in the intervention group were significantly lower than the control group during and after catheter removal (p<0.05). Respiratory rate of the intervention group was significantly lower than the control group (p = 0.005). No significant difference between the two groups in the mean of heart rate in all three time periods (p>0.05).
Conclusion:
Application of the ice bag on the femoral region is effective in stabilizing the vital signs and decreasing the pain caused by femoral catheter removal in MI patients undergoing PCI. Therefore, considering its low cost and complications, topical application of an ice bag, as a nursing intervention to control the pain and keep stable vital signs, is recommended.
Clinical Trial Registration No: IRCT201511070249191N7.
1. INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of mortality globally. It is estimated that around 17.9 million people died from CVD in 2019, accounting for nearly 32% of all global deaths [1].
Statistics released by the Iranian Ministry of Health also show that this disease is responsible for almost 46% of all deaths in the country. Research indicates that the age of onset of first MI is decreasing in Iran, and complications increase dramatically with delayed onset of treatment [2].
Coronary invasive percutaneous procedures (PCI) as a standard treatment for patients with acute MI, is associated with lower rates of death, re-infarction, stroke, and intracerebral hemorrhage compared to thrombolytic therapy. The femoral arterial site has been the most commonly used during PCI. General and local complications occur following PCI. General complications are less common, including hypovolemia, cardiac arrest, and arterial embolism. Local complications are seen in 29%-65% of patients and include hematoma, vasovagal reaction, infection, ischemia, arterial obstruction, bleeding, and pain. Many patients experience pain during the removal of a catheter previously inserted into the femoral region [3, 4].
According to previous evidence, local complications such as vascular complications may develop when the pain induced by catheter removal is not controlled. Quality assurance efforts in pain management consist of methods to establish pain management protocols, to monitor their application, and to assess the benefits they provide to the patients. The quality of pain management that results from these efforts can be evaluated by assessment of various pain management outcomes, patients’ satisfaction is one of them. Healthcare facilities routinely use patient satisfaction evaluations to identify methods of practice improvement and better care provision [3-5].
Pain caused by the removal of a femoral catheter may be controlled by using pharmacological methods. Providing appropriate non-pharmacological nursing pain relief interventions to patients can greatly reduce the use of various medications and complications and may result in increased patient satisfaction from nursing care.
Non-pharmacological nursing interventions can also be helpful in relieving pain in patients. Cold therapy is one of the non-pharmacological methods to provide pain control [3]. Application of ice bag, as one of the cold therapies, increases the threshold of pain tolerance, decreases temperature, decreases blood flow, reduces pain and cell metabolism, and thus reduces tissue damage.
BayJndJr et al. (2017) conducted a randomized control trial study in title “The effect of the ice bag on the femur pain of patients undergoing invasive PCI on 104 patients (52 patients in each group).
The pain experienced by the patients was evaluated before and during removal and again while the nurse applied pressure on the catheter site after removal. The NRS scores were identified as NRS1, NRS2, and NRS3 for the three assessments, respectively. The results showed that pain scores decreased in the intervention group during and after femoral catheter removal [3]. Çürük et al. (2017) investigated the effect of ice bag application to the femoral region of patients undergoing PCI on topical vascular complications and low back pain. The results showed that the use of ice bag, as compared to the sand bag, was significantly effective in reducing pain, decreasing topical vascular complications and low back pain and making patients feel comfortable [6].
Miranda (2011) evaluated the pain intensity and vital signs after cardiac surgery. The study concluded that there was a relationship between the pain intensity and vital signs [7].
Considering the prevalence of pain in patients undergoing PCI, and the avoidance of pain-related complications that cause changes in vital signs, there is a need to reduce such pain in these patients and minimize changes in their vital signs. Because of these complications, care should be taken after PCI. Therefore, managing most post-PCI femoral arterial catheter complications is one of the main responsibilities of nurses in acute and critical care settings [4]. Also, nurses play an important role in helping patients to adopt non-pharmacological therapies such as applying cold. These methods are easier to perform and have fewer side effects and low cost.
1.1. Purpose
To determine the effect of the application of ice bag on the vital signs and pain in the femoral region of patients with acute MI undergoing PCI.
1.2. Literature Review
The authors reviewed studies published in 2017-2021 in relevant searching engines such as PubMed, ProQuest, Scopus, and Web of Science. Search terms included ice bag, vital signs, pain, Acute MI, PCI.
Kurt and Kaşıkçı (2019) conducted a quasi-experimental study on patients undergoing percutaneous coronary intervention. Patients were assigned to 3 groups of ice bag, placebo and control. In the experimental group, a cold pack was applied to the bottom of the sandbag for the first 15 min after withdrawing the femoral arterial catheter. Results showed pain was less in the experimental group at the catheter entry site compared to the control group [4].
BayJndJr et al. (2017) carried out a study on the effect of ice bag on femoral pain of patients undergoing PCI. In the experimental group, cold application was applied for 20 min by placing an ice bag on the site of the femoral catheter. Results showed that the pain was reduced in the intervention group during and after femoral catheter removal [3].
Çürük et al. (2017) performed a study on the effect of ice bag application to femoral region of patients undergoing PCI on local vascular complications and low back pain. Ice bag was applied for 20 min with 10 min intervals during 2 hours. They found that the highest pain scores were in individuals in sandbag applied group, and differences between groups were statistically significant. They concluded that icebag application is considered the most effective method compared to sandbag application with regards to decreasing pain and complication rates and providing patient comfort [6].
Sundar et al. (2017) performed a study aimed to determine the effect of ice massage cryotherapy on pain due to venous, arterial fistula puncture in hemodialysis patients. Cold application was made with ice cubes wrapped in gloves on the web between the thumb and index finger of the hand not having the arteriovenous fistula ten min before venipuncture and continued throughout the puncturing procedure. The results of this study showed that ice massage reduced pain when inserting cannula into an arteriovenous fistula in hemodialysis patients [8].
Miranda (2011) conducted a descriptive explorative study to evaluate the pain intensity and vital signs after cardiac surgery among 38 patients during the postoperative period. The findings of the data, measured before and after performing the nursing procedure, indicated that the manifestation of pain occurred at different levels and the main changes in vital signs were referred to blood pressure. The study concluded that there was a relationship between pain intensity and vital signs [7].
2. MATERIALS AND METHODS
2.1. Design
This is a double-blind controlled trial study registered in Iran's clinical trial database with the code (IRCT20151107024919N7). Patients and statisticians were not aware of the study groups.
2.2. Participants
The study population consisted of all acute MI patients undergoing PCI. Sample size was determined using the results of Bayındır et al.’s study (2017). Thus, considering the pain SD score of 1.4 in the intervention group and 2.1 in the control group, α= 0.05, and study power= 90%, the researcher sought to discover at least 1.5 pain score differences between the intervention and control groups [9]. According to the foregoing study, the sample size was 60 individuals (n= 30 per group) using the sample size formula. Patients were assigned to intervention and control groups using randomized block design (4 blocks) where two persons were assigned to the intervention group and two to the control group in each block. The advantages of block randomization are that it ensures the balanced number of participants in each group over time and the difference in the number of individuals in each group will never exceed half the number of individuals in each block.
The samples were selected by convenience sampling method. Convenience sampling is defined as a method adopted by researchers where they collect market research data from a conveniently available pool of respondents. It is the most commonly used sampling technique and randomly divided into control and intervention groups after obtaining their informed consent. Inclusion criteria included individuals aged above 18 years, Iranian nationality, alertness, stable hemodynamic status. Exclusion criteria also included the use of sedative and analgesic medications, cold sensitivity, history of Raynaud's disease, mental illnesses (self-reported), history of previous angiography, sensory and physical problems, such as visual and hearing impairment, experience of arrhythmia or vasovagal response during femoral catheter removal, need for analgesics or narcotics during intervention, and narcotics and alcohol addiction. It should be noted that two patients in control group had vasovagal reaction and were excluded from this study.
3. INSTRUMENTS
Data were collected by demographic information form, clinical information form, vital signs form (blood pressure, pulse, respiration, temperature), and NRS, as pain-assessment instrument.
3.1. Demographic Information Form
It included information on age, gender, education, BMI, occupation, pain tolerance, history of a chronic illness, history of medication use, history of smoking, and history of angiography in the family.
3.2. Clinical Information Form
It included PCI related information such as catheter size, femur pain, heart pain, and duration of catheter placement in the femoral site.
3.3. Vital Signs Form
Vital signs (blood pressure, pulse, respiration, temperature) of the two groups were recorded by the first author in this form before, during and after the intervention.
3.4. Numerical Rating Scale (NRS), Pain Assessment Instrument
This scale consists of a 10-centimeter graded ruler, with numbers ranging from zero (no pain) to 10 (the most severe possible pain). The pain severity was indicated by the number circled or shown by the patient. On this scale, the possible pain score range was 0-10, with scores 0, 1–3, 4–6, and 7–10 representing no pain, low, moderate, and severe pain, respectively. NRS has been widely used in pain-related research, and its validity and reliability have been confirmed. For construct validity, the NRS was shown to be highly correlated to the VAS (r=0.95) and it has been showing high test–retest reliability (r= 0.96) [10]. 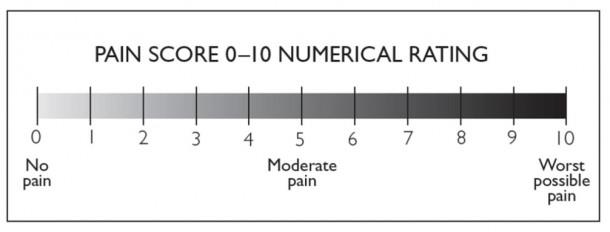
4. INTERVENTION AND DATA COLLECTION
In this study, each acute MI-diagnosed patient was referred to the cardiac emergency room and confirmed to be a candidate for PCI, and the patient was then dispatched to the angiography department as soon as possible. After transferring the patient from the angiography department, the researcher came to her/his bedside, evaluated the inclusion criteria, and explained the study objectives and method if they were eligible for inclusion. After obtaining informed consent, demographic and clinical information forms were completed through face-to-face interviews with the patient and observation of his / her medical record. Patients were assigned to intervention and control groups using a randomized block design. Pain and vital signs were measured by the first author in both groups before femoral catheter removal.
In the intervention group, in addition to routine care, underwent the ice bag treatment (10 × 15 cm, 250 g, Beauty Basics Model NT_ 304, Berlianteb Company) in the femoral region for 20 minutes before femoral catheter removal. Pain and vital signs were then measured and recorded by the first author during femoral catheter removal. After femoral catheter removal, the femoral region was assessed by the angiography nurse and pain and the patients’ vital signs were recorded by the first author immediately at 60 seconds. The routine protocol of application of manual compression to the catheter site was performed by the angiography nurse after femoral catheter removal and then a sandbag (2kg) was placed in the femoral region for 4-6 hours in both groups. It should be noted that the 6-inch Cordis catheter was used for patients.
Vital signs, pulse, respiration, and blood pressure were recorded and measured using a monitor attached to the patient, and the temperature was also measured using a Tympanic digital thermometer (Beurer, Iran). The probe cover was placed on the head of the thermometer, the thermometer was placed in the patient's ear and the body temperature was measured. The probe cover of this thermometer was replaceable, which prevented ear infections. The memory of this thermometer stored up to 9 temperature readings, allowing the researcher to observe changes in body temperature at any time. In order to prevent and reduce the error, vital signs were measured before femoral catheter removal at two twice at 5-minute intervals and twice after femoral catheter removal with 15-minute interval and the mean value of each time step was then recorded.
4.1. Data Analysis
The data were entered into SPSS ver. 22. Descriptive analysis was conducted using central indices, dispersion, frequency, percentage, and mean). Chi-square test was used to determine the similarity of the two groups in terms of the studied variables. Mann-Whitney test was used to compare the pain score and vital signs between the two groups considering the non-normality of the data distribution. P-value < 0.05 was considered as the significance level.
4.2. Ethical Considerations
In this study, after receiving the Code of Ethics (IR.KMU.REC.1397.325) from the Ethics Committee of Kerman University of Medical Sciences and the clinical trial code from the Iranian Registry of Clinical Trials (IRCT20151107024919N7), an introduction letter was submitted to the hospital where data were collected from the School of Nursing and Midwifery. The confidentiality of information and voluntary participation in the study was explained. In addition, the patients were informed about the study’s purpose, methodology and probability of placing in the control or the intervention group before data collection, and their questions were answered before written consent was obtained. The intervention was performed by a skilled nurse. After extracting the results, the findings of the study were also made available to the research authorities.
5. RESULTS
5.1. Descriptive Findings
The mean age of the patients in the control and intervention groups was 56.7 ± 12.4 and 58.5 ± 9.8 years, respectively. All patients (100%) had acute MI. Chi-square test showed that both groups were homogenous in terms of all demographic and disease-related variables (p>0.05) (Table 1).
| Variable | Control M(SD) |
Intervention M(SD) |
Statistics p-value |
|
| Age | 56.7(12.4) | 58.5(9.8) | t=0.61 P=0.53 |
|
| BMI | 24.14(3.97) | 25.25(2.96) | Z=-0.86 P=0.38 |
|
| Time of catheter placement | 6.9(1.88) | 8(1.11) | Z=-0.39 P=0.69 |
|
| Variable |
Control N) %) |
Intervention N) %) |
Statistics p-value |
|
| Gender | Male | 23(76.6) | 24(80) | Chi2=0.09 P=0.75 |
| Female | 7(23.3) | 6(20) | ||
| Education level | Uneducated | 6(20) | 6(20) | Chi2=0.95 P=0.91 |
| Elementary | 8(26.7) | 9(30) | ||
| High school | 5(16.7) | 6(20) | ||
| Diploma | 9(30) | 6(20) | ||
| Bachelor | 2(6.7) | 3(10) | ||
| Job | Employed | 1 (5.3) | 3 (15.8) | Chi2=0.45 P=0.92 |
| Housewife | 1 (5.3) | 0(0) | ||
| Self employed | 4 (21.1) | 3 (15.8) | ||
| Others | 2 (10.5) | 8 (42.1) | ||
| Pain tolerance | Low | 7(23.3) | 6(20) | Chi2=1.13 P=0.56 |
| Moderate | 10(33.3) | 14(46.7) | ||
| High | 13(43.3) | 10(33.3) | ||
| Drug history | Yes | 10(33.3) | 9(30) | Chi2=0.07 P=0.78 |
| No | 20(66.7) | 21(70) | ||
| Cigarette smoking | Yes | 6(20) | 4(13.3) | Chi2=0.48 P=0.48 |
| No | 24(80) | 26(86.7) | ||
| PCI history in family | Yes | 3(10) | 5(16.7) | Chi2=0.57 P=0.44 |
| No | 27(90) | 25(83.3) | ||
| Chronic disease history | Yes | 10(33.3) | 9(30) | Chi2=0.07 P=0.78 |
| No | 20(66.7) | 21(70) | ||
| Femoral ecchymosis | Yes | 7(23.3) | 4(13.3) | Chi2=1.00 P=0.31 |
| No | 23(76.7) | 26(86.7) | ||
5.2. Pain
Findings showed that mean score of pain before femoral catheter removal in control and intervention groups was 1.4 ± 0.27 and 0± 0, respectively, which was not significantly significant (p=0.15). While mean score of pain during femoral catheter removal was 2.73 ± 77.5 in the control group and 1.1 ± 1.39 in the intervention group, which was statistically significant (p<0.0001). Also, mean score of pain after femoral catheter removal was 1.72± 0.83 and 0±0 in control and intervention groups, respectively, which was statistically significant (P<0.0001) (Table 2).
6. VITAL SIGNS
6.1. Blood Pressure
Findings showed that the mean systolic blood pressure before femoral catheter removal in the control and intervention groups was 122.75± 14.53 and 123.19± 11.03, respectively, which was not statistically significant (p = 0.89), while mean systolic blood pressure during femoral catheter removal was 135.50± 14.78 and 171.97± 17 in above groups, respectively, which was statistically significant (p<0.0001). Findings also showed that mean systolic blood pressure after femoral catheter removal in the control and intervention groups was 128.13± 21.31 and 114± 24.80, respectively, which was statistically significant (p = 0.012).
Findings also revealed that the mean diastolic blood pressure before femoral catheter removal in the control and intervention groups was 76.28± 8.28 and 74.33± 13.16, and there was no significant difference between the two groups in terms of diastolic blood pressure before femoral catheter removal (p = 0.21), while mean diastolic blood pressure during femoral catheter removal was 83.30± 10.63 and 70.80 ± 11.42 in the above groups, respectively, and there was a significant difference between the two groups in terms of diastolic blood pressure during femoral catheter removal (p<0.0001). The findings also showed that the mean diastolic blood pressure after femoral catheter removal was 77.71± 9.36 in the control group and 71.53± 9.65 in the intervention group, which was statistically significant (p = 0.012) (Table 2).
| Variable | Time | Group | Mean ± SD | Statistic | p |
| Pain | Before catheter removal | Control | 1.43±0.27 | Z=-1.42 | 0.15 |
| Intervention | 0 ± 0 | ||||
| During catheter removal | Control | 5.77±2.73 | Z=-5.66 | <0.0001 | |
| Intervention | 1.10±1.39 | ||||
| After catheter removal | Control | 1.72±0.83 | Z=-2.78 | 0.005 | |
| Intervention | 0 ± 0 | ||||
| Systolic BP | Before catheter removal | Control | 122.75±14.53 | Z=-0.13 | 0.89 |
| Intervention | 123.11±19.03 | ||||
| During catheter removal | Control | 135.5±14.78 | Z=-3.77 | <0.0001 | |
| Intervention | 17 ± 117.97 | ||||
| After catheter removal | Control | 128.21±13.31 | Z=-2.51 | 0.012 | |
| Intervention | 114±24.80 | ||||
| Diastolic BP | Before catheter removal | Control | 8.28 ± 76.28 | Z=-1.23 | 0.21 |
| Intervention | 74.33±13.16 | ||||
| During catheter removal | Control | 10.63 ± 83.30 | Z=-3.88 | <0.0001 | |
| Intervention | 11.42± 70.80 | ||||
| After catheter removal | Control | 9.36± 77.71 | Z=-2.50 | 0.012 | |
| Intervention | 9.65± 71.53 |
| Variable | Time | Group | Mean ± SD | Statistic | p |
| Pulse rate | Before catheter removal | Control | 74.35±16.27 | Z=-1.014 | 0.31 |
| Intervention | 78±10.20 | ||||
| During catheter removal | Control | 81.43±15.33 | Z=-1.95 | 0.051 | |
| Intervention | 75.23±7.05 | ||||
| After catheter removal | Control | 75.50±14.55 | Z=-0.25 | 0.80 | |
| Intervention | 75.10±7.96 | ||||
| Respiratory rate | Before catheter removal | Control | 17.13±0.34 | Z=-0.074 | 0.94 |
| Intervention | 17.18±0.46 | ||||
| During catheter removal | Control | 18.83±2.33 | Z=-2.81 | 0.005 | |
| Intervention | 17.47±1.19 | ||||
| After catheter removal | Control | 17.20±0.44 | Z=-0.95 | 0.34 | |
| Intervention | 17.18±0.62 | ||||
| Temperature | Before catheter removal | Control | 37.29±0.86 | Z=-1.47 | 0.13 |
| Intervention | 37.42±0.64 | ||||
| During catheter removal | Control | 37.33±0.72 | Z=-3.98 | <0.0001 | |
| Intervention | 36.72±0.60 | ||||
| After catheter removal | Control | 37.27±0.70 | Z=-3.57 | <0.0001 | |
| Intervention | 36.78±0.51 |
6.2. Pulse Rate
Results showed that the mean pulse rate before femoral catheter removal in the control and intervention groups was 74.35± 16.27 and 78.20± 10, respectively and the two groups were not significantly different from each other with regard to the pulse rate before the femoral catheter removal (P=0.31). The mean pulse rate during femoral catheter removal in control and the intervention groups was 81.43± 15.33 and 75.23±7.05, respectively, which was not statistically significant (p = 0.051). Results of the present study demonstrated that the mean pulse rate after femoral catheter removal in the control and intervention groups was 75. 14± 50.55 and 75.10 ± 7.96, respectively, which was not statistically significant (p = 0.80), so there was no significant difference between the two groups in the mean pulse rate in all three stages (Table 3).
6.3. Respiratory Rate
Findings showed that the mean respiratory rate before femoral catheter removal in the control and intervention groups was 17.13± 0.34 and 18.17± 0.46, respectively which was not statistically significant (p = 0.94). The mean respiratory rate during femoral catheter removal in control and intervention groups was also 18.83 ± 2.33 and 17.47 ±1.19, respectively, which was statistically significant, as the respiratory rate was lower in the intervention group (normal range) than the control group (p=0.005). The results showed that the mean respiratory rate after femoral catheter removal in the control and intervention groups was 20.17 ±0.44 and 18.17± 0.62, which was not statistically significant (p=0.34) (Table 3).
6.4. Temperature
Findings showed that the mean pre-intervention temperature in the control and intervention groups was 37.29± 0.86 and 37.42± 0.3, respectively, which was not statistically significant (p = 0.13). Also the mean temperature score during femoral catheter removal in the control and intervention groups was 33.37± 0.72 and 36.72±0.60, respectively, which was statistically significant (p<0.0001). Findings showed that the mean temperature after femoral catheter removal in control and intervention groups was 37.27± 0.70 and 78.36 ± 0.51, respectively, and there was a significant difference between the two groups in terms of mean temperature after femoral catheter removal (p<0.0001) (Table 3).
7. DISCUSSION
Invasive interventions are more widely used as acute MI treatment today, but these methods may cause problems and complications that require nursing interventions. The results of the present study showed that 20-min application of icebag in the femoral area is effective in reducing pain and to keep stabilizing some vital signs (blood pressure, respiration, and temperature) in patients with acute MI undergoing PCI.
The findings showed the pain score was lower in the intervention group compared to the control group during and after femoral catheter removal. Therefore, the intervention group experienced less pain than the control group. This finding is consistent with the results of studies by Kurt and Kaşıkçı (2019), BayJndJr et al. (2017), Çürük et al. (2017), Sundar et al. (2017) and Attia et al. (2017).
Kurt and Kaşıkçı, (2019) showed pain was less in the patients undergoing percutaneous coronary intervention at the catheter entry site compared to the control group [4].
BayJndJr et al. (2017) showed that after cold application, the pain was reduced in the patients undergoing PCI during and after femoral catheter removal [3]. Çürük et al. (2017) concluded that ice bag application is considered the most effective method compared to sandbag application with regards to decreasing pain and complication rates and providing patient comfort [6].
Sundar et al. (2017) showed that ice massage reduced pain when inserting a cannula into an arteriovenous fistula in hemodialysis patients [8]. The reason for this consistency can be attributed to the use of cryotherapy for at least 20 min in most of the above studies since cryotherapy should be applied for at least 5 minutes to produce its optimal physiological effects. At the meantime, drug methods are expensive. On the other hand, due to side effects such as drowsiness, and gastrointestinal bleeding, non-drug therapy is often preferred.
Based on the findings, the use of icebag decreased the blood pressure of the intervention group during and after femoral catheter removal compared to the control group. However, there was no significant difference between the two groups in terms of the mean heart rate in all three stages, meaning that the ice bag application to the femoral did not affect the heart rate in patients with acute MI undergoing PCI. According to Attia et al. (2017) ice bag application to cardiovascular changes reduces blood pressure, but the exact cause is unknown. They go on to say that hemodynamic parameters are influenced by other physical and mental factors [9]. It should be noted that the findings of the study on the effect of ice bag on respiratory and pulse rates showed that ice bag affected the respiratory rate only at the time of femoral catheter removal, and the intervention had no effect on the pulse rate at the above three stages. Findings of Attia et al.’s study (2017) showed that cryotherapy is effective in improving respiratory rate before and after arterial puncture [9]. Hodges et al. (2018) conducted a study on cardiac autonomic function during hypothermia and its repeated measurements and concluded that hypothermia would lead to an increase in heart rate [11]. The three above studies reported similar and contradictory results that could possibly reject or confirm the effect of cryotherapy on these responses, which seems to be due to the use of different cold therapies (ice bag vs. cryotherapy and hypothermia). Therefore, it is better to conduct studies on the factors affecting changes in blood pressure, respiratory rate, and pulse rate with the use of the ice bag in order to comment more confidently on the results.
The results of the current study showed that ice bag application to the femoral region of patients with acute MI undergoing PCI can decrease temperature during and after femoral catheter removal and even MI-induced fever. There has been no study investigating the effect of ice bag on the temperature of patients undergoing PCI. However, this finding is consistent with the results of the study by Kazan and Gorgulu (2017) in patients after arthroscopic knee surgery [12]. Efforts to lower body temperature due to feverish illnesses have been carried out using cold water compresses or by using cold foot baths for many years; nowadays using different cooling techniques (ice, crushed ice and water mixed with ice, and cryotherapy) are used to lower the body temperature. Kazan and Gorgulu (2017) stated that when the ice bag is used, the intra-tissue temperature, which is high, approaches the ice bag temperature and as a result, the temperature decreases and the ice bag starts melting until it reaches equilibrium temperatures which decreases skin temperature in response to cryotherapy being a major determinant and known factor for cold therapy application [12]. It should be noted that alcohol has been sometimes used in combination with ice or ice and water mixture to reduce body temperature in some studies, which has been more effective than using ice pack alone. Since these studies are aimed at finding the best method to reduce patients' problems, further studies should be carried out to improve the comfort and convenience of patients using non-invasive, low-cost methods. One of the strengths of the present research is that the intervention is effective, inexpensive, and safe.
LIMITATIONS
This study has several limitations. One limitation of this research was that patients in the control group, such as the patients in the intervention group, did not spend the same time with nurse, and this difference may be effective in expectancies and stabilizing their vital signs. Another limitation included subjective reporting of pain that may be lower or more than the actual rate.
Also, the weight of the ice bag is a confounding variable in the study. The weight of the bag on a low BMI vs obese BMI could impact the patient femoral region differently, especially with regard to temperature.
Third limitation of this study is that it was conducted on patients with PCI in the cardiac emergency room of Training and Research Hospital affiliated with Health Sciences University. For this reason, the results of this study can only be generalized to similar settings.
RECOMMENDATIONS FOR FUTURE RESEARCH
It is recommended to conduct future randomized controlled trial that compare the efficacy of ice pack application on the vital signs and femoral site pain in patients with acute MI undergoing PCI, by using different nonpharmacological methods.
Also, this study should be conducted in non-acute situations limiting the compulsion of the patients.
NURSING IMPLICATIONS
Management of pain is a high priority for nursing care and the study results support the effectiveness of simple, non-pharmacological and effective interventions like icepack application in the reduction of pain and stability of vital signs in patients undergoing percutaneous coronary intervention. This intervention makes PCI less complicated and distressing for the patients and heightens the need for effective pain management among nurses working in the angiography unit.
Knowledge of non-pharmacological interventions which are cost-effective and easily available is essential for clinical nurses to alleviate pain and promote comfort for patients. Nursing education should offer short term continuing nursing education program on integration of pharmacological and non-pharmacological interventions in reducing pain and decreasing the need for narcotic analgesics. Clinical nurses should be encouraged and motivated to apply the research findings in their daily nursing care and to bring out new innovative interventions to prevent suffering and promote comfort for the patients.
CONCLUSION
This study employed a safe intervention without any negative effects on the vital signs and femoral region pain in patients with acute MI undergoing percutaneous coronary intervention. According to the results of the present study and previous studies, the use of icebag reduces the pain caused by femoral catheter removal and stabilizes respiration rate, blood pressure, and temperature in acute MI patients undergoing PCI. The advantages of ice bag application, on the other hand, include easy acceptance and good cooperation on the part of most patients, absence of undesirable side effects of medication interventions, and most importantly, nurses' independence while carrying out the intervention, so, it can be used as an effective therapeutic technique to reduce pain and stabilize respiration, blood pressure, and temperature of patients undergoing angiographic interventions.
LIST OF ABBREVIATIONS
| CVD | = Cardiovascular Disease |
| NRS | = Numerical Rating Scale |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
In this study, the code of ethics (IR.KMU.REC.1397.325) received from the ethics committee of Kerman University of Medical Sciences, Iran.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
CONSORT guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and analyzed during the current study are available from the corresponding author [B.T] upon reasonable request. Confidentiality and security of data and materials were ensured through all stages of the study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The present article is the result of a master's thesis, which is registered in the Department for Research and Technology of Kerman University of Medical Sciences with the code 97000319. The researchers would like to sincerely thank the patients who participated in this study.


