All published articles of this journal are available on ScienceDirect.
Feedback on the Preceptor's Experience Post-training: “A Quasi-experimental Design”
Abstract
Background:
The conventional clinical practice component of undergraduate nursing education is insufficient preparation for contemporary professional nursing practice. The preceptorship program became a substitute for limited clinical training in nursing school. Few studies have been conducted to demonstrate its practice impact above that of conventional clinical training. Therefore, the preparation of nurse preceptors is vital to any of the preceptorship roles. The preceptor plays a significant role during the transition period from being a student to a competent nurse. He/she provides direct supervision, support, and guidance, and offers a role model to consolidate scientific knowledge, practice clinical skills, and develop professional attitudes and values.
Objective:
The objective of the study is to assess differences between the preceptors' knowledge pre- and post-training program, evaluate preceptor’s feedback regarding the training program, assess the effect of the training program on preceptor’s performance three months post-training, and evaluate student’s satisfaction with the preceptor’s performance three months post-training.
Method:
A quasi-experimental design was adopted in this study. Overall, there were 79 (n=34 Saudi and non-Saudi nurse demonstrators and lecturers who have working experience of at least six months and n=45 nurse students) study participants. Questionnaires were used to collect data.
Results:
A statistically significant difference was found between pre-test and post-test values of nurse demonstrators and lecturers' awareness of preceptorship.
Conclusion:
Participants perceived the preceptorship program positively as they learned to assume different roles as a preceptor, an educator, a facilitator, a role model, and an evaluator.
The preceptorship program focuses on essential skills pertinent to clinical and educational settings. It develops clinical preceptors' roles and helps them support, develop and integrate new graduate nurses' clinical competence using an individualized and systematic approach. The ultimate aim is to ensure patient safety, i.e., the preceptee masters the clinical skills needed for competence before moving into more advanced nursing care tasks.
1. INTRODUCTION
A preceptorship involves two individuals in a professional relationship; an experienced nurse assists an inexperienced nurse colleague or student to acquire professional knowledge, attitudes, and skills. As nursing is a practice-based profession, nursing students need to increase their competency and confidence in decision-making, clinical skills, and knowledge application within clinical settings. Preceptorship is typically time-bound and often develops into a mutually satisfying mentoring relationship between the preceptor and the student [1, 2]. Thus, the demand for effective preceptors arises from healthcare organizations that strive to prepare and grow talent within their professional workforce [3, 4].
It was believed that the conventional clinical practice component of undergraduate nursing education is insufficient preparation for contemporary professional nursing practice. Hence, the preceptorship program in the workplace became a substitute for limited clinical training in nursing school [5, 6]. Unfortunately, few studies have demonstrated its practice impact above that of conventional clinical training. The preceptor training program is developed in response to a need to prepare preceptors in the workplace. The overall purpose of this preceptorship training program under study is to develop an understanding of the comprehensive roles of a nurse preceptor. This program is also designed to motivate inexperienced demonstrators and lecturers to assume preceptor roles and emphasize the importance of these roles for those involved in the preceptorship process.
2. BACKGROUND
Preceptorship is one of the strategies that help advance new graduate’s clinical skills from a student to a qualified professional nurse. Previous studies have heavily emphasized the positive impact of preceptorship training programs in reducing the gap between theory and practice that nurses experience in clinical settings [7-12].
Lalonde and McGillis Hall [13] indicated that the core of the preceptorship training program is to designate an experienced nurse or nurse clinician (a preceptor) to effectively work with and guide a new nurse (a preceptee) in a particular clinical setting. The preceptor plays a significant role during the transformation period from being a student to a competent nurse. He/she provides direct supervision, support, and guidance, and offers a role model to consolidate scientific knowledge, practice clinical skills, and develop professional attitude and values. This role development enhances communication with patients, their families and other healthcare team members [11, 14-16]. Practice experiences create a respectful and mutual relationship between a preceptor and the newly appointed nurse that facilitates learning and ensures the achievement of clinical competence [1, 10, 17, 18].
Preceptorship has many benefits. These benefits are not limited to facilitating a student's transition to a qualified nurse or helping newly qualified nurses gain confidence with specific clinical skills. The ultimate benefit is to provide new nurses with a real-life experience of practice while upholding the student-learner relationship [10, 19].
Nursing faculties have integrated preceptorship within clinical education for the past 30 years. Hence, it has become a dominant approach to supporting international learning and practice in clinical settings. The preceptorship approach is characterized by the instructor's responsibilities and practice assessment processes shared between the preceptor and nursing faculty member. The preceptor typically is an experienced nurse who is enthusiastic about teaching. A preceptor's responsibilities involve developing and improving new nurses or students' clinical skills by assuming role modelling, communicating professionally with others while performing nursing duties, and guiding the nurse preceptee [10, 14, 15, 20].
Communication between the preceptor and the preceptee and the preceptor and faculty is essential in preceptorship. This communication enables the student to understand how the expert nurse manages problems and provides patient care. Nursing faculty must continuously assess this partnership status with the preceptor. The progress of the preceptee, the overall learning experience and any concerns must be discussed together [7, 21].
While giving professional encouragement and assistance, a preceptor must assume one of four role functions, i.e., role modelling, facilitation, guidance, and prioritization. Nursing literature classified preceptor's functions into various tasks and roles. For example, the preceptor's one significant function is demonstrating appropriate nursing practice for students and newly appointed nurses. Supervision, assessment, and counselling are other functions included in the preceptor’s role because these strengthen the professional relationship [14, 22-24].
The nursing faculty member often liaises with the preceptor, preceptee, and the clinical setting. The faculty member is committed to orienting the preceptor about the clinical practice required, practice learning objectives, and the expected outcomes, in addition to specific information related to the clinical skills required to evaluate the preceptee's performance. Some researchers suggest that the most significant characteristics of a preceptor are personal characteristics, clinical competency, instructional skills, and encouragement [10, 25].
The exclusion of nursing faculty and health care managers from the selection process of preceptors can lead to the selection of inexperienced practitioners, resulting in an inadequate standard of preceptorship [26, 27]. Selecting a clinically competent preceptor is essential because the preceptor will work to improve the clinical competence of preceptee [10, 26]. Some preceptors may doubt their abilities to teach future nurses properly because they feel unprepared for the role, leading to difficult role experiences and increasing preceptor and preceptee’s stress [28, 30]. A preceptorship program offers the preceptees opportunities to develop and refine their daily practice and simultaneously decreases the “reality shock,” a common experience during initial clinical exposure [22, 29-31].
The relationship established between preceptors and students positively affects both parties. The preceptor and preceptee will further develop the skills required for working in the field [32-34]. However, the literature suggests that when preceptorship is in use, there is often a lack of detail regarding the ideal ratio between staff nurses and students. Furthermore, few standardized guidelines for the curriculum are included in the preceptorship model [30-32, 35]. Studies have identified a relationship between effective preceptors, reduced nurse turnover and increased patient safety. While nurse managers are key to nurse recruitment, staff nurses as preceptors are the key to nurse retention. Accordingly, the requirement for registered nurses to serve as preceptors for new nursing staff is increasing [18, 26, 36, 37].
2.1. Purpose and Significance of the Study
Establishing preceptorship programs to guide students and prepare new nurses for today's clinical practice is efficient and cost-effective when done well [26, 32]. As a result, a program for preceptorship is developed in response to the need to have prepared preceptors in the workplace. Thus, the preceptorship program aims to improve participants' awareness of the role of nurse preceptors, motivate faculty to sustain preceptor roles, and emphasize the significance of enhancing the confidence and self-reliance of graduate nurses. In addition, the goal is to prepare preceptors in the workplace and increase job satisfaction for the preceptee and the preceptor.
3. THE MAIN OBJECTIVES
The main objectives of this paper are to assess differences between the preceptors' knowledge pre- and post-training program, evaluate feedback from the preceptors regarding the training program, assess the effect of the training program on preceptor’s performance three months post-training, and evaluate the students’ satisfaction with the preceptors’ performance three months post-training.
4. METHODS
4.2. Sample and Recruitment
A convenience sample was used. The study sample comprised 79 (n=34 nurse demonstrators and lecturers and n=45 nurse students) participants.
4.2.1. Inclusion Criteria
The inclusion criterion was nurse demonstrators and lecturers with more than six months of work experience affiliated with Imam Abdulrahman bin Faisal University (IAU) and willing to percept student nurses in their clinical years, and no prior experience of preceptor role preparation.
4.3. Setting
This study was conducted at King Fahd Hospital of the University, and College of Nursing, Imam Abdulrahman bin Faisal University IAU, Saudi Arabia.
4.4. Tool
The researchers developed four questionnaires after reviewing related literature.
4.4.1. Tool I
Measures the nurse demonstrators’ and lecturers' awareness of preceptorship before and after the training program. It contains five open-ended questions about the preceptorship, the preceptors' roles, and their qualities.
4.4.2. Tool II
Comprises a structured questionnaire that assesses nurse demonstrators' and lecturers' feedback regarding the preceptor training program. It included 12 statements about the relevance to students' needs and interests, the trainer's effectiveness in presenting material, the quality of hand-outs, and the use of audio-visuals. A five-point Likert scale was used to record the responses, ranging from poor to excellent.
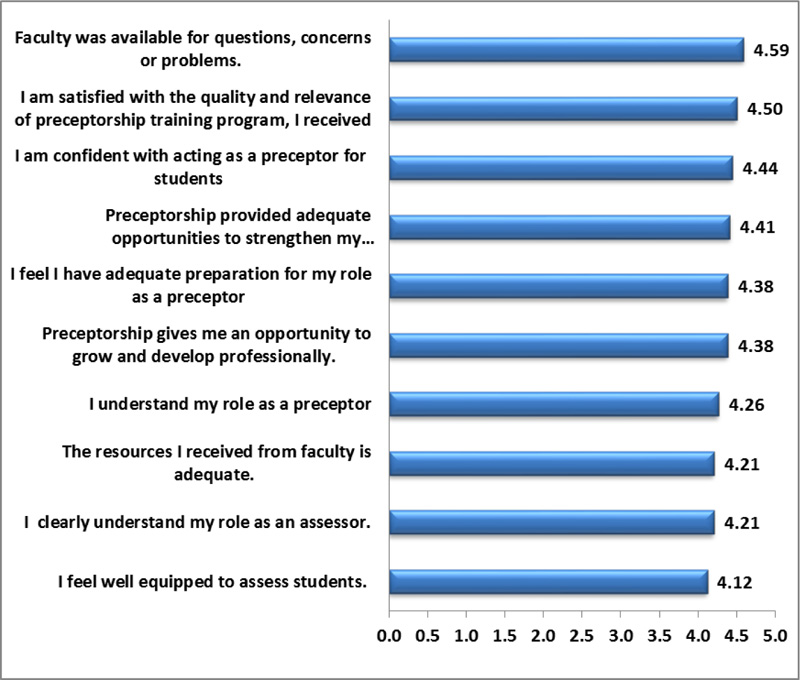
4.4.3. Tool III
Is a questionnaire that assesses the effectiveness of the training program in terms of the preceptors' performance from their perspectives. It consisted of 10 statements about how preceptorship training strengthened participants' communication skills to understand their role as preceptors and prepared them. This questionnaire also uses a five-point Likert scale to indicate the degree of the participants' agreement, ranging from strongly agree (5) to strongly disagree (1).
4.4.4. Tool IV
Is a structured questionnaire that assesses the satisfaction of nursing students regarding the performance of the preceptors who attended the preceptorship training program. It includes eleven statements related to the preceptors' ability to enhance the clinical skills and knowledge of student nurses and their availability to answer their questions and concerns. The questionnaire uses a five-point Likert scale, which indicates satisfaction from 5= very satisfied to 1= not at all satisfied.
4.5. Validity and Reliability
Three experts in different nursing specialties assessed the tools for ″content and face validity″. Test-retest reliability of Likert scale ordinal data used Kendall's tau and Spearman's rho, and most of the values obtained were greater than 0.76, indicating high reliability. Likewise, questionnaires were assessed for internal consistency reliability using Cronbach's coefficient alpha, yielding values of 0.9, indicating excellent internal reliability. The researchers conducted a pilot study with 10% of nurse demonstrators and lecturers to evaluate the statements' usability and suitability and the time required to complete the questionnaire. Rewording and rephrasing were conducted accordingly.
4.6. Ethical Approval
Ethical approval was obtained from the Institutional Review Board (IRB) at Imam Abdulrahman Bin Faisal University (IAU).
4.7. Data Collection Procedures
The program structure comprised five modules: preceptor roles, the role model, the educator, the facilitator, and the evaluator, and it was delivered over four weeks. The training included group activities, application exercises, and group discussions.
Researchers assessed the nurse demonstrators’ and lecturers’ awareness of preceptorship before and after their completion of the training program, using Tool I (pre and post-test). Later, feedback was sought regarding their experience of the training program using tool II. Finally, a post-test was conducted two weeks following the completion of the program. In addition, a three-month follow-up of the program's effectiveness was conducted to discover the satisfaction of preceptors’ and students’ satisfaction about their preceptors' performance, using tools III and IV.
The questionnaires were distributed to the participants by the research team, which required 10 to 15 minutes to complete, and study data were collected over a total period of five months.
4.8. Statistical Analyses
Data were coded, classified, and subjected to statistical analysis. SPSS (Statistical Package for Social Sciences) (version 17.0) was used to analyze data, and graphical presentation was achieved through the use of “Microsoft Office Excel.” Categorical data were described using numbers and percentages, while the mean and standard deviation were used for continuous data. The pre-test and post-test values were compared using the paired sample's t-test, and the test result was considered significant at P< 0.05.
5. RESULTS
Table 1 shows the distribution of participants' demographic characteristics. 56% of the participants were demonstrators, and 44% were lecturers. More than one-third (38.2%) of them were in the age group 25-27. A high percentage of demonstrators/lecturers (41.2%) were from medical-surgical, with the percentage from Oby-Gyn and critical care specialties similar at 17.6%. The majority (67.6%) of the demonstrator/lecturer sample had less than five years of experience. Regarding students, 48.9% were in the age group 20-21 and 44.4% were in their second year. 44% of the students were enrolled in the medical-surgical course.
The results in Table 2 show the post-test mean score (17.09 ± 2.11) to be higher than the pre-test mean score (8.53±3.15). There is a significant difference between participants' pre-test and post-test values, as the p-value is less than 0.05 (t 14.74). This result suggests that there is a substantial change in the participants' awareness related to preceptorship.
|
Demonstrators and Lecturers’ Characteristics (n= 34) |
Students’ Characteristics (n= 45) |
||||
|---|---|---|---|---|---|
| Age | No. | % | Age | No. | % |
| 22-24 | 9 | 26.5 | 19-20 | 20 | 44.4 |
| 25-27 | 13 | 38.2 | 20-21 | 22 | 48.9 |
| 28-30 | 7 | 20.6 | ˃ 21 | 3 | 6.7 |
| ˃ 30 | 5 | 14.7 | Academic Year | No. | % |
| Category | No. | % | |||
| Demonstrators | 19 | 56 | 2nd | 20 | 44.4 |
| Lecturers | 15 | 44 | 3rd | 15 | 33.3 |
| Specialty | No. | % | 4th | 10 | 22.2 |
| Oby-Gyn | 6 | 17.6 | Course | No. | % |
| Pediatric | 5 | 14.7 | Oby-Gyn | 8 | 17.8 |
| Medical-surgical | 14 | 41.2 | Pediatric | 6 | 13.3 |
| Critical care | 6 | 17.6 | Medical-surgical | 20 | 44.4 |
| Psychiatry | 3 | 8.8 | Critical care | 4 | 8.9 |
| Years of experience | No. | % | Psychiatry | 7 | 15.6 |
| < 5 | 23 | 67.6 | |||
| ≤ 5 | 11 | 32.4 | |||
| N | Mean | Std. Deviation | Paired Differences | t | df | Probability | |||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Std. Error Mean | |||||||
| Pretest | 34 | 8.53 | 3.15 | 8.56 | 3.39 | 0.58 | 14.74 | 33 | .00000 |
| Post-test | 34 | 17.09 | 2.11 | ||||||
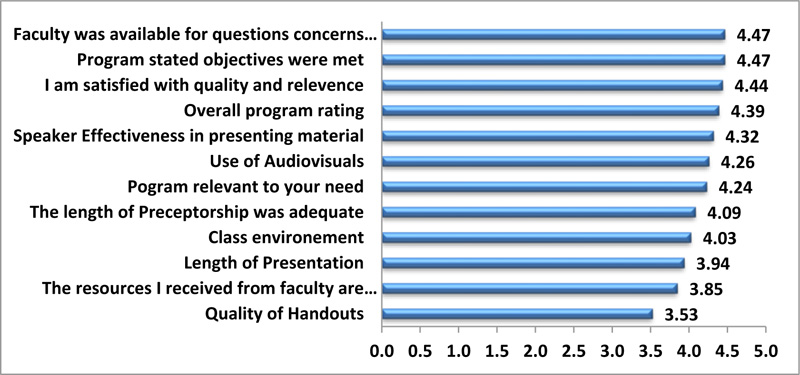
Fig. (1) illustrates positive feedback from the participants about the preceptorship training program, as the highest mean score was an equal value (4.47) for both items: ″faculty was available for questions, and ″ program's stated objectives were met”.
Fig. (2) shows the program's effect on preceptors' performance at post-program follow-up. It illustrates the highest average mean score (4.59) for the item “the faculty member was available for questions, concerns, or problems.” While the item that portrayed participants' “…satisfaction with the quality and relevance of the preceptorship training program they received”, the mean score was 4.5. The average mean score (4.44) was reached for the item “being confident with acting as preceptors for students” as well as (4.41) mean score for “preceptorship allows them to strengthen their communication skills.”
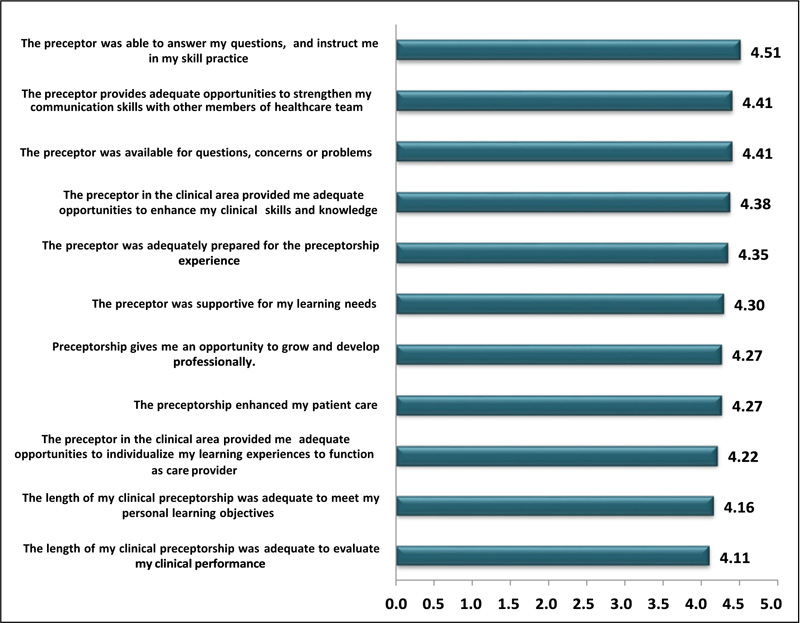
The researchers assessed students' satisfaction with the preceptors' performance (Fig. 3). They were delighted with the following items: a high average mean score (4.51) as rated by students for the item: ″The preceptor was able to answer their questions and instruct them in their skill practice.” Also, high mean score (4.41) rating was given for both items: “The preceptor provides them with adequate opportunities to strengthen their communication skills with other members of the health team” and “the availability of preceptors to show concerns for questions or solve problems.”
6. DISCUSSION
The organization's understanding of the effectiveness of preceptorship is crucial. Unfortunately, this study’s findings illustrated that participants lacked knowledge about preceptorship before engaging in the program. Most preceptors are skilled clinicians but have never been in a formal training role. As a result, they need to understand the learning process, be evaluators, and effectively provide student feedback. Hence, preceptorship training programs have been a valuable strategy for improving the quality of guidance to new graduates/nurse students (preceptee). These findings support claims in previous studies that ″the preparation of preceptors in the teaching and assessing fields is vital to feel prepared to fulfil their roles as preceptors” [38-41].
This study’s findings highlighted that the program was rated highly by participants regarding the “availability of faculty member for questions, concerns or problems,” ″satisfaction with the quality and relevance of preceptorship training program, ″, and ″program's objectives were met ″. The findings of this study also endorse those in earlier published studies that suggest that the success or failure of preceptorship depends on the preceptor's behavior, such as closeness, role modelling, and constructive feedback, thus enhancing student learning [31, 32, 39]. Hence, the preceptorship training program should be continuously evaluated to inform future adjustments and improvements [36].
This study also found that participants held a positive perception about the effectiveness of the preceptor training program regarding their role performance. They were satisfied after attending this program; they felt well-equipped to assess new nurses or students and acquired more understanding of their roles as assessors. In contrast, a lack of role satisfaction may influence preceptor retention and students' clinical learning quality [42]. Several studies have suggested that recently qualified nurses must participate in preceptorship after qualification. For example, Robinson and Griffiths (2009), Rogers (2021) and Kennedy (2019) stated that a significant component of a successful transition experience from a new nurse graduate to a qualified nurse is the constructive preceptorship relationship [43-45]. Moreover, numerous studies indicate that a practical approach to fostering nurse graduates' professional development and transition into clinical practice is their preceptorship experience [18, 32, 46, 47].
The current study's findings also demonstrate the program's impact on preceptors' performance through follow-up; they reported that the preceptorship training program they received gave them confidence in acting as preceptors for students and strengthened their communication skills. Our study results echo those from Marks-Maran et al.’s (2013) study that investigated the impact, value, and sustainability of a preceptorship program for newly qualified nurses from the perspective of the preceptees. Preceptorship was highly valued by the majority (85%) of preceptees in this study. In terms of stress reduction, preceptors were beneficial. In addition, preceptorship benefited preceptees in terms of communication and clinical skills development and role, personal, and professional development [48].
When exploring students' satisfaction with the preceptors' performance, our study findings showed that students were satisfied with the training provided by preceptors. Students reported that the preceptors were available to answer their questions, instructed them in their skill practice, and provided adequate opportunities to strengthen their communication. Other published studies about preceptorship training have suggested that the effectiveness of preceptorship training programs can distinguish between new nurses who have attended and those who have not attended the program. For example, Rachael Vernon (2017) and Al-Hussami et al. (2011) claimed that new nurses who attended the preceptorship program acquired more knowledge and skills, became good communicators, were more satisfied with their work, became more confident, and achieved higher patient satisfaction levels [10, 49].
Moreover, preceptorship fostered effective communication between the new nurses and their preceptors. Preceptors provide ongoing guidance and support for new nurses and prepare them to handle practice challenges. As new nurses observe and adopt the role behaviours of their preceptor, their professional judgment and clinical competency can be developed [49, 50]. Furthermore, preceptorship helps new graduates recognize the organization's culture and modify their attitude to become a part of the “working team” [13, 19, 51]. Harrison-White Simons (2013) reported that preceptees can provide high-quality and effective care and become more confident in their professional role through the assistance of competent preceptors [52].
CONCLUSION
The participants' knowledge levels dramatically enhanced the preceptor's roles, communication skills, responsibility, and confidence. In addition, preceptor participants have had a positive experience of the preceptorship training program, as they have learned to be a preceptor, an educator, a facilitator, a role model, and an evaluator. Hence, this preceptorship training program is a meaningful approach that fosters new nurses' professional role transition experience.
IMPLICATIONS
The preceptorship program focuses on essential skills, which are pertinent to clinical and educational settings. It develops clinical preceptors' knowledge, attitudes and skills, and helps them integrate, support, and develop freshly graduated nurses' clinical competence in an individualized systematic approach. The aim is to ensure patient safety, i.e., the preceptee masters the clinical skills needed for competence before moving on to more advanced nursing care tasks.
RECOMMENDATIONS
1. The preceptor challenge should be implemented as a training course intended to prepare the academic nurse demonstrator/lecturer to assume the function of an effective preceptor.
2. The preceptorship training program should be evaluated frequently and on an ongoing basis to encourage program adjustment and improvements.
3. Additional research should be conducted to closely identify the effect of grading/evaluation on the relationship between preceptors and preceptees.
4. Further research should be conducted to assess the impact of preceptorship on nursing practice and patient safety.
ETHICAL STATEMENT
The approval number of the ethics committee of the Institutional Review Board (IRB) at Imam Abdulrahman bin Faisal University (IAU) for this study was IRB-2014-05-064.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
STROBE guidelines have been followed.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author upon request.
FUNDING
This research was funded by Imam Abdulrahman bin Faisal University, Dammam, Saudi Arabia.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This research would not have been possible without the participants’ exceptional commitment and enthusiasm, which have kept our work on track to the end of the study. Furthermore, the authors thank Imam Abdulrahman bin Faisal University for funding and supporting this research. Finally, they also are grateful for the insightful comments offered by Dr. Isabel White and her generosity and expertise in proofreading the manuscript, which has improved this study in an innumerable way and saved it from many language errors. Those that inevitably remain are entirely the authors’ responsibility.


