All published articles of this journal are available on ScienceDirect.
Hand Hygiene in the Intensive Care Unit: Knowledge, Compliance and Factors Influencing Nursing Adherence, a Descriptive Study
Abstract
Background:
Nosocomial infections are particularly common among hospitalized patients who undergo resuscitation compared with other types of care. Hand hygiene remains the simplest and most effective measure to prevent and control the risk of infection.
Objective:
The main objectives are to evaluate hand hygiene compliance among nursing staff in the different intensive care units and to identify the factors influencing the adherence of nursing staff to the practice.
Methods:
It was a quantitative descriptive study using a questionnaire and an observation grid with all the nursing staff working in all the intensive care units of our university hospital.
Results:
The study showed a hand contamination rate of (80%), a hand hygiene compliance rate of (21.3%), it also showed the different factors explaining non-adherence, these are not necessarily related to training, nor to the availability of material resources but related to hidden reasons, non-apparent factors, which are often more important. (Workload and work environment)
Conclusion:
This study examined hand hygiene in the ICU setting, obtained data on overall compliance, which remains poor, and the various factors influencing nurses' adherence to the practice.
1. INTRODUCTION
Making health care safer in a complex, pressurized, rapidly changing environment is one of the major issues in health care today. Several studies show that unsafe care causes harm to a large number of patients, which can lead to serious sequelae and complications. In low- and middle-income countries, due to a combination of unfavorable factors, the safety of care is even less assured [1].
The World Health Organization (WHO) has made quality and patient safety one of its priorities and is launching the 1st World Challenge for Patient Safety the motto of this program is “Clean care is safer care” highlighting hand hygiene as an essential element to reduce healthcare-associated infections [2, 3].
These infections are particularly frequent in patients hospitalized in the intensive care unit, as compared to other sectors of care, a major cause of death due to the severity of their condition and the many invasive devices necessary for their management [4]. In Africa, the prevalence rates of healthcare-associated infections vary between 14.8% and 19.1% [5-7]. The last survey conducted in our institution in December 2014 revealed a rate of 11.1%; the most affected services were: Intensive care unit (40%) and hematology-oncology (14.8%) [8].
Hand hygiene is one of the basic practices essential to the prevention of infections in hospitals, both in patients and caregivers. Indeed, it has been reported to be the most important measure for preventing nosocomial infections and the spread of antibiotic-resistant pathogens [9, 10].
It has been rated Level IA (highly recommended for use based on scientific, clinical or epidemiological evidence) by the Centers for Disease Control and Prevention (CDC) and the Healthcare Infection Control Practices Advisory Committee (HICPAC) to reduce HAIs [11]. It is the basis of the program launched by WHO in October 2005: the first global patient safety challenge, “Clean Care is Safe Care”, which aims to reduce HCAIs worldwide [12, 13].
Despite its importance, the efforts made by specialists and the multiple promotion and training initiatives, studies constantly highlight poor compliance with hand hygiene in all sectors of care, including those at high risk of infection, particularly in developing countries [14-21]. This may be the beginning of an explanation for the increase in the prevalence of HAIs in our context.
Hence the present study evaluates hand hygiene compliance among nursing staff in different intensive care units, and identifies the factors influencing the adherence of nursing staff to the practice, to understand their interpretation and their own reading grid to this problem in order to implement corrective actions. In particular, several studies show that a 30% improvement in compliance is associated with a 41% decrease in the prevalence of infections [22, 23].
2. MATERIALS AND METHODS
Study design: It is a quantitative descriptive study that uses a questionnaire and an observation grid which involve all the nursing staff working in the intensive care units of our university hospital.
Study setting: The study took place from January to May (2019-2020) at the level of all intensive care units of our university hospital (Table 1).
Study target population: The target population of the study corresponds to all the nursing staff practicing at the level of the intensive care units.
2.1. Data Collection Methods and Tools
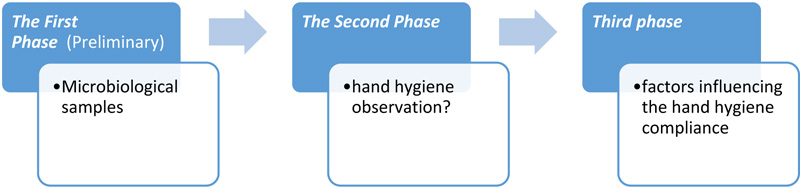
This study is divided into three parts:
2.1.1. The First Phase
The completion of 20 hand samples initiated the 1st phase from voluntary and anonymous caregivers (informed consent). The samples were taken as part of the celebration of World Hand Hygiene Day (2019) (Appendix 1). The objective was to show the extent of the handling in intensive care units and, of course, an educational objective, using the results to provide hand hygiene training during awareness days for health care workers.
Sampling was performed by nursing staff who specialized in the prevention of infectious risk. The technique consisted of rubbing the hand with a sterile swab moistened by brain heart infusion (BHI) broth. The swabs were then transmitted to the laboratory in their protective cases as quickly as possible, under conditions that did not alter the viability, or the number of microorganisms, and protected against contamination.
| Establishment | Specialty |
|---|---|
| Hospital 1 | Surgical resuscitation |
| Medical Resuscitation | |
| Resuscitation of surgical emergencies | |
| Burning Resuscitation | |
| Hospital 2 | Versatile Resuscitation Service |
| Hospital 3 | Pediatric Resuscitation Service |
| Maternity Resuscitation Service | |
| Neonatology Resuscitation Service |
2.1.2. The Second Phase
The 2nd phase of the study concerns the compliance audit (verifying that a hand hygiene gesture is performed when expected). The data were collected by direct observations reported in a standardized WHO observation grid. The professional categories targeted were doctors, nurses and physiotherapists, present on the audit days. The types of hand hygiene evaluated were disinfection by hydroalcoholic friction and simple washing at different times (morning - afternoon).
The individuals observed were randomly selected, not according to a pre-determined list. Two main hand hygiene opportunities were selected:
“Entrance” opportunity: as soon as healthcare personnel enter a room or prepare to take charge of a patient. This corresponds to the indication “before patient contact” and before an aseptic procedure.
‘'Discharge” opportunity: as soon as a health care professional leaves a room or ends the care of a patient. It corresponds to the fusion of two indications: “after last patient contact” and “after last contact with the patient's immediate environment”.
All heads of departments of the different intensive care units were informed that an observation would be carried out in the near future by the operational hygiene team (free and informed consent). But the nursing staff does not know the day the audit will be conducted, and the Hand Hygiene is observed to avoid a bias (Hawthorne effect).
Regular visits are made, especially to high-risk departments, in order to raise awareness among nursing staff, evaluate care practices and meet the expectations of nursing staff with regard to the prevention of infectious risks.
The results of these observations were presented as percent compliance representing the fraction of the number of times hand hygiene should have and the number of times it did occur correctly.
2.1.3. Third Phase
The last part of the study concerns the factors influencing nurses' adherence. The information was collected by means of a self-administered questionnaire with 4 main parts: identification, knowledge about hand hygiene, factors for non-adherence, and suggestions.
The questionnaire was developed from various tools prepared by WHO in the context of the Patient Safety and Hand Hygiene Program “Template for Self-Assessment of Hand Hygiene Promotion and Practice at the Health Care Facility Level” (Appendix 3).
It assessed healthcare workers' knowledge of hand hygiene, perceptions of healthcare-associated infections, and hand hygiene. Other questions were derived from international handwashing guidelines.
A Likert scale of 1 to 5 was chosen as a response choice; we tried to facilitate the statement of the questions, to inform about the purpose of the research and to give explanations of some items during the distribution of this questionnaire while insisting on the anonymity and confidentiality of all information provided.
In order to validate the questionnaire, a pre-test was carried out with ten (10) nurses working in intensive care units in order to measure the degree of comprehension and the ease of interpretation of this instrument. The internal consistency (Cronbach's alpha) of this tool was 0.780 in this study. After data collection using the selected methods, a descriptive statistical analysis of the data was performed using SPSS, which allowed for data tabulation and configuration.
3. RESULTS
3.1. Microbiological Samples
Of the twenty (n: 20) samples taken, 80% (n: 16) were positive. 20 bacteria were isolated: Coagulase-negative methicillin-resistant staphylococcus in the first position (54.2%), followed by ESBL-producing Enterobacteriaceae (12.5%) and C3G-susceptible Enterobacteriaceae (12.5%) and in last position Pseudomonas aeruginosa (4.2%).
Multi-bacterial contamination of the hands was found in 3 samples (presence of multiple bacteria).
3.2. Compliance Audit
The sessions collected 370 Opportunities before and 410 after contact with the patient or his or her environment, a total of 780. The distribution of observations by occupation is presented in Table 2:
| Résults | N | % |
|---|---|---|
| Number of Positive samples. | 16 | 16,7% |
| Number of Negative samples. | 4 | 83,3% |
| Number of germs found . | - | - |
| Methicillin-resistant coagulase-negative staphylococci (MRCoNS) | 13 | 54,2% |
| Enterobacteriaceae Producing Broad-Spectrum Beta Lactamases ((ESBL) | 3 | 12,5% |
| Pseudomonas aeruginosa | 1 | 4,2% |
| C3G-sensitive enterobacteria | 3 | 12,5% |
| Total | 20 | 100,0% |
| Bacterial associations | - | - |
| Methicillin-resistant coagulase-negative staphylococci (MRCoNS) + Enterobacteriaceae Producing Broad-Spectrum Beta-Lactamases (EBLSE) | 2 | - |
| Staphylococcus coagulase negative methicillin resistant + Enterobacteriaceae Producing Broad-Spectrum Beta-Lactamases (EBLSE) + P.aeruginosa | 1 | - |
3.2.1. Hand Hygiene Compliance Rate
A total of 780 Hand Hygiene opportunities were observed in the selected ICUs; the opportunities, translated into WHO hand hygiene indications, were distributed as follows: 370 “Before Patient Contact” opportunities and 410 “After Patient Contact” opportunities.
Overall compliance was 21.3% (166 out of 780 cases). However, in 78.72% of cases, no hand hygiene was carried out. Our results show a significant difference between the levels of hand hygiene compliance before and aftercare. The compliance after is better with 24.1%. However, the compliance before care was low at (18.1%) (Table 3).
| Hand Hygiene Indication | Number of Opportunities | Number of Observations | Compliance Rate |
|---|---|---|---|
| Before patient contact | 370 | 67 | 18.1% |
| After patient contact | 410 | 99 | 24.1% |
| Total | 780 | 166 | 21.3% |
4. HAND HYGIENE COMPLIANCE BY PROFESSIONAL CATEGORIES
3 categories were observed: nurses, doctors and physiotherapists. Of the total opportunities, nurses had the highest number of contacts (455 opportunities), 215 for doctors and 97 for physical therapists (Table 4).
Hand hygiene compliance varies with target groups. The highest rate was found in nurses (25.7%), kinesitherapists (15.5%), while the lowest rate was observed in doctors (14.9%). Hand hygiene compliance after contact with the patient is clearly more evident than before contact for the 3 categories observed, especially for kinetherapists 30% before, while 7.1% after contact.
| - | Nurse | Doctors | Physiotherapist | ||||
|---|---|---|---|---|---|---|---|
| Numbre | Compliance Rate | Numbre | Compliance Rate | Numbre | Compliance Rate | ||
| Before patient contact | Number of opportunities | 200 | 24,5% | 100 | 13,0% | 70 | 7,1% |
| Compliance | 49 | 13 | 5 | ||||
| After patient contact | Number of opportunities | 255 | 26,7% | 115 | 16,5% | 40 | 30,0% |
| Compliance | 68 | 19 | 12 | ||||
| TOTAL | 455 | 25,7% | 215 | 14,9% | 110 | 15,5% | |
5. QUESTIONNAIRE RESULTS
5.1. Study Participants
The demographic data from this study are presented in Table 5. In total, 124 questionnaires were distributed and retrieved. The respondents were predominantly 73% female, 87% were nurses and 13% were physiotherapists, and 75% had been working in their position for less than 5 years.
| Variable | n | % | |
|---|---|---|---|
| Gender | Male | 45 | 27% |
| Female | 79 | 73% | |
| Occupation | Nurse | 108 | 87% |
| Physiotherapist | 16 | 13% | |
| Experience | Less than 5 years | 93 | 75% |
| Between 5 and 10 years | 18 | 15% | |
| Up to 10 | 13 | 10% | |
5.2. Knowledge of Hand Hygiene
- Infection control / hospital hygiene training.
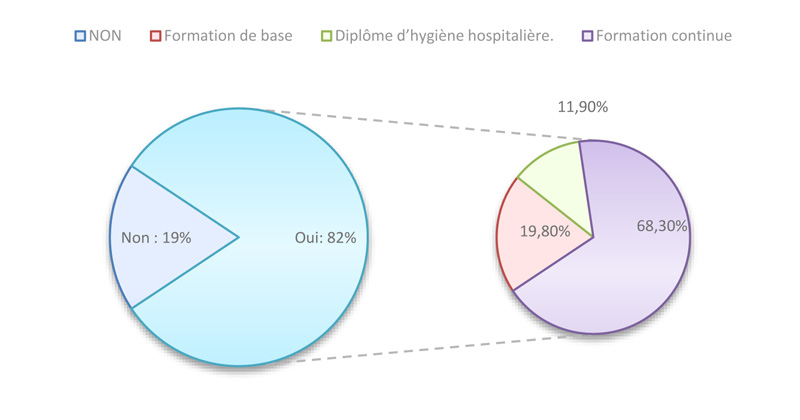
It was found that 81% reported having received hand hygiene training, 16% basic training, 39% continuing education and 27% diploma training in hospital hygiene and nosocomial infection prevention.
- Nurses' knowledge of Hand Hygiene:
The first category of predisposing factors concerned nurses' knowledge of infection prevention and control.
The results revealed that the majority of the nurses interviewed have a certain amount of knowledge, and beliefs on the subject; in fact, 97% are aware of the dramatic consequences of an infection associated with care for patients, 94.4% approved that the mastery of hand hygiene will decrease the incidence of HCAI at the level of intensive care units, while 92.8% knew the prerequisite of hand hygiene and its importance in relation to the effectiveness of the practice.
Nurses seem to have a good knowledge of hydro-alcoholic solutions: 67.7% know the effectiveness of SHA compared to simple hand washing, 67.8% proved the bacterial action of alcohol on infections even those related to BMR, 80% confirmed that simple hand washing is the suitable technique for soiled hands. On the other hand, only 27.4% confirmed that wearing gloves does not alter the indications of hand hygiene and does not replace the practice of hand hygiene (Table 6).
|
Strongly Disagree |
Disagree | Neither / Nor Agree | Agree |
Strongly Agree |
|
|---|---|---|---|---|---|
| A healthcare-associated infection (HAI) can have serious consequences for the patient. | 0 (0,0%) |
0 (0,0%) |
03 (2,4%) |
94 (75,8%) | 27 (21,8%) |
| Hand hygiene reduces the number of healthcare-associated infections. | 0 (0,0%) |
0 (0,0%) |
7 (5,6%) |
103 (83,1%) | 14 (11,3%) |
| For an effective hand hygiene: Your professional outfit is short-sleeved, short nails without varnish and no jewelry | 0 (0,0%) |
0 (0,0%) |
09 (7,3%) |
24 (19,4%) | 91 (73,4%) |
| Hydroalcoholic friction (FHA) is more effective than simple hand washing (water + soap) on microorganisms. | 0 (0,0%) |
15 (12,1%) |
25 (20,2%) |
50 (40,3%) | 34 (27,4%) |
| Hydro-alcoholic products offer a better tolerance on the hands than soaps. | 10 (8,1%) |
25 (20,2%) |
5 (4,0%) |
60 (48,4%) | 24 (19,4%) |
| Hydro-alcoholic friction should be preferred even in the presence of soiling on the hands. | 17 (13,7%) | 90 (72,6%) |
4 (3,2%) |
13 (10,5%) | 0 (0,0%) |
| A simple hand washing (water + soap) must systematically be carried out before any hydroalcoholic friction. | 09 (7,3%) |
63 (50,8%) |
02 (1,6%) |
50 (40,3%) | 0 (0,0%) |
| The active ingredients (alcohols) of these hydroalcoholic products have a bactericidal action, including on bacteria that are multi-resistant to antibiotics. | 0 (0,0%) |
27 (21,8%) |
13 (10,5%) |
76 (61,3%) | 08 (6,5%) |
| If I wear gloves, I still have to wash my hands after taking them off | 0 (0,0%) |
37 (29,8%) |
53 (42,7%) |
34 (27,4%) | 0 (0,0%) |
The nurses' knowledge was generally found to be quite solid, with many good answers, especially in relation to hydroalcoholic friction, which is considered the key to improving hand hygiene.
6. FACTORS AFFECTING HAND HYGIENE COMPLIANCE
Several organizational dimensions were affected by our study; these are factors and elements of the WHO multimodal strategy that may be involved in the adoption of healthy hand hygiene behavior:
The results show that participants in the ICU setting attributed the non-adherence of nurses to hand hygiene practice to several factors, but they emphasized workload and the number of patients to be cared for as the most important factor, with an overall response rate of 96.8%, the misuse of gloves instead of hand washing 71%, and the internal environment of the ward (59.7%).
However, 73% of staff did not link non-compliance to the availability of hand hygiene products, nor the knowledge component (73%). The results also show that 43% of nurses do not wash their hands because the products used for hand hygiene cause skin dryness and hand irritation (Table 7).
25% of the nurses strongly agreed that the organization of assessment sessions is one of the essential actions to improve compliance at the ward level, finally only 30.6% agreed that seniors not setting an example in hand hygiene is one of the reasons influencing the adherence of the nursing staff to hand hygiene.
7. DISCUSSION
This study highlighted several elements related to hand hygiene (Fig. 1). The first was to convince nurses to produce tangible evidence of contamination of hands during care by taking bacteriological samples from the hands of participants. The results showed a contamination rate of 80%. A similar Indian study in Gujarat reported a high rate of bacterial colonization of the hands 70% [24].
| - |
Strongly Disagree |
Disagree | Neither / Nor Agree | Agree |
Strongly Agree |
|---|---|---|---|---|---|
|
Hand hygiene products are not sufficient quantity or are inaccessible. |
18 (14,5%) |
68 (54,8%) |
13 (10,5%) |
16 (12,9%) |
9 (7,3%) |
| Misunderstanding of hand hygiene. | 39 (31,5%) |
48 (38,7%) |
23 (18,5%) |
14 (11,3%) |
0 (0,0%) |
| Reminders of hand hygiene in In workplace. | 0 (0,0%) |
22 (17,7%) |
15 (12,1%) |
87 (70,2%) |
0 (0,0%) |
| Lack of evaluation and reporting of results. | 0 (0,0%) |
73 (58,9%) |
5 (4,0%) |
46 (37,1%) |
0 (0,0%) |
| Influence of workload and number of patients to be taken care of. | 0 (0,0%) |
0 (0,0%) |
4 (3,2%) |
44 (35,5%) |
76 (61,3%) |
| Regular hand hygiene leads to dry skin and hand irritation | 34 (27,4%) |
49 (39,5%) |
7 (5,6%) |
23 (18,5%) |
11 (8,9%) |
| Health workers use gloves instead of hand washing. | 01 (8%) |
14 (11,3%) |
21 (16,9%) |
71 (57,3%) |
17 (13,7%) |
| Environment (internal context) not promoting hand hygiene. | 0 (0,0%) |
23 (18,5%) |
27 (21,8%) |
41 (33,1%) |
33 (26,6%) |
Coagulase-negative methicillin-resistant staphylococcus in the first position (54.2%), together with methicillin-resistant Staphylococcus aureus (MRSA), is an important cause of nosocomial infection, leading to increased morbidity, length of hospital stay and health care costs [25-27].
It has also been reported that MRSA and MRCONS strains share the same habitats and permanently or transiently colonize the anterior nares and other areas of the skin and mucous membranes, which can be sources of subsequent bacteremia and other infections [28] and even horizontal cross-propagation of resistance genes [29].
Resistant microorganisms isolated from the hands of caregivers are a potential risk factor for our resuscitation patients who have life-threatening failures and are at high risk for care-related infections.
This is why hand hygiene is one of the most important measures for the prevention of healthcare-associated infections. Healthcare workers must respect and enforce the 5 main hand hygiene guidelines recommended by the WHO [12].
The study also assessed hand hygiene compliance among nursing staff in intensive care and resuscitation units. Most observations were made among nurses because of their frequent contact with patients and also because they have more opportunities for hand hygiene than physicians [30].
The overall compliance with hand hygiene, all categories taken together, is 21.3%. The comparison of the results obtained with the data in the literature allows us to note a rate in the lower limits of those reported in the literature [31-36].
Compliance before care was 21.3%, and aftercare was 24.3% (as shown in Table 2). Similar results are found in the literature where all professional categories are less compliant before care as compared to aftercare [37].
Moreover, according to Erasmus et al. (2009), the attitudes of the nursing staff are to privilege their protection towards dirty and soiled substances. This leads to a form of compliance with a narcissistic purpose. The nursing staff does not consider the safety of the patient as a priority reason, but to answer a need for personal protectiononly for their quality of life [38].
The best adherence rate was noted among nurses (25.7%), and physiotherapists (15.5%), while the lowest was observed among physicians (14.9%). The result is in agreement with other studies, where doctors have a poor adherence compared to other health professionals [39, 40].
Several studies have also shown that the practice of hand hygiene among physicians is always worse; low adherence to good hygiene practices in their daily practice, and that compliance will remain alarmingly low [41]. Similarly, Van de Mortel et al. [42] found that hand hygiene knowledge and practices were significantly higher among nursing students than medical students.
This difference between doctors and nurses could be explained by the frequency and type of contact of nurses with patients [43, 44]. Another factor related to the intense interaction of nurses with patients is that they are required to perform technical care and apply aseptic measures and standard precautions at all times. In addition, each nurse has a bottle of hydroalcoholic solution in his or her workstation (care cart), which encourages adherence to the practice.
At the same time, the goal is not to create a competitive atmosphere for physicians and nurses. Rather, it is to help clinicians of all types understand where their handwashing compliance stands and how to improve it.
The third part of our study tries to explain the rate of compliance found (21.3%), looking for a nursing explanation of the different reasons for non-adherence to hand hygiene.
The majority focused on workload (96.77%); several studies highlighted nurse working conditions, as a motivating factor [45]; a busy and highly stressed environment has negative effects affecting hand hygiene practices [46-48]. In a study by McArdle et al. [47], understaffing and workload made hand hygiene less important, as it took more time and energy to attend multiple patients, hence their non-adherence behavior.
The 2nd reason is the use of gloves (70.97%). This is the main risk factor for hand hygiene non-compliance, and there is a correlation between inappropriate glove use and hand hygiene compliance [49, 50]. It was even found in a study by Cusini et al. [50], that hand hygiene compliance increased significantly after rationalizing the use of gloves.
The 3rd reason is related to regular reminders & incentives in the workplace (70.16%) with follow-up, distribution of posters and explanation of the importance of the practice to all health professionals. This is an essential element of the World Health Organization's (WHO) multimodal strategy for real improvement in hand hygiene compliance [51].
In relation to other reasons for non-adherence to hand hygiene, the lack of equipment is one of the main limitations of this technique [52, 53]. In our context, this is not a real factor since only 20.2% of the nurses mentioned it as a reason for not following hand hygiene practices.
Concerning the “Training” dimension, is a basic element of prevention and control of healthcare-associated infections [54-57]. The study showed that more than two-thirds (81%) of the people surveyed had received training in this area, (20%) basic training, (68%) continuing education and (16%) even a diploma in the prevention of infectious risks (Fig. 2).
Even for the nurses, level of knowledge was satisfactory, the proof is that they were able to answer the different questions related to hand hygiene. Moreover, only 11.29% agreed that it is an essential cause of non-compliance with hand hygiene.
Skin problems such as dryness and irritation caused due to the use of hand hygiene products, present a real problem in care units [58]. In our context, it was not cited much (27.42%), so it does not really present a real factor of adherence, moreover, several studies have shown that these products are better tolerated by the nursing staff and associated with a better skin condition than ordinary soap or antimicrobial [52-59].
Finally, the study showed a hand contamination rate of (80%), and a compliance rate of 21.3%; it also showed the different factors explaining non-adherence, which are not necessarily related to training nor the availability of material resources, but to hidden reasons, non-apparent factors, which are often more important. It is useless to have very nice protocols and procedures if there are inconsistencies and contradictions on the environmental and organizational levels, especially in a context where most of our intensive care units suffer from a shortage of nursing staff sometimes (5 nurses for 29 patients with heavy technical and relational care).
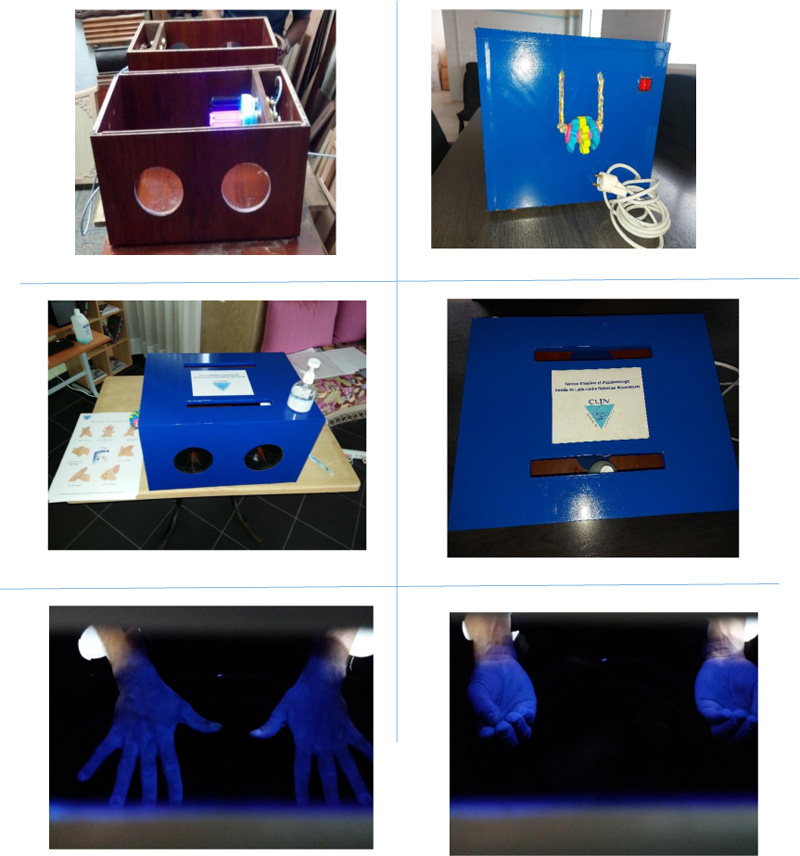
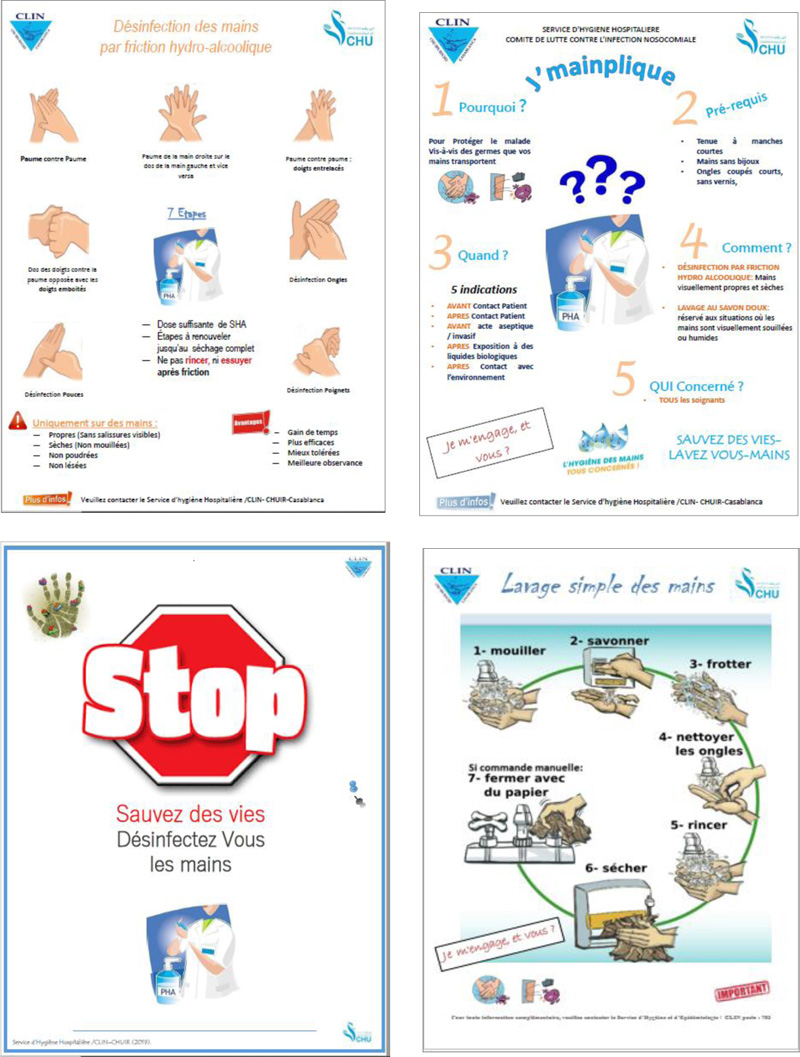
The promotion of standard precautions is at the center of our activity; we organize several theoretical and practical training sessions, especially for hand hygiene and the proper use of gloves. On May 5 of each year, we celebrate the global day of hand hygiene, a campaign of exchange, sharing of information, and motivation of the nursing staff (APPENDIX 1-3). The event is marked by practical workshops, a scientific program, bacteriological sampling of the hands of caregivers and interdepartmental competition (knowledge and availability of products) to raise awareness among the public and caregivers about infection prevention and identify actions for improvement.
And we were even able to produce our educational material to validate the application of standardized hand rubbing techniques with hydroalcoholic solutions (APPENDIX 2), as well as our own posters and reminders (APPENDIX 3).
Another element is that the study period coincided with the covid-19 pandemic, and all the activity of our service was devoted to crisis management; several training sessions on standard and complementary precautions were organized. Practical and illustrated communication materials were developed and distributed in all intensive care units to preserve the health and safety of health professionals and patients.
It is also important to note that during the period of COVID-19, the incidence of nosocomial infections in our institution has decreased [60, 61]. This decrease may be related to the positive aspects and benefits of the pandemic because all the resuscitation services were innovated, and equipped with the necessary human and material resources.
All the services were clean, safer, and healthier, and even the behavior of the nursing staff was changed; a respect for strict rules of hygiene, and individual protection was adopted for all the nursing staff, a new reflection on their way of caring and taking care of a patient was adopted.
8. LIMITATIONS
The main strength of this study is its comprehensive nature, which explored hand hygiene in intensive care units from all aspects (microbiological, knowledge, calculation of compliance rate and factors of poor compliance). It is in line with the international issues of the WHO through the World Alliance for Patient Safety for the prevention of NI through the promotion of hand hygiene practices.
This study also has some weaknesses and limitations; compared to hand sampling, the small number of samples taken, and the results obtained may not be generalizable to other caregivers and other care settings where the culture of infection prevention and control is different. It is also possible that the small surface area investigated (hand) and the sampling solution used to moisten the swab do not allow the exact microbiological contamination to be given (risk of false-negative).
Another point is that the samples were taken in the middle of the working morning in a random way without specifying whether the hands were disinfected or not. Our objective, like that of other studies [62, 63], was essentially to highlight the role of hands in the transmission of nosocomial infections, to determine the transient flora and to know the bacterial ecology of the isolated germs (circulating strains and their source).
In relation to the section on factors influencing hand hygiene adherence among healthcare workers, as in other studies [64-66], medical staff has been excluded since all of the doctors in our University Hospital are in training (internal doctors and residents). Another element is the lack of a concept of stability: Physicians in intensive care and resuscitation units change service every 6 months. In addition, there is a significant variation between the two categories in relation to the items sought: (Training, work organization, nature and workload.)
CONCLUSION
The present study has made it possible to examine hand hygiene in the intensive care setting, to obtain data on overall compliance, which remains insufficient, particularly among medical staff, as well as the various factors influencing nurses' adherence to the practice. The latter concern several dimensions, particularly the environmental dimension.
The implementation of a multimodal strategy recommended by the World Health Organization (WHO), including several areas of intervention, appears to be decisive for increasing the overall compliance rate.
The support of management and institutional bodies, the adoption of a collaborative approach with a wide range of training tools, and the monitoring of hand hygiene compliance are the main keys to success.
At the same time, healthcare professionals (doctors, nurses, and physiotherapists) must respect and improve their practice, attitude, and knowledge, which will play an important role in improving the quality and safety of care.
LIST OF ABBREVIATIONS
| WHO | = World Health Organization |
| BHI | = Brain Heart Infusion |
ETHICAL STATEMENT
This study has been approved by the Scientific Committee for the Control of Nosocomial Infections of our institution (a committee composed of professors of higher education and health executives).The committee elaborates and validates an action plan of the different activities related to the prevention of infectious risk, including the axes of training, prevention, monitoring and evaluation and with the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
The 1st phase was initiated by the completion of 20 hand samples from voluntary and anonymous caregivers (informed consent).
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILTY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.