RESEARCH ARTICLE
Exploring the Nursing Care Process for Patients with COVID-19: A Grounded Theory Study
Zohreh Karimi1
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187443462203290
Publisher ID: e187443462203290
DOI: 10.2174/18744346-v16-e2203290
Article History:
Received Date: 21/9/2021Revision Received Date: 9/1/2022
Acceptance Date: 21/1/2022
Electronic publication date: 31/05/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
A specific model and process of nursing care for patients with COVID-19 has yet to be developed. However, nurses are navigating how to care for patients and themselves in a novel and stressful work environment. A care process is needed that promotes effective nursing for patients’ health and well-being.
Objective:
This study aimed to explore the current nursing care process for patients with COVID-19.
Methods:
The present qualitative study used a grounded theory approach. Participants included 23 nurses working in a hospital COVID-19 ward who were selected through purposive sampling. Semi-structured interviews were conducted with nurses, and data were simultaneously analyzed using MAXQDA software to code the data. Grounded theory with a storyline approach was used to categorize codes to elucidate themes from interviews and check for data saturation. This consists of several steps, including open coding, developing concepts in terms of their properties and dimensions, analyzing data for context, bringing the process into the analysis, and integrating categories.
Results:
Data analysis revealed seven main categories to describe nurses’ conceptions of the care process for COVID-19 patients: ‘patients’ complicated condition’, ‘severe nursing staff shortage’, ‘nursing professionalism’, ‘treatment team collaboration’, ‘work and environmental pressure’, ‘efficacy of care’ and ‘care deficit’. The category of ‘nursing professionalism’ was determined to be the core concept that nurses used to describe their care process.
Conclusion:
Though nurses think highly of their efficacy of care for patients with COVID-19, they face many challenges in their care process that lessen the care they are able to provide for patients and themselves. These include the complex health status of patients, shortage of staff, environmental stresses such as becoming infected, and lack of resources in the hospital. The results of the present study can be used for planning in various fields of nursing, including management, education and clinical training.
1. INTRODUCTION
In March 2020, the World Health Organization declared a pandemic of the ongoing global health crisis of the coronavirus disease 2019 (COVID-19) [1]. So far, more than 277 million people globally have been infected with COVID-19, with estimates of more than 5 million people dead as a result of the virus [2]. In Iran, more than 6 million people have been infected, and more than 130,000 have died [2].
The novelty of the current coronavirus outbreak, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has put nurses in a unique position as the vanguard of care teams in medical centres as they navigate patient needs, symptoms and prognoses [3]. The care of patients is the essence of their partnership [4]; providing appropriate and ethical care can lead to more effective recovery of patients, reduction in their hospitalization time, and early discharge [5, 6]. Through the provision of proper care services, nursing, as a science and an art, can reduce patients’ pain and suffering significantly [7]. Nurses work on the front lines, meaning they need to constantly adapt to new technologies and guidelines while also considering patient needs [8]; this deep, complex relationship with care highlights the importance of the nurse’s role and the need to evaluate the services nurses provide to patients [9]. Nursing knowledge, experiential evidence and understanding patients’ values and beliefs contribute to improving fundamental nursing care [10]. The provision of care should be carried out in accordance with patients’ needs, as should the interaction between the nurse, the patient and others involved in the patient care [11]. Nurses must grapple with the complexity and sensitivity of human life, influenced by physical, psychological, economic and cultural factors that can greatly alter their working conditions and abilities, as well as the instability, variability and uncertainty that exist in providing care [12, 13].
Certain conditions necessitate the unique care that nursing provides, and care for patients with COVID-19 has required unique and special attention to many aspects of care that nurses typically don’t encounter on a day-to-day basis [13, 14]. The viral nature of the disease, the risk of transmission and severity of symptoms, the complexity of the condition, the need for continuous and complex care, and the very high resulting workload are among the serious problems that nurses confront when providing services to these patients [15, 16]. Additionally, nurses must consider their own well-being amid the unique challenges posed by COVID-19. Nurses around the world have struggled to obtain proper personal protective equipment (PPE) and have suffered from distress and mental health trauma related to the vulnerable conditions of patients [14].
Thus, despite being on the front lines, conducting many of the primary measures affecting patient care, nurses in COVID-19 wards face a completely unprecedented situation with little reprieve [17].
Care challenges continue to arise from active and careful examination of the condition of patients with COVID-19 and consideration of how to best provide care to patients in complete isolation [18, 19]. Although hospital nurses have made myriad adjustments to provide useful and effective care, existing care models are inadequate to address current needs [20, 21].
Because of the lack of a specific model and process for caring for COVID-19 patients, a transparent exploration of the care process for patients with COVID-19 can provide evidence for improving nursing care services and in turn, patients’ health and well-being. No studies have yet been conducted on the care process for patients with COVID-19; thus, a theoretical exploration of this process should be undertaken to increase professional knowledge and improve the health of patients with COVID-19 [22]. The issue of care is a social one, resulting from social interactions between various individuals involved in the context of care. Therefore, the grounded theory method, as a qualitative social science research method, can be used to explore the current process of care by using current evidence of practice to elucidate broader themes and practices [23]. Grounded theory emphasizes the interactions of individuals through a thorough and complete study of behaviours, actions, values, individuals and views of social groups [24, 25]. Theory should be constructed as an outcome of data interpretation, focusing on qualitative data such as interviews and oral history. Today’s nursing philosophy is the result of pluralism and the interaction of different values, ideas and paradigms that have been formed under the shadow of postmodernism [26].
2. MATERIALS AND METHODS
2.1. Study Design
This is a qualitative study using grounded theory to gain knowledge of the practice of nursing care for COVID-19 patients. The grounded theory method, best used when there is a lack of knowledge about the target phenomenon, is able to elucidate the patterns, meanings, and interactions between individuals involved in care, to paint a broad picture of the current care process. Corbin and Strauss (2014), the proponents of the grounded theory method, note that grounded theory explores the connections that describe the status of the target phenomenon [25]. In the present study, the fundamental assumption was in line with the theory of symbolic interactionism. Symbolic interactionism theory has been criticized because it ignores the emotional side of the self as a basis for social interaction.
2.2. Setting and Participants
Purposive sampling was used to find participants who could provide information-rich data about nursing practices. Participants consisted of 23 nurses who met the inclusion criteria: they were able to speak Persian, were over 22 years old, had at least four months of work experience in a COVID-19 ward, possessed no mental or physical disorders, and were willing to participate in the study. Sampling continued until data saturation was complete and a theory could be developed.
The ‘research field’ – the in-depth experiences of the performances, behaviours, beliefs and attitudes of individuals or groups as they are in real life [27] – was the real field of occurrence of phenomena in this study: the COVID-19 ward of a hospital.
2.3. Data Collection
After receiving a letter of introduction, the researcher was referred to the research field to obtain participants’ consent. The first participant was selected through a purposive sampling method. Individual, unstructured and semi-structured interviews with open-ended questions were conducted to allow the researcher and participants to the conversation as needed. Interviews were conducted in a suitable and secluded place, taking into account environment, time and participants’ tolerance and willingness to participate. Interviews were conducted face-to-face, by phone call, and by video call using programs such as WhatsApp and Skype, according to participants’ preference. The duration of each interview session was 45-90 minutes. At the beginning of each interview, the objective of the study was explained and patient consent was obtained. Participants could withdraw from the study at any time. All interviews were recorded and written down verbatim.
Two formal interviews were conducted with each participant. The first interview used open-ended and unstructured questions. After transcribing the first interviews, coding and theoretical sampling, with simultaneous analysis from the beginning of data collection, follow-up interview questions were developed according to participants’ responses in the first interviews. Follow-up interviews were semi-structured and were used to meet the objectives of the study by elucidating further explanations and examples. Examples of the questions asked in the interviews included: ‘Describe your experience caring for a patient with COVID-19.’ and ‘Explain your relationship with your patients.’ When necessary, each participant was interviewed again. At the end of the interviews, open-ended questions were asked, such as, ‘Is there anything you would like to add? I would be happy to hear it.’
For data collection from the study environment – including behaviours, performances, events and individual interactions – participant observation methods were used. Field notes were recorded of observations, hearings, events and the researcher’s own ideas. The presence of the researcher in the field involved no disturbance or participation. Memos were used in all stages from data collection to data analysis. In order to maintain reflectiveness in the research process, reflection notes were taken and the researcher also recorded personal experiences.
2.4. Data Analysis and Rigour
Data analysis was performed using the grounded theory approach proposed by Corbin and Strauss (2015). This approach consisted of several steps including open coding, developing concepts in terms of their properties and dimensions, analysing data for context, bringing the process into the analysis and integrating categories.
Data were analysed simultaneously with data collection, starting with the first interview. Each interview was transcribed within 24 hours of the interview. Transcripts of the interviews were read several times and coded using MAXQDA 10. Codes were developed using an iterative process. Core sentences were coded based on what participants said. Codes were then categorized based on similarity. As more codes developed, the codebook was reassessed and similar items were merged. By constantly comparing the codes, new categories were exported according to their common focus. A storyline approach was used to develop, orient and clarify the main categories to elucidate the main themes in the data. Based on the context in which a phenomenon occurred and its placement on the storyline, the connections between variables were continuously examined until a target process was identified. The created categories were constantly evaluated to ensure that each was unique. By focusing on the conditions and the context in which a phenomenon occurred and the conditions controlling the phenomenon, the core variables and the processes defining the data were identified.
The criteria developed by Guba and Lincoln were used to evaluate the data: credibility, confirmability, dependability and transferability. The credibility of data was confirmed by using triangulation of time, method [data] and source. Additionally, several techniques were used to establish credibility in the research methods: considering the participants as the most important source, gathering documents using the same data collection methods as the interviews, taking field and observational notes, bilateral and circular data collection and data analysis (i.e., starting the analysis simultaneously with the first interview), member checking, the researcher’s prolonged engagement with participants to understand their experiences and secure their trust, constant comparison of data, reading interviews several times for thorough understanding, and finally, the researcher’s experience in conducting qualitative research.
For confirmability and impartiality, the researcher performed bracketing methods by obtaining an agreement on codes and topics by reviewing interviews and codes multiple times, continuously providing reports, peer-checking and using multiple observers during the study.
For dependability, transcripts of the interviews were typed immediately after the interview. The entire dataset was re-examined with an external reviewer as debriefing, and an external report check was carried out. Finally, for transferability, interviews were performed with maximum variance of sampling and different terms and topics were used.
2.5. Ethical Considerations
In order to enter the research field, necessary permissions were obtained from hospital officials. Informed consent was obtained from all participants. At the beginning of each interview, the objective of the study was explained in full to each participant. All participants were assured that interview recordings and documents would be kept strictly confidential. This study was approved under the ethical code number IR.YUMS.REC.1399.113 by Yasuj University of Medical Sciences.
3. RESULTS
The participants included 23 nurses who were working in a COVID-19 ward. Nurses’ mean age was 28.434±3.369 years, with a range of 23 to 35 years old. The nurses’ mean work experience was 7.782±2.696 years, with a range from 4 to 13. Of the 23 nurses, 15 were married (65.2%) and 8 were single (34.8%); 11 identified as male (47.8%), while 12 identified as female (52.2%). Four nurses had earned a Master of Science degree, and 19 had Bachelor of Science degrees. While five of the nurses had worked for 4 months in the COVID-19 ward, 18 had 6 months of work experience there.
Of a total of 2000 initial codes created to describe the data, 30 primary categories were generated. Then, these 30 categories were reduced to seven main categories. These categories describe the main themes of nurse interviews and observational notes. The are: ‘patients’ complicated condition’, ‘severe nursing staff shortage’, ‘nursing professionalism’, ‘treatment team collaboration’, ‘work and environmental pressure’, ‘efficacy of care’, and ‘care deficit’.
3.1. Storyline
In order to clarify the core categories and the main processes, a storyline approach was used when integrating categories. According to this storyline, the context in this study was ‘COVID-19 patients’ nursing care’, and in this context and its accompanying features, ‘nursing care in the COVID-19 ward’ was considered as a phenomenon in this process. ‘Nursing professionalism’ was recognized as the strategy and the factor controlling the phenomenon. Intervening situations included ‘treatment team collaboration’ and ‘work and environmental pressure’. The causal conditions in the process path included ‘patients’ complicated condition’ and ‘severe nursing staff shortage’. The outcomes related to the strategy influenced by the interventional factors and causal conditions included ‘efficacy of care’ and ‘care deficit’ (Fig. 1).
Each of these categories will be discussed in turn to understand the process of care for COVID-19 patients in the studied hospital setting.
3.2. Patients’ Complicated Condition
Participants reported that the condition of patients with COVID-19 was complex and unpredictable, making it difficult to care for them. There was little definite information known about each patient’s condition, and there was a likelihood that patients might fall into a serious state and approach death at any moment. Participants repeatedly emphasized this complex situation in their statements.
‘Patients’ conditions may get worse at any moment. Their fever is out of control. Their breathing is not very good. We don’t know how complicated their condition will become.’ (Nurse No. 2)
‘It is unbelievable how easily a patient with shortness of breath may die. We cannot say how bad the patient’s condition will be in a few minutes’ time. Indeed, patients with COVID-19 have a very complicated condition.’ (Nurse No. 4)
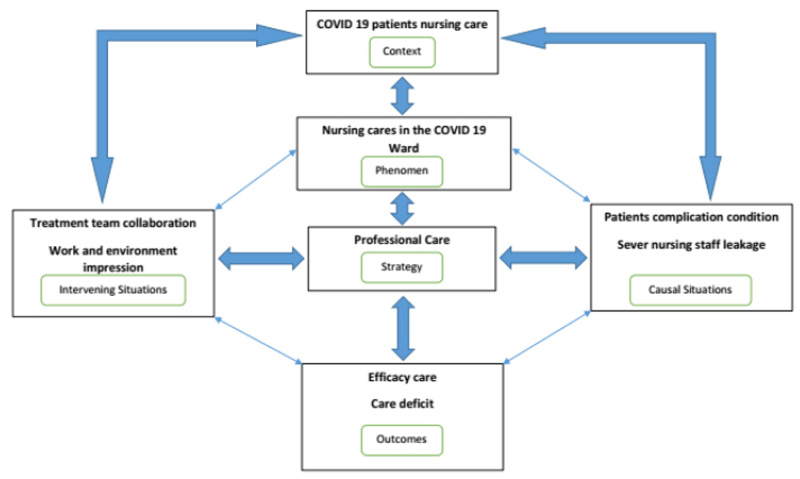 |
Fig. (1). The process of care for COVID-19 patients in hospital. |
Memo: ‘In fact, patients with COVID-19 were not physically stable, and this situation made the process of providing care difficult.’
‘The conditions of these patients are so complicated that nothing can be said. So far, I have not seen a patient with COVID-19 in a stable condition. One comes in with no symptoms, and suddenly their condition gets worse. Another comes in with just a simple fever, and suddenly needs a ventilator.’ (Nurse No. 9).
3.3. Severe Nursing Staff Shortage
All participants emphasized the lack of necessary nursing staff for providing adequate care to patients. They believed that the number of nursing staff in their ward, considering the very large number of patients and hospitalizations, was not enough to provide care to patients with COVID-19. They noted that the lack of nursing staff endangered the health of patients with COVID-19. In this regard, participants hoped for a solution that provided the necessary nursing staff to help manage patients’ deteriorating conditions and reverse their illness.
‘As you can see, we do not have enough staff, we do not have enough nurses. ... How can this small number of nurses cover these patients?’ (Nurse No. 5)
‘There are so many patients and hospitalizations, yet the number of our colleagues is not enough. ... Considering the number of hospitalizations, the number of nurses is very small. ... It is not enough at all; this is dangerous for our patients and their health.’ (Nurse No. 6)
‘It seems that this situation is getting worse, and we should think of a solution. If the nurses are not hired and the necessary staff are not provided, we will face serious problems such as patient mortality and shortage of nurses in the future.’ (Nurse No. 11)
‘If enough nurses are available, the care condition can be improved. ... Now that our number of nurses is limited, even those who are available cannot cover all this overcrowding. This is dangerous for our patients.’ (Nurse No. 15)
Memo: ‘Overcrowding refers to the high number of patients referred to the hospital and hospitalized there. What was observed was the low ratio of nurses to patients, which made the nurses’ work difficult.’
3.4. Nursing Professionalism
According to participants, one of nurses’ fundamental needs is sufficient knowledge and practical information to provide the necessary professional services to patients. Many emphasized the issue of professional nursing and practice based on ethical codes. However, they stated that the sudden outbreak of the COVID-19 pandemic caused nurses to be placed in the position of taking care of COVID-19 patients without any specific prior training. They emphasized the responsibility of nurses, as a matter of professional principle in such situations, to increase the quality and safety of care. They also stated that the nurses’ duty is to enhance their own practical effectiveness and to establish correct standards for providing professional care.
‘I have never had such an experience. .... I always say, “I wish I had already gained enough knowledge about such diseases and cared more professionally”, yet I try my best to work according to ethical codes and enhance my performance.’ (Nurse No. 3)
‘In order to provide better care, it is necessary for nurses to have the necessary knowledge about conditions such as this disease, so that they can act professionally and meet the needs of the patient.’ (Nurse No. 14)
‘It's hard for our nurses to think about the professionalism of their care at all, with all these difficulties ... but this isn’t still something that should be forgotten, that the kind of care becomes problematic. This is a principle in nursing, and the nurse should be responsible.’ (Nurse No. 8)
Memo: “Recently, a course was held for nurses regarding professionalism, and it had a positive effect on their statements.”
‘It is not possible to perform professional nursing well in this way ... yet our nurses do their best not to stay away from that aspect of professional nursing and ethical codes, to be accountable, and to be responsible for their work.’ (Nurse No. 1)
‘Considering these conditions, in such situations, it is better for our nurses to deal with the issue professionally and responsibly. This way, the patients’ safety is also guaranteed ... and the necessary care is provided to them.’ (Nurse No. 12)
3.5. Treatment Team Collaboration
According to participants, in the current conditions, the collaboration of all members of the treatment team involved in the care process of patients with COVID-19 had a significant impact on the improvement of patient health, including faster recovery and discharge. The higher the commitment of the members of the treatment team – including nurses, physicians, and each individual involved with the disease – the better the health of the patients, and the greater the reduction of workload and cost of treatment. Participants also mentioned the collaboration of the treatment team as a principle, saying that in this situation, everyone should stand by and facilitate the care and the treatment of patients with COVID-19.
‘All therapeutic staff, whether nurses, physicians or others, are seriously involved together and working tirelessly. ... These partnerships make the patient recover and get home sooner.’ (Nurse No. 7)
‘In this great crisis, the collaboration of the medical team is expected to be greater than before. ... Everyone here collaborates so that we can discharge the patient sooner.’ (Nurse No. 16)
‘One side of the collaboration is the treatment team and the other side are the patients and their families. ... In order for their patient to get well sooner, they expect all the medical staff, who work really well together, to be together and empathetic. In such a way, the patient can be discharged sooner, and the burden and the hospital costs will be reduced.’ (Nurse No. 19)
‘The collaboration of the treatment team greatly affects the morale of our patients and the speed of their recovery. ... Patients look happier when they see fellows working together so well.’ (Nurse No. 21)
Memo: ‘”Fellows” refers to the members of the treatment team. Being together, asking for each other’s ideas, and helping each other were among the things that were particularly observed among the different members of the treatment team. They helped each other a lot and strengthened each other's morale.’
3.6. Work and Environmental Pressure
Participants talked about daily stresses and constant anxiety during work shifts. On one hand, the difficulty and frequency of shifts, the lack of opportunity to relax, and the inadequacy of the facilities in some situations, such as treating patients’ acute conditions, increased the nurses’ workload. On the other hand, the inappropriate and inconvenient location of the COVID-19 ward within the hospital, in terms of commute and infection control, increased the environmental burden and its impact on nursing care in this ward. Workload and environmental pressure seriously affected nursing care from the participants’ points of view.
‘Sometimes the number of facilities is not enough. ... We are under pressure, so much pressure that I can no longer continue and work.’ (Nurse No. 7)
‘The location of our ward is not suitable; it is big and spacious. As soon as you have something to do and want to commute, it will put pressure on you, make you tired, and take your time.’ (Nurse No. 22)
‘I am so tired that I cannot rest due to the intensity of work and fatigue, as if I cannot sleep. A lot of pressure is on me and my colleagues. ... We all pray while caring for the patient; I hope nothing happens.’ (Nurse No. 1)
‘Stress, stress and stress ... fear and pressure … a ward of this area and so much work. ... It is really hard.’ (Nurse No. 13)
Memo: ‘There was disturbance, worry and urgency on [the participant’s] face.’
‘Ah, what can I say? The pressure is so great that there is no limit. We should always be careful for the patient. ... You see how big this hospital is and how many patients there are. It is getting very hard to work when the facilities are scarce, I mean, when there are no facilities, and at this time, the patient’s condition gets worse.’ (Nurse No. 17)
Memo: ‘The hospital was newly established; many of its wards were not set up; its staff was not fully supplied.’
‘Apart from all our workload, we always have this stress that every place in the ward cannot be completely isolated, that it is full of virus and can infect us, too. ... Of course, that is not impossible. ... I sometimes faint due to fatigue and high pressure while working with the patients.’ (Nurse No. 5).
3.7. Efficacy of Care
Particularly evident in participants’ interviews was their seriousness, self-sacrifice, unremitting effort and emphasis on scientific and accurate observance of knowledge-based nursing care for patients with COVID-19. Caregiving experiences made nurses stronger and more efficient in providing care, as well as their practical and scientific efforts to follow the right policies of care. They noted that effective care results in effective interaction in the treatment process.
‘It seems that a major change has occurred in everyone’s behaviour. We take great care of the patient, all care is efficient, principled and correct. We make sure that they are given good care. We are very careful about clinical inconsistencies and the patient’s condition; the patient should be given good care in all circumstances.’ (Nurse No. 21)
Memo: ‘”Clinical inconsistencies” refers to the existence of ambiguity in the patient’s files, such as medication orders, which nurses identify, report and clarify in order to prevent errors.’
‘The practice of our nurses is efficient, and they are highly skilled. ... We all try not to work outside the rules and regulations. ... Some of them work truly selflessly and share their experiences with others; even this has affected our relationship with our patients.’ (Nurse No. 20)
‘Very good care is given to the patients. Our relationship with the patient is excellent. Our nurses are strong and literate, and work with all their might. They all try their best to provide adequate care to the patients.’ (Nurse No. 6)
3.8. Care Deficit
According to participants, the fatigue of work and the loss of morale from the failure to treat some patients has led to care deficits and reduced the level and quality of nursing care, along with increasing the likelihood of errors and negligence during care. Care deficit has also occurred due to lack of staff, environmental stress and in some cases, due to lack of attention to nursing professionalism.
‘Ah, I see that in some cases, real services are not provided. Fatigue and workload cause a failure in care for the patient; and in this way, the quality of care may be decreased.’ (Nurse No. 18)
‘The small number of nurses, the very bad condition of the patients, and the lack of staff all increase the possibility of errors. Nurses do not like negligence, yet it may occur unconsciously in these difficult conditions.’ (Nurse No. 11)
‘Making mistakes isn’t impossible with these bad and messy conditions; everything has made our work difficult. Well, do you think everything can be done perfectly?’ (Nurse No. 9)
Memo: ‘The person expressed this in an angry manner.’
4. DISCUSSION
To answer the main question of the research, which was ‘What is the care process for patients with COVID-19?’, interviews with nurses were coded in detail, and based on emerging themes, seven main categories were generated to create a storyline and answer the research question: ‘patients’ complicated condition’, ‘severe nursing staff shortage’, ‘nursing professionalism’, ‘treatment team collaboration’, ‘work and environmental pressure’, ‘efficacy of care’, and ‘care deficit’.
Participants believed that COVID-19 patients’ complex conditions placed nursing care in an unpredictable situation. Although the complexity of nursing care has not yet been clearly defined in the literature – and there are many possible causes for it – unfixed and uncertain patient status can affect the provision of nursing care. In one study, authors concluded that the complexity of nursing care, as a potential concept, is characterized by the instabilities, variabilities and uncertainties that exist. The authors pointed out that the extent of the complexity of nursing care was related to patients’ problems and needs, as well as the extensive knowledge, experience, attention and caring skills of nurses [13]. Knowing the complexities of nursing care can improve attention and safety when caring for patients. Manning and Gagnon emphasized that cognition and transparency in the concept of care complexity are effective in improving medical care. They also discussed how the emergence of complex patients represents a diverse range of care [28]. For nurses in this study, patient care was complex because patients’ health status could deteriorate quickly and unpredictably. Furthermore, nurses were dealing with an illness that was still not well-understood at the time of the study, and with limited treatment options and resources. Because they were understaffed, they also had difficulty addressing emerging patient concerns or conditions quickly and effectively.
Nursing staff shortages have long been a concern of nurses, even before the COVID-19 pandemic. In this study, participants strongly emphasized the lack of nursing staff for providing care to patients with COVID-19. This shortage of nurses, while having an impact on the care provided, has serious and even debilitating consequences for nurses. Nurses play a vital role in providing hospital care. Haryanto explained that the shortage of nursing staff is a dynamic issue affecting all countries and healthcare systems, and this situation is critical for the provision of care [29]. Because nurses are at high risk of being infected with COVID-19, their vulnerability requires consideration of safety standards and protection to ensure that nurses themselves do not become infected, further reducing the availability of nurses in healthcare settings [30]. Rasmussen et al. argued that, although there has been a shortage of nurses during the COVID-19 pandemic, policymakers’ attitudes have changed towards the application of technology and digital education in care [31]. According to participants in this study, the most important effect of the shortage of nurses during the coronavirus disease has been that patients’ health has been seriously endangered.
The core concept expressed by participants in this study was ‘nursing professionalism’. Participants emphasized the effect of nursing professionalism on increasing patients’ satisfaction, on accountability and care safety and on providing care specifically to patients with COVID-19. Fallon discussed that although parallels may be drawn between challenges faced in nursing homes during the current pandemic, a professional approach, integration of evidence and providing the necessary and accountable care to these patients is necessary [32]. Jiang et al. argued that nurses should not only provide the necessary care to their patients, but also consider other aspects of patients’ lives, including social and cultural aspects. They must adapt themselves to current conditions, a tactic that should implicitly be a feature of professional nursing [33]. This important role of nurses and their role in society during the pandemic has led to a sense of satisfaction and a change in society’s view of nurses. O'Connor et al. noted that nursing practice should be provided within a completely ethical and clear framework, considering values such as care, compassion, dignity, kindness, support, self-empowerment and communication as essential requirements of professional nursing [34]. To achieve professional nursing, Eid et al. recommended strengthening performance and action based on codes of professional ethics and considered having a type of nursing profession as a prerequisite for accountable care [35]. Participants in this study expressed concern that because of their workload and a lack of specific training to treat COVID-19 patients, they were unable to perform their jobs at the highest level of professionalism. Many of them took advantage of a professionalism course that was offered during the time of the research study. When unsure of what to do, they often turn to ethical codes to guide their decision making.
Nurses in this study expressed belief that the collaboration of medical team members leads to the promotion of health and faster recovery of patients; so, those partnerships are considered as a factor in controlling treatment costs and better management of patients with COVID-19. Zakerimoghadam et al. argued that collaboration among medical staff is significant in providing appropriate care to patients and enhancing their recovery process. Collaboration between the members of the treatment team, as complements to each individual’s role, is obvious and inevitable [36]. In one study on the significant impact of collaboration of a treatment team in promoting the safety and health of patients, Alsallum et al. considered it important to increase awareness of this collaboration and recommended removing the barriers to this collaboration when providing services and care to patients [37]. In another study, Kang et al. concluded that improving the process of cooperation and collaboration between nurses, physicians and the treatment team can lead to improved outcomes in treatment and care [38]. Participants in this study felt that the ‘crisis’ of COVID-19 necessitated their collaboration more than ever, and that their teamwork improved both their own and patients’ morale.
The various stresses and factors in providing care to COVID-19 patients made workload and environmental pressures a high concern of nurses in this study. Riedl et al. found that work pressure on nurses causes emotional exhaustion in the workplace, and the effects of this go beyond work [39]. Leary et al. referring to the deep understanding of the nursing profession concluded that specialization and attention to professional strengthening factors can result in the development of the nursing profession and the provision of professional care [40]. Copanitsanou et al. emphasized several factors that affect nursing care and the burnout of nurses, including the work environment. They believed that a good work environment is effective in increasing patients’ satisfaction as well as increasing nurses’ job satisfaction and reducing burnout [41]. Therefore, it can be inferred that having a suitable work environment will increase the quality of care and enhance recovery.
Nurses in this study made clear that efficacy of care, the observance of instructions and the application of nursing knowledge all serve to improve the level of nursing care, while care deficit – due to the factors causing it – increases the incidence of errors and reduces the level of nursing care possible. Amoah et al. considered good communication to be an indispensable part of patient care; this is crucial in determining the quality of care and for helping to remove its barriers, including environmental barriers [42]. Larrabee et al. considered the provision of immediate and efficient care, being able to meet the needs of patients and the competence of nurses to be effective factors in nursing care [43]. In one study on the influence of nurse characteristics and work conditions on the quality of nursing care, Mudallal et al. concluded that work conditions have the greatest impact on the quality of care [44]. Care deficit occurs as a result of poor work conditions for nurses, and ultimately it reduces the level and quality of care. Although nurses in this study were extremely positive about their efficacy of care, stating that in all circumstances, the best care was given to the best of their ability, they also expressed a myriad of complaints about limitations that made their jobs more difficult and prevented them from providing their highest level of care. These limitations included fatigue, high workload, staff shortage, and the poor health conditions of patients.
The most important limitation of this study was the special circumstances related to the COVID-19 ward. Additionally, because of the contagious nature of COVID-19, interviews could not be conducted in a traditional manner; however, this limitation was eliminated after explaining the objective of the study to participants and using remote interviewing methods for data collection.
CONCLUSION
Nurses are newly facing challenges of the complexity of nursing care for COVID-19, the challenges of providing care to contagious patients while also protecting themselves, and the novelty of information regarding caring for these patients. Thus, it is necessary for plans to be made to develop guidelines and care policies in the field of nursing management, as well as to determine educational needs and opportunities to provide up-to-date information for nurses to strengthen their scientific capacity in the field of education. New research priorities must be determined to ensure that nurses have clear processes for providing the best care to patients and to themselves in the midst of a pandemic.
Policymakers and nursing managers can apply the current process in the clinical setting to enhance the performance and knowledge of nursing professionals, to improve patients’ health and to increase the quality and safety of nursing care provided to patients with COVID-19. Positive developments in nursing care can be made by considering the dynamics of the concept of care, as well as strengthening the necessary competencies, as well as considering the environmental and non-environmental conditions affecting the care of these patients.
STRENGTHS AND LIMITATIONS OF THIS STUDY
- This paper is the first to explore the nursing care process specifically for patients with COVID-19.
- Seven main categories were determined from thematic analysis of interviews with nurses working in a COVID-19 ward, regarding the process of care for patients in the ward: ‘patients’ complicated condition’, ‘severe nursing staff shortage’, ‘nursing professionalism’, ‘treatment team collaboration’, ‘work and environmental pressure”, ‘efficacy of care’, and ‘care deficit’.
- The core concept was determined to be ‘nursing professionalism’. Participants in this study emphasized the effect of demonstrating professional nursing practices on increasing patients’ satisfaction, accountability, care safety and responsibility when providing care to patients with COVID-19.
- The most important limitations in this study were the special circumstances related to working in the COVID-19 ward, including visiting the ward and conducting interviews.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the Institutional Review Board of Yasuj University of Medical Sciences (approval number 990109).
HUMAN AND ANIMAL RIGHTS
No animals were used as the basis of this study. This research was conducted according to the 1964 Declaration of Helsinki principles, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author [M.B], on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
We thank all the nurses who helped us conduct this research. The authors appreciate Dr. Hossein Mari Oryad, Deputy of the Research Center of Yasuj University of Medical Sciences, for financial support.
REFERENCES
| [1] | Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020; 91(1): 157-60. |
| [2] | WHO. 2022. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200724-covid-19-sitrep-186.pdf?sfvrsn=4da7b586_2 |
| [3] | Eghbali M, Negarandeh R, Froutan R. COVID-19 epidemic: Hospital-level response. Nurs Pract Today 2020; 7(2): 81-3. |
| [4] | Wei H, Corbett RW, Ray J, Wei TL. A culture of caring: the essence of healthcare interprofessional collaboration. J Interprof Care 2020; 34(3): 324-31. |
| [5] | Coronado-Vázquez V, Canet-Fajas C, Ramírez-Durán MV, et al. Nursing care ethical implications regarding chronic patients at hospital discharge. Healthcare 2020; 8(2): 167. |
| [6] | Recio-Saucedo A, Dall’Ora C, Maruotti A, et al. What impact does nursing care left undone have on patient outcomes? Review of the literature. J Clin Nurs 2018; 27(11-12): 2248-59. |
| [7] | Vega H, Hayes K. Blending the art and science of nursing. Nursing 2019; 49(9): 62-3. |
| [8] | Locsin RC. The co-existence of technology and caring in the theory of technological competency as caring in nursing. J Med Invest 2017; 64(1.2): 160-6. |
| [9] | Hawke-Eder S. Can caring be taught? Nurs N Z 2017; 23(3): 23-25, 46. |
| [10] | Grove SK, Gray JR. Understanding Nursing Research E-Book: Building an Evidence-Based Practice 2018. |
| [11] | Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017; 9(4): 30-5. |
| [12] | Zwakhalen SMG, Hamers JPH, Metzelthin SF, et al. Basic nursing care: The most provided, the least evidence based - A discussion paper. J Clin Nurs 2018; 27(11-12): 2496-505. |
| [13] | Huber E, Kleinknecht-Dolf M, Kugler C, Spirig R. Patient-related complexity of nursing care in acute care hospitals - an updated concept. Scand J Caring Sci 2021; 35(1): 178-95. |
| [14] | Daly J, Jackson D, Anders R, Davidson PM. Who speaks for nursing? COVID-19 highlighting gaps in leadership. J Clin Nurs 2020; 29(15-16): 2751-2. |
| [15] | Shanthanna H, Strand NH, Provenzano DA, et al. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia 2020; 75(7): 935-44. |
| [16] | Shen Y, Li C, Dong H, Wang Z, Martinez L, Sun Z, et al. Airborne transmission of COVID-19: epidemiologic evidence from two outbreak investigations 2020. Available from:
https://www. researchgate. net/publication/340418430_Airborne_transmission_of_COVID-19_epidemiologic_evidence_from_two_ |
| [17] | Alharbi J, Jackson D, Usher K. The potential for COVID19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs 2020; 29(15-16): 2762-4. |
| [18] | Liang T. Handbook of COVID19 prevention and treatment 2020. |
| [19] | Burke RM, Midgley CM, Dratch A, et al. Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. MMWR Morb Mortal Wkly Rep 2020; 69(9): 245-6. |
| [20] | Huang L, Lin G, Tang L, Yu L, Zhou Z. Special attention to nurses’ protection during the COVID-19 epidemic. Crit Care 2020; 24(1): 120. |
| [21] | Reper P, Bombart MA, Leonard I, Payen B, Darquennes O, Labrique S. Nursing Activities Score is increased in COVID-19 patients. Intensive Crit Care Nurs 2020; 60: 102891. |
| [22] | Desborough J, Banfield M, Phillips C, Mills J. The process of patient enablement in general practice nurse consultations: a grounded theory study. J Adv Nurs 2017; 73(5): 1085-96. |
| [23] | Goes MG, de Brum CN. Application of constructivist grounded theory in nursing research. Qual Rep 2016; 21(13): 48-53. |
| [24] | Singh S, Estefan A. Selecting a grounded theory approach for nursing research. Global qualitative nursing research. Glob Qual Nurs Res 2018; 5: 1-9. |
| [25] | Corbin J, Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory 2014. |
| [26] | Howard-Payne L. Glaser or Strauss? Considerations for selecting a grounded theory study. S Afr J Psychol 2016; 46(1): 50-62. |
| [27] | Polit DF, Beck CT. Essentials of nursing research: Appraising evidence for nursing practice 2010. |
| [28] | Manning E, Gagnon M. The complex patient: A concept clarification. Nurs Health Sci 2017; 19(1): 13-21. |
| [29] | Haryanto M. Nursing shortage: Myth or fact? Orthop Nurs 2019; 38(1): 1-2. |
| [30] | Jackson D, Anders R, Padula WV, Daly J, Davidson PM. Vulnerability of nurse and physicians with COVID-19: Monitoring and surveillance needed. J Clin Nurs 2020; 29(19-20): 3584-7. |
| [31] | Rasmussen S, Sperling P, Poulsen MS, Emmersen J, Andersen S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet 2020; 395(10234): e79-80. |
| [32] | Fallon A, Dukelow T, Kennelly SP, O’Neill D. COVID-19 in nursing homes. QJM 2020; 113(6): 391-2. |
| [33] | Jiang L, Broome ME, Ning C. The performance and professionalism of nurses in the fight against the new outbreak of COVID-19 epidemic is laudable. Int J Nurs Stud 2020; 107: 103578. |
| [34] | O’Connor S, Chu CH, Thilo F, Lee JJ, Mather C, Topaz M. Professionalism in a digital and mobile world: A way forward for nursing. J Adv Nurs 2020; 76(1): 4-6. |
| [35] | Eid AG, Ahmed MZ, Safan SM, Mohamed SM. Nursing professionalism: a concept analysis. Menoufia Nurs J 2018; 3(2): 87-96. |
| [36] | Zakerimoghadam M, Ghiyasvandian S, Kazemnejad Leili A. Nurse-physician collaboration: the attitudes of baccalaureate nursing students at tehran university of medical sciences. Iran Red Crescent Med J 2015; 17(4): e23247. |
| [37] | Alsallum FS, Banakhar MA, Gattan SK, Alwalani SA, Alsuhaim RA, Samarkandi RA. Nurses’ and physicians’ attitudes towards nurse-physician collaboration in critical care. Glob J Health Sci 2020; 12(1): 149. |
| [38] | Kang XL, Brom HM, Lasater KB, McHugh MD. The association of nurse-physician teamwork and mortality in surgical patients. West J Nurs Res 2020; 42(4): 245-53. |
| [39] | Riedl EM, Thomas J. The moderating role of work pressure on the relationships between emotional demands and tension, exhaustion, and work engagement: An experience sampling study among nurses. Eur J Work Organ Psychol 2019; 28(3): 414-29. |
| [40] | Leary A, Maclaine K, Trevatt P, Radford M, Punshon G. Variation in job titles within the nursing workforce. J Clin Nurs 2017; 26(23-24): 4945-50. |
| [41] | Copanitsanou P, Fotos N, Brokalaki H. Effects of work environment on patient and nurse outcomes. Br J Nurs 2017; 26(3): 172-6. |
| [42] | Amoah VMK, Anokye R, Boakye DS, et al. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs 2019; 18(1): 4. |
| [43] | Larrabee JH, Bolden LV. Defining patient-perceived quality of nursing care. J Nurs Care Qual 2001; 16(1): 34-60. |
| [44] | Mudallal RH, Saleh MY, Al-Modallal HM, Abdel-Rahman RY. Quality of nursing care: The influence of work conditions and burnout. Int J Afr Nurs Sci 2017; 7: 24-30. |









