RESEARCH ARTICLE
Incidence of Preterm Infants, Indications of Admission, Risk Factors, and Discharge Outcome: A Retrospective Study
Atyat Mohammed Hassan1, 2, *
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187443462203250
Publisher ID: e187443462203250
DOI: 10.2174/18744346-v16-e2203250
Article History:
Received Date: 20/12/2021Revision Received Date: 1/2/2022
Acceptance Date: 3/3/2022
Electronic publication date: 31/05/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Prematurity is still a major cause of neonatal and infant mortality and morbidity.
Aim:
This study aimed to describe the incidence of preterm infants, indications of admission, risk factors, and discharge outcome.
Materials and Methods:
A retrospective, descriptive design was used. A sample of 692 preterm infants admitted to the Neonatal Intensive Care Unit (NICU) was included. A structured sheet was used to gather the necessary data. It involved two parts: characteristics of preterm infants and their mothers and risk factors concerning preterm birth.
Results:
The study found that 49.4% of admitted neonates were preterm; among them, 48.1% died on discharge. Moreover, there were significant relations between the type of gestation (p=0.000), mothers' age (p=0.001), anemia, pregnancy-induced hypertension, preeclampsia, antepartum hemorrhage, premature rupture of membranes, obstructed labor, family history of medical diseases, and mothers' history of medical diseases with preterm infants' gestational age (p=0.01, 0.001, 0.02, 0.01, 0.000, 0.000, 0.000, 0.000, respectively). Moreover, it was observed that higher admission of preterm infants who had respiratory problems, followed by gastrointestinal problems.
Conclusion:
There was a higher prevalence with a higher mortality rate of admitted preterm infants to NICU. Likewise, the type of gestation, mothers' age, presence of complications during pregnancy, bad obstetric history, and family and medical history of diseases were the most common risk factors of prematurity. Moreover, respiratory problems were the main etiology for admission of preterm infants to NICU. Therefore, early screening of diseases and obstetric complications during pregnancy is recommended.
Implications for Nursing Practice:
Providing educational programs for pediatric nurses will increase their level of awareness regarding incidence, indications, risk factors, and discharge outcome of prematurity, thus reducing the rate of mortality and morbidity among preterm infants.
1. INTRODUCTION
Worldwide, of the 130 million neonates born every year, 15 million neonates are born preterm. Moreover, prematurity is still a major cause of neonatal and infant mortality and morbidity and a significant contributor to long-term adverse health outcomes [1, 2]. About 123.13% of preterm births at 32 to less than 37 weeks of gestation are reported in Egypt. This statistic may indicate a higher rate of admission to the NICU every year [3]. A study by Algameel et al. [4], conducted in Upper Egypt, indicated that 28% of the studied neonates were late preterm infants.
Infants born preterm have a higher risk for mortality, as indicated by a study conducted in low and middle-income countries [5]. This greater risk for mortality has frequently been pertaining to neonatal sepsis [6]. Moreover, they have a higher risk for short- and long-term complications, such as neurological, cognitive, and motor disorders. Likewise, they are more prone to malnutrition, chronic illnesses, and early death [7].
The delivery of preterm infants has been linked to many factors. Studies conducted by Kildea et al. [8] and Savitz and Murnane [9] found that ethnicity, mothers' age, and smoking are risk factors for preterm birth. Others identified that mothers' education is also a risk factor for preterm birth [10-12]. Whereas Delnord et al. [13] reported that mothers' parity is a risk factor for preterm birth. Additionally, lack of antenatal care leads to poor pregnancy outcomes, such as preterm births [14].
Moreover, Gurung et al. [15] determined that mothers' age, education, smoking habits, lack of antenatal care, multiple deliveries, and severe anemia are risk factors for preterm birth. Besides, other studies revealed that interventions, such as labor induction and cesarean section (C.S), attributed to preterm birth [16, 17]. Hosnya et al. [18] found that factors like mothers' age, history of abortion, antepartum bleeding, prenatal infection, and premature rupture of membranes (PROM) are prominent factors for preterm birth.
There are many factors that indicate the admission of preterm infants to NICU, such as respiratory distress syndrome (RDS), feeding difficulties, apnea, neonatal jaundice (NJ), necrotizing enterocolitis (NEC), hypoglycemia, neonatal sepsis (NS), intraventricular hemorrhage (IVH), and temperature instability [19]. Despite care at NICU, immaturity at birth has a lifelong impact on various systems [19], disabilities, and delayed neurodevelopment, such as learning, hearing, and visual complications [20]. Moreover, a short-term impact increases with decreasing gestational age [21]. Therefore, detecting and interpreting the risk factors, indications of admission, and outcomes for prematurity can aid in identifying this problem.
1.1. Significance of the Study
The pediatric nurse plays an important role in preventing the birth of a preterm infant by knowing the risk factors and etiology. These will be achieved by applying the prevention levels: Firstly, providing primary prevention to prevent the birth of a preterm infant. It is applied in the preconception period by working on healthy women and decreasing the introduction to risk factors and vulnerability. Secondly, providing secondary prevention at the prenatal time through early detection of these factors. Finally, preventing complications and providing tertiary prevention and rehabilitation to improve outcomes for this category of infants at the postnatal period.
2. MATERIALS AND METHODS
2.2. Setting
This study was implemented at the Neonatal Intensive Care Unit (NICU). The NICU is affiliated with Assiut University Children's Hospital. It has more than fifty incubators. It serves Upper Egypt Governorates from El-Minia to the Red Sea.The average admission during 2018 was about 1500 high-risk neonates with 127 admitted cases/ month.
2.3. Subjects
A sample of 692 preterm infants admitted to the NICU during the period from the 1st January to 31st December, 2016, was included. Where the total number of high-risk neonates admitted to NICU was 1400. The study subjects included retrospectively all high-risk neonates having gestational age less than 37 weeks. Gestational age assessment was based on the clinical assessment done by neonatologists and documented in the medical records.
2.4. Data Collection Tools
A structured sheet was used to gather the necessary data for this study. It involved two parts as the following:
Part one: Characteristics of preterm infants and their mothers: It included gestational age, gender, delivery type, type of gestation, discharge outcome, and indications of admission to NICU. Mothers’ age, occupation, and parents' consanguinity.
Part two: Risk factors concerning preterm birth: It included mothers' obstetric history, gravidity, parity, abortion, stillbirths, and neonatal death numbers. Family and mothers' history of medical disease and complications during the current pregnancy. It included the presence of anemia, gestational diabetes, pregnancy-induced hypertension (PIH), preeclampsia, taking medications during pregnancy, rheumatic heart disease, antepartum hemorrhage (APH), PROM, polyhydramnios, and oligohydramnios.
2.5. Methods
Official permission was secured from the head of NICU after clarifying the study aim. The tool of data collection was established by the researcher after reviewing the related literature. The content validity of the tool was done by five experts in the field of pediatric nursing and pediatrics, and it was 0.89. Cronbach's alpha coefficient was used to examine the internal consistency, and it was r=0.83. After that, a pilot study was carried out for 10% of the studied preterm infants (70 neonates). It was implemented to check the applicability and feasibility of the tool. The pilot study participants were included in the study sample without any modifications. The data were collected by the researcher during the period of five months from April to September, 2017, during the morning and afternoon shift, two days/week.
2.6. Ethical Considerations
The Ethical Committee of the Faculty of Nursing, Assiut University, approved the research proposal (IRB No: 3370034). Likewise, written consent was obtained from the director of Assiut University Children's Hospital and the head of NICU. The researchers ensured that the collected data would be used only for the aim of the study. Confidentiality and anonymity were assured.
2.7. Data Analysis
Data were entered and analyzed using the Statistical Package for Social Science software (SPSS) version 20.0. Descriptive statistics were presented in the form of frequencies and percentages as qualitative variables. Likewise, means and standard deviations were used for quantitative variables. The variables were compared using correlation coefficient and chi-square test. The p-value was considered significant at P =≤ 0.05.
3. RESULTS
Fig. (1) indicates that 49.4% were preterm infants and 50.6% were full-term neonates.
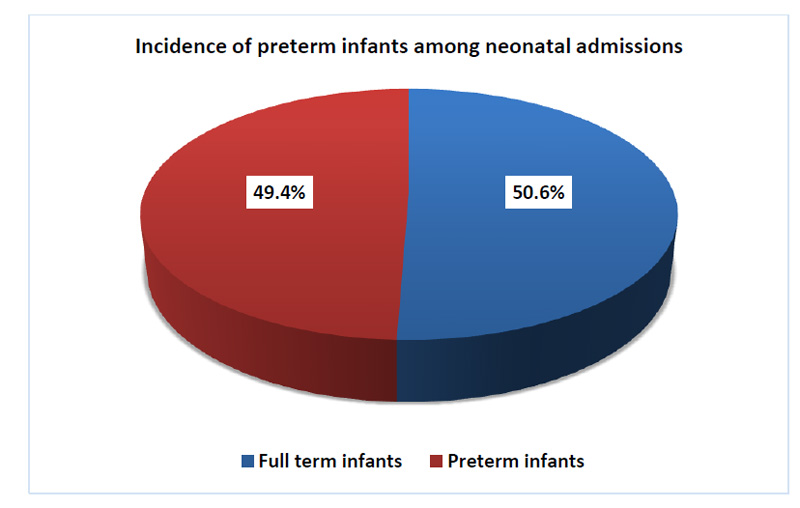 |
Fig. (1). Incidence of preterm infants among neonatal admissions (N=1400). |
| Characteristics | No. | % | r | P-value |
|---|---|---|---|---|
| Gender: | ||||
| • Male | 421 | 60.8 | -0.07 | 0.06 |
| • Female | 271 | 39.2 | ||
| Type of gestation: | ||||
| • Single | 541 | 78.2 | -0.2 | 0.000 |
| • One of the twins | 126 | 18.2 | ||
| • One of the triples or more | 25 | 3.6 | ||
| Delivery type: | ||||
| • Normal vaginal delivery (NVD) | 233 | 33.7 | 0.05 | 0.1 |
| • Elective CS | 178 | 25.7 | ||
| • Emergency CS | 281 | 40.6 | ||
| Mothers' age/years | ||||
| • <20 | 90 | 13.0 | -0.1 | 0.001 |
| • 20- | 362 | 52.3 | ||
| • 30- | 216 | 31.2 | ||
| • 40 and more | 24 | 3.5 | ||
| Mean ± SD (Max-Min) | 26.7 ± 6.3 (14-46) | |||
| Mothers' occupation: | ||||
| • Not working | 524 | 75.7 | -0.03 | 0.5 |
| • Working | 168 | 24.3 | ||
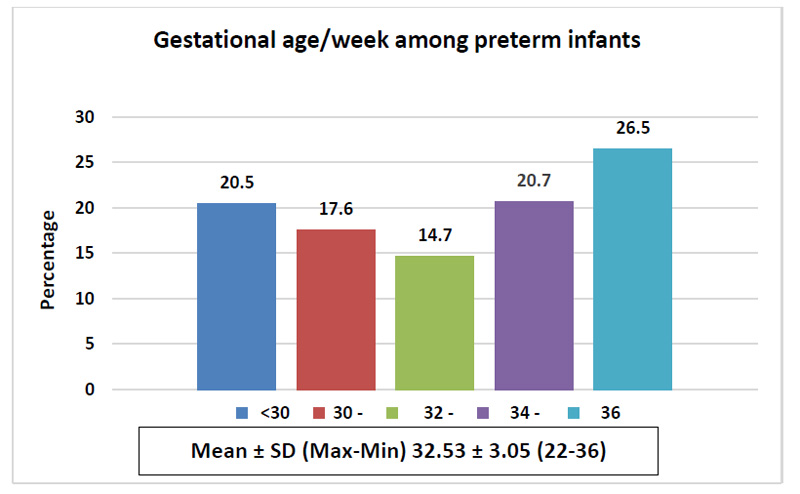 |
Fig. (2). Gestational age/week of preterm infants (n=692). |
Fig. (2) shows that 26.5% of preterm infants were born at 36 weeks. Moreover, 20.7% and 20.5% of them were born at 34-<36 and <30 weeks, respectively. The mean gestational age was 32.53±3.05.
Table 1 reveals that 60.8% were males, and 78.2% were born in a single gestation. Moreover, 40.6 were delivered by emergency C.S. Furthermore, 52.3% of mothers were aged 20-<30 years old, and 75.7% of them were not working. Moreover, there were statistically negative correlations between the type of gestation (r=-0.2, p=0.000) and mothers' age (r=-0.1, p=0.001) with the gestational age of preterm infants.
Fig. (3) illustrates that 48.1% of admitted preterm infants died while 51.9% of them were stable on discharge with a statistically negative correlation (r=-0.3, p=0.000).
Table 2 demonstrates statistically positive correlations regarding family history of medical diseases (r=0.4, p=0.000*) and mothers' history of medical diseases (r=0.1, p=0.000*) with the gestational age of preterm infants. While there were no statistically negative correlations regarding mothers' gravidities, parity, and abortion numbers (r=-0.01, p=0.6, and r=-0.03, p=0.4, r=-0.01, p=0.6) respectively, and gestational age of preterm infants.
Table 3 detects statistically significant differences concerning mothers' complications during current pregnancy; anemia (p=0.01*), PIH (0.001*), preeclampsia (p=0.02*), APH (0.01*), PROM (p=0.000*), and obstructed labor (p=0.000*) and gestational age of preterm infants.
Table 4 identifies respiratory problems as the main etiology for preterm infants' NICU admission; 28.9% and 28.3% were RDS and RD, respectively. Followed by gastrointestinal; POI and NJ were 22.5% and 14.2%, respectively, CA were 16.6%, neurological causes; poor reflexes were 13.9%, and NS was 13.8%.
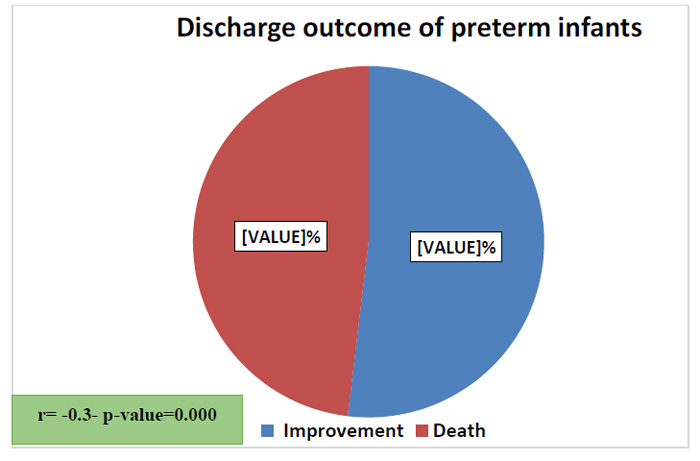 |
Fig. (3). Discharge outcome of preterm infants (n=692). |
| History* | No. | % | r | P-value |
|---|---|---|---|---|
| 1. Obstetric history | ||||
| 1) Gravidity number | ||||
| • Primigravida | 169 | 24.4 | -0.01 | 0.6 |
| • <5 | 388 | 56.1 | ||
| • ≥5 | 135 | 19.5 | ||
| Mean ± SD (Max-Min) | 2.9 ± 2.0 (1-15) | |||
| 2) Parity number | ||||
| • Primipara | 146 | 21.1 | -0.03 | 0.4 |
| • <5 | 457 | 66.0 | ||
| • ≥5 | 89 | 12.9 | ||
| Mean ± SD (Max-Min) | 2.7 ± 1.5 (1-12) | |||
| 3) Abortions number | ||||
| • 1-2 | 178 | 25.7 | -0.01 | 0.6 |
| • 3 and more | 38 | 5.5 | ||
| 4) Still births number | 19 | 2.7 | 0.01 | 0.8 |
| 5) Neonatal deaths number | 31 | 4.5 | 0.06 | 0.08 |
| 2. Family history of medical diseases | 53 | 7.7 | 0.4 | 0.000* |
| 3. Mothers' history of medical diseases | 166 | 24.0 | 0.1 | 0.000* |
| Complications* | No | % | X2 | P |
|---|---|---|---|---|
| • Anemia | 96 | 13.9 | 42.9 | 0.01 |
| • Gestational diabetes | 36 | 5.2 | 11.3 | 0.5 |
| • PIH | 69 | 10.0 | 34.2 | 0.001* |
| • Preeclampsia | 25 | 3.6 | 25.9 | 0.02* |
| • Taking medications during pregnancy | 128 | 18.5 | 1.3 | 0.9 |
| • Rheumatic heart disease | 7 | 1.0 | 15.0 | 0.3 |
| • APH | 66 | 9.5 | 27.5 | 0.01* |
| • PROM | 112 | 16.2 | 50.3 | 0.000* |
| • Polyhydramnios | 10 | 1.4 | 24.0 | 0.5 |
| • Oligohydramnios | 11 | 1.6 | 24.1 | 0.5 |
| • Obstructed labor | 9 | 1.3 | 58.0 | 0.000* |
| Indications of admission* | No | % |
|---|---|---|
| Respiratory problems: | ||
| • Respiratory distress syndrome (RDS) | 200 | 28.9 |
| • Respiratory distress (RD) | 196 | 28.3 |
| • Meconium aspiration syndrome | 12 | 1.7 |
| • Apnea | 36 | 3.8 |
| • Need mechanical ventilation | 17 | 2.5 |
| • Cyanosis | 16 | 2.3 |
| Gastrointestinal problems: | ||
| • Neonatal jaundice (NJ) | 98 | 14.2 |
| • Poor oral intake (POI) | 156 | 22.5 |
| • Necrotizing entercolitis (NEC) | 2 | 0.3 |
| Endocrine problems: | ||
| • Infant of diabetic mother (IDM) | 36 | 5.2 |
| Blood problems: | ||
| • Intraventricular hemorrhage (IVH) | 13 | 1.9 |
| • Severe pallor | 13 | 1.9 |
| Neurological problems: | ||
| • Neonatal convulsion (NC) | 14 | 2.0 |
| • Poor reflexes | 96 | 13.9 |
| Renal problems: | ||
| • Renal etiology | 6 | 0.9 |
| Birth weight problems: | ||
| • IUGR | 42 | 6.1 |
| • LBW | 20 | 2.9 |
| Other problems: | ||
| • Neonatal sepsis (NS) | 110 | 13.8 |
| • Congenital anomalies (CA) | 115 | 16.6 |
4. DISCUSSION
The largest number of developing countries lack reliable data on the incidence of preterm labor [2]. Therefore, this study aimed to define the incidence of preterm infants' admission at the neonatal Intensive Care Unit, indications, risk factors, and discharge outcome.
This retrospective study found a higher incidence (49.4%) of admitted neonates at the NICU that were born preterm; of 1400 high-risk neonates, 692 were born preterm. This finding was supported by the study conducted by Khasawneh et al. [22] in Jordan, who found that 56% of preterm births required admission to NICU. Moreover, Khasawneh et al. [23] indicated that the main indication for NICU admission was prematurity, representing 33.3% among the whole study cohort. Likewise, Abdelhady and Abdelwahid [3] revealed a higher admission rate of preterm neonates from 32 to less than 37 weeks. Moreover, a study conducted by Kuppusamy and Vidhyadevi [19] found that 28.25% of the total NICU admission were preterm infants. The higher incidence in this study could be due to the higher admissions of high-risk neonates to the NICU than other intermediate care units for neonates. Besides, this NICU is the main NICU in Upper Egypt and receives many referrals, leading to higher admission rates. Therefore, this demonstrates that preterm birth is a significant health problem.
Additionally, it was noticed that more than one-fourth of the studied preterm infants were born at 36 weeks with a mean gestational age of 32.53±3.05. This result was in the same line with the findings of studies conducted by Abdel Razeq et al., Al-Qurashi et al., and Abdelhady and Abdelwahid [3, 24, 25]. Moreover, Khasawneh and Khriesat [23] found that late preterm at 36 weeks of gestation accounted for a higher rate (75%) of NICU admission among all premature births. This result might be demonstrated by increasing use of assisted reproduction, higher rates of labor induction, and increased rates of C.S delivery.
The present study found statistically negative correlations between the type of gestation and gestational age of preterm infants, indicating that mothers who had multiple gestations were more prone to deliver preterm. This finding was in the same line with the findings of Gurung et al. [15] and Kuppusamy and Vidhyadevi [19], where they found that multiple gestations were significant risk factors of preterm birth. Other studies done in Korea by Kim et al. [26] and in Bangladesh by Shah et al. [27] demonstrated the same results. This finding could be attributed to the fact that multiple gestations cause distension of the uterus, leading to early labor.
Moreover, statistically negative correlations between mothers' age and gestational age of preterm infants showed that the mothers' age is a significant factor that increases the risk of delivery of a preterm infant. This result was reinforced by the findings of Gurung et al. [15], who indicated that preterm births are higher among younger mothers. Numerous other studies also reported an association between younger and older mothers and preterm birth [28-31]. This result might be attributed to younger mothers having less experience concerning pregnancy complications and outcomes. In comparison, older ones might have health risk factors.
Moreover, it was observed that nearly half of the studied sample was dead on discharge. This was supported by the findings of Gurung et al., Sania et al., and Draper et al. [15, 32, 33]. Moreover, KC et al. [34] found a 12-fold increased risk of neonatal death among preterm infants compared to full-term. This higher incidence of mortality rate among the studied preterm infants might be due to the higher frequency of very (<32 weeks) and extremely (<28 weeks) preterm infant incidence.
The study reported statistically positive correlations between family history of medical diseases and mothers' history of medical diseases with preterm infants' gestational age. These findings were in agreement with the findings of studies conducted by Aregawi et al., Ticaria et al., and Mohsenzadeh et al. [35-37], who found that maternal medical complications as chronic diseases are a risk factor for preterm birth. These findings could be due to the major adverse effects of medical diseases on mothers' health in general and in pregnancy specifically.
Furthermore, the study determined that mothers who had anemia, PIH, preeclampsia, APH, PROM, and obstructed labor during pregnancy are more at risk for preterm birth. These results were concurrent with many studies conducted by Hosnya et al., Gurung et al., Aregawi et al., and Wagura et al. [2, 15, 18, 35], who found that PIH, APH, and PROM are significant risk factors for preterm labor. Likewise, the results by Kuppusamy and Vidhyadevi [19] revealed that anemia, PROM, and PIH are the most common associated factors for prematurity. Moreover, Mohsenzadeh et al. [37] indicated that PROM and preeclampsia are significant risk factors for preterm birth. Moreover, a study conducted in Egypt by El Beltagy et al. [38] had the same results. The researchers agreed that these findings were due to the direct negative effects of these complications on mothers' health during pregnancy and, therefore, on the health of the fetus.
Finally, the study findings identified that respiratory causes are the main etiology for preterm infants' NICU admission as RDS and RD, followed by gastrointestinal poor oral intake and NJ, CA, neurological problems, such as poor reflexes, and NS. These results were similar to the results of Khasawneh and Khriesat [23], who demonstrated that preterm infants had higher rates of RDs and sepsis. Moreover, a study by Algameel et al. [4] conducted in Upper Egypt found that jaundice and respiratory morbidity were increased among preterm infants. These results could be due to premature birth; the neonates had immature lungs and lacked sufficient surfactant for normal lung expansion, leading to a higher frequency of RD and RDs.
The limitation of this study is the retrospective design where all the inferred data reflect what is recorded and reported in the medical records. Thus, specific outcomes might be overestimated or underestimated. Although this study was conducted at a large university hospital, the findings cannot represent the whole Egyptian population; therefore, a conclusion about the generalizability of the findings cannot be accurately made.
CONCLUSION
A higher prevalence with a higher mortality rate of admitted preterm infants to NICU was reported. Likewise, the type of gestation, mothers' age, presence of complications during pregnancy, bad obstetric history, and family and medical history of diseases were found to be the most common risk factors of prematurity. Moreover, respiratory problems were the main etiology for admission of preterm infants to NICU. Therefore, early screening of diseases and obstetric complications during pregnancy is recommended.
RECOMMENDATIONS
Following strategies can be recommended:
- Raising public and professional health awareness of the risk factors linked to prematurity.
- Implementing educational programs for early detection and intervention for short-term and long-term complications.
- Local strategies and policies should be established and implemented to improve the outcome of birth through early screening of diseases and obstetric complications.
- Increasing mothers' awareness about the importance of antenatal care and follow-up. Therefore, early detection and intervention of complications can be done.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research proposal was approved by the Ethical Committee of the Faculty of Nursing, Assiut University, (IRB No: 3370034).
HUMAN AND ANIMAL RIGHTS
No experimentation was taken place due to the retrospective nature of the study.
CONSENT FOR PUBLICATION
Written consent was obtained from the director of Assiut University Children's Hospital and the head of NICU.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
None.
ACKNOWLEDGEMENTS
The authors would like to thank the NICU administrative staff who facilitated data collection procedures.









