All published articles of this journal are available on ScienceDirect.
Predictive Model for the Quality of Life of Infertile Men
Abstract
Purpose:
This study explores factors influencing the quality of life of infertile men, and attempts to construct a structural model to predict their quality of life.
Methods:
Data was collected via questionnaires from 242 infertile male outpatients from 3 infertile clinics at general hospital urologist departments, with the subjects’ confidentiality was ensured. The self-reported questionnaires were collected for 7 months from February to August 2016 in the outpatient centers. The collected data was analyzed using SPSS/WIN 21.0 Program and Mplus 6.0 Program.
Results:
Hypothesis test of the quality of life as the endogenous variable identified infertility-related stress (β=-0.79, t=-9.41), depression (β=-0.20, t=-2.58), and spirituality (β=0.21, t=2.90) as statistically significant variables. Marital adjustment (β=-0.06, t=-0.69) and social support (β=-0.12, t=-1.79) were not statistically significant. The variables accounted for 84.1% of the variation.
Conclusion:
The results of the study show that infertility-related stress and depression have negative correlation, and spirituality has a positive correlation with infertile men’s quality of life. As such, there needs to be a development of practical and multi-faceted nursing intervention programs to control infertility-related stress and depression levels so as to sustain infertile men’s quality of life.
1. INTRODUCTION
World Health Organization (WHO) reported that about 15% of married couples within the fertility period are infertile couples [1]. The number of infertile men has been increasing by the annual rate of 11.3%, which is more than twice that of infertile women, although the number of infertile women is 4.3 times more than that of infertile men. That is, the number of male patients diagnosed with infertility has recently increased at a rapid rate. Infertile couples are very likely to struggle with a variety of personal and social problems. Stress stemming from infertility might often lead to conflicts with spouses and/or among family members, which could develop to become a social problem such as family destruction [2]. Infertile couples might feel that their lives are ruined and have a hard time getting along with others and at work [3]. Thus, it might be safe to conclude that infertility can exert a negative influence on individuals, families and society. It was reported that infertile couples often expressed negative emotions, including envy and resentment, and that infertility led to physical or mental disorders or diseases in a surprisingly great portion of infertile patients: (78.9%) [4]. It was also reported that 27.7% of the infertile patients diagnosed with other diseases had mental problems, including depression and nervous breakdown [5]. Such negative experiences would play a crucial role in affecting every aspect of their lives as well as daily routines. As time goes by, these infertile men often experience psychological/emotional symptoms such as anxiety, depression, a sense of isolation and guilt after they recognize their infertility [6]. Such stress may be partly attributable to the Korean traditional value system, since marriage is perceived as a process of giving birth and producing the next generations. Becoming a parent is considered a rite of passage to becoming a real adult in society [7]. Failing to become a parent, thus, might be rather perceived as failing to play an important role and being an abnormal being [8].
It was reported in the literature that the longer the period of infertility they had to go through, the more anxiety and tension they had and the less satisfaction they had with their sex life and adaptation to overall marriage life [9].
Development in science and medicine has brought about many changes in the diagnosis and treatment of infertility, which has contributed to the increasing success rate of pregnancy of infertile patients up to 40 to 50% [10]. However, it was also reported that infertile couples often struggle with some difficulties during the period of medical treatments: for example, loss of pride and subjective status, and even confusion of sexual identity due to excessive exposure of their sexual behaviors [11, 12]. Moreover, infertile couples could not but have stress since medical treatments and surgical procedures would not guarantee a pregnancy. As a consequence, during the whole process, they naturally have to struggle with anxiety and concerns, a sense of isolation, helplessness and despair, which might lead to a loss of sense of unity between couples [3]. These negative experiences would, then, result in lowered satisfaction with marriage life, social relationship and, eventually, decreased quality of life [9].
Bae [3] reported that infertile men would feel responsible for infertility, stressed and depressed of seeing their spouses fail to concieve after IVF treatments, being conscious of their spouses and lose activeness. Based on the findings that infertility is responsible for a higher level of stress of male patients, we might assume that infertile men, as well as infertile women, also experience a lowered quality of life. However, a great portion of research on infertile men have focused on medical diagnosis and treatments: for example, genetic factors, causes/diagnosis and oriental medicine for infertility [13]. Also, many researchers have used a fragmental approach to each of the negative side effects such as stress, depression and lowered quality of life [14]. Another reason for the insufficiency of researches on infertile men and lack of base data and intermediation programs would be that infertile men are not willing to share their experiences, and tend to have avoidance and internal concealment [15]. Therefore, it is necessary that we examine the factors influencing the quality of life of infertile men and the relationship between infertility and quality of life in order to identify grounds for intermediation to enhance their quality of life [9].
In this line of thought, adequate programs for nursing intermediation should be developed that could help infertile men overcome their infertility and improve their quality of life by (i) identifying a set of influential factors, and (ii) investigating the relationship between their quality of life and related phenomena such as infertility stress, social support, depression, and spiritual aspects on the basis of many previous types of research including Boivin et al. [14].
Thus, the purpose of the current research is to identify the factors influencing the quality of life of infertile men, to investigate the relationship among the predicted factors and eventually to establish a forecasting model for their quality of life.
2. METHODS
2.1. Study Design
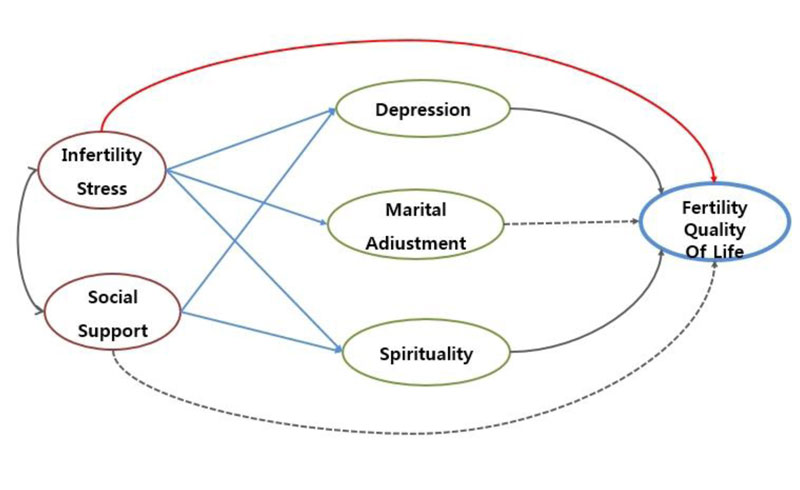
The hypothetical model of the current research is based on the concept of Boivin et al. [14] of infertile men’s quality of life and the literature review of related previous research works. The model consisted of 2 exogenous variables and 4 endogenous variables. The former type of variables are infertility and social support and the latter are depression, marital adaptation, spirituality and quality of life. It was set up in such a way that the two exogenous variables of infertility stress and social support would have a direct effect on their quality of life and that depression, marital adaptation and spirituality would also directly influence their quality of life. Also, it was assumed that the two exogenous variables would exert an indirect effect on their life quality via the parameters of depression, marital adaption and spirituality, as illustrated in Fig. (1). The present research is a test of a structural model to identify the correlation among the influential factors on the quality of life of infertile men.
2.1.1. Setting and Samples
The present research proceeded with convenience sampling of the male patients registered in the urology clinic of the Infertility Center located in S City and G Province. A group of 250 subjects agreed to participate in this research with an understanding of the purpose and meaning of the project. There is no exact criterion for the size of sampling, but the minimal recommendation level is 5 to 10 times of the measurement variables, and at least 200 samples are necessary to verify the structural model based on Maximum Likelihood Estimation (MLE) [16]. Thus, the sample size of the current research subjects, 242, seems suitable since the goodness-of-fit would get worse if the size is too big, say 400 or 500, it would often lead to excessively greater sensitivity.
2.2. Data Collection
The data under analysis was collected at the Infertility Centers of 3 hospitals located in S City and G Province between February and August 2016. Before medical treatments, nurses at the outpatient clinic explained to the subjects how to respond to the questions in the questionnaire. To secure the privacy of the subjects, they were asked to fill up a questionnaire in the consulting room. It normally took 30 to 40 minutes for a patient to finish up answering the questions. Even when one could not complete the questionnaire at the time to see a doctor, he or she returned to the counseling room and filled it up. A total of 242 questionnaires were directly collected in person.
2.3. Ethical Considerations
To protect the subjects’ privacy, the current research began with the approval of the Institutional Review Board of the hospitals: IRB number: GCI-16-02. Also, we received written consent from all the subjects to participate in the research. The consent form included explanations for protection of privacy, anonymity, and their free will to choose to cancel their participation in the research project. Also, in order to avoid information leakage, nurses of the infertility clinic immediately collected the questionnaires right after the subjects’ completion of filling them up. The collected questionnaires were sealed and sent to the researchers, who directly encoded the data into the database. The survey documents and the consent forms were stored in the researcher’s personal cabinet, which was locked and could not be opened by anybody but the researcher. It was stated that those research materials would be destroyed by a paper shredder 3 years after the completion of the research.
2.4. Instruments
2.4.1. Infertility Stress
This study adopted Kim and Shin’s [17, 18] Korean version of the Fertility Problem Inventory (FPI) developed by Newton et al. [17], to measure infertility stress. This tool consisted of a set of 46 items with 5 categories: 10 items for social aspects, 8 on sexual life, 10 on relationships, 8 on refusal of life without children, and 10 items on the necessity for parenthood. The items were measured on a 6 point scale from 1 for ‘strongly agree’ and ‘6 ’for strongly disagree’. A greater score meant a greater level of infertility stress. The reliability of the tool, Cronbach's α, was .93 in the research by Newton et al. [17]. 92 in the research by Kim and Shin [18], and 0.91 in the current research.
2.4.2. Social Support
Social support was measured by adopting Park’s [19] measurement for financial and social support. The tool consisted of a set of 23 items: 9 items for social support, 7 for informative support, 2 for material support and 5 items for appraisal support. The items were measured on a 5 point Likert scale: 1 point for ‘strongly disagree’ and 5 points for ‘strongly agree’. A greater score meant greater social support. Cronbach's α was 0.95 in the research by Park [19] and 0.98 in the present research.
2.4.3. Depression
The measurement of depression was carried out by adopting a version of Beck Depression Inventory (BDI) translated by Lee et al. [20, 21], and developed by Beck [20]. This research tool included emotional, cognitive and physiological aspects to measure the seriousness of one’s depression. It consisted of a total of 21 items measured on a 3 point Likert scale. The greater the score, the greater his or her depression. Cronbach’s α, which indicates the reliability of the tool, was 0.84 in the research by Lee et al. [21], and 0.88 in the present research.
2.4.4. Marital Adaptation
The present research adopted Choi’s [23] Korean version of the Revised Dyadic Adjustment Scale(RDAS) developed by Spanier [22] to measure the marital adaptation of the subjects. RDAS consisted of a set of 14 items with 3 subcategories: 6 items for dyadic consensus, 4 for dyadic satisfaction and 4 for dyadic cohesion. The items were measured on a 6 point Likert scale: 1 point for ‘always in disagreement’ and 6 points for ‘always in agreement’. A greater score meant a greater level of marital adaptation. The reliability of the tool was identified by calculating Cronbach’s α: which was 0.94 in the research by Choi [23] and 0.90 in the present study.
2.4.5. Spirituality
The spirituality of the research subjects was measured by utilizing a version of the Spirituality Assessment Scale (SAS) translated by Oh et al. [24, 25], and developed by Howden [24]. The tool consisted of a total of 28 items belonging to one of the 4 categories: 4 items for ‘meaning and purpose of life’, 9 for a reciprocal relationship, and 6 items for transcendence. The items were measured on a 6 point Likert scale: 6 points for ‘strongly agree’ and 1 point for ‘strongly disagree’. A greater score meant a greater level of spirituality. The subjects’ scores ranged from 28 to 168. A score between 140 to 168 was considered ‘high level of spirituality’, 84 to 112 as ‘moderate’ and 28 to 56 as ‘having spiritual agony’. Cronbach´s α, which signifies the reliability of the measurement tool, was obtainedto be 0.92 in Howden and 0.95 in the current analysis.
2.4.6. Quality Of Life Of Infertile Men
The present research adopted a translated version of a measurement tool for infertile men’s quality of life proposed by Schanz et al. [26]. The tool consisted of a total of 35 items, which belonged to one of the four categories: 7 items for psychological health, 9 for hoping for a baby, 13 for sexual identity and 6 for sexual relationships. Six of the items were written in negative statements and the rest were in affirmative ones. The tool was based on a 5 point Likert scale: 5 points for ‘strongly agree’ and 1 point for ‘strongly disagree’. Thus, the 6 items in negation reverse coded for reverse scoring. A greater score was interpreted as a higher level of life quality. The reliability of the established categories of the tool provided by Schanz et al., varied: Cronbach’s α was 0.84 for psychological health, 0.92 for hoping for a baby, 0.89 for sexual identity and 0.83 for a sexual relationship. The overall internal consistency of the tool was obtained at Cronbach’s α= 0.92 in the present research.
2.4.7. Data Analysis
The collected data was analyzed by utilizing the statistical programs of SPSS/WIN 21.0 and Mplus 6.0. A descriptive analysis was conducted to identify the general characteristics of the subjects, frequency, percentage, means, and standard deviation of related variables. The correlation among the variables under measurement was analyzed by adopting Pearson correlation coefficient. Multiple regression was performed to analyze the influential factors for quality of life. The Cronbach’s α value was calculated to examine the reliability of the measurement tools and a confirmatory factor analysis tested the validity of the tools. The normality of the samples was identified by multivariate normality analysis using Mplus 6.0 program: the mean, standard deviation, skewness, and kurtosis were identified. To analyze the structural equation, the measurement model was estimated and then the structural model.
The verification of goodness of the model was evaluated by using χ2 the index of absolute fitness of RMSEA, the index of relative fitness of CFI, TLI, and the standardized residual average square root of SRMR. Mplus 6.0 program was utilized to identify the statistical significance of the indirect effect and the overall effect of the current research model.
3. RESULTS
General characteristics and infertility-related characteristics of the subjects as for the age of subjects, 62.4% of them were younger and 37.6% were older than 35. In terms of education, a great portion, 92.1%, of the subjects had at least a bachelor’s degree. Also, more than half of them, 57.4%, reported that they had no religion. 90.1% of the subjects lived in the form of a nuclear family. Considering the period of marriage, 47.1% of them had been married for more than 1 year and less than 3 years, 24.4% for 3 to 5 years and 22.3% for less than a year. 42.6% of them lived with a monthly income of more than 500 million won. 48.8% were nonsmokers. 41.3% of them mentioned that they drink once or twice per week. 61.6% answered that they were not participating in any physical workout. 80.2% of them said that they would stay at work for 9 to 12 hours per day. Finally, 67.4% of them had been diagnosed with infertility less than a year (Table 1).
The subjects’ infertility stress, social support, depression, marital adaptation, spirituality and quality of life.
The mean and standard deviation for each factor was obtained at 99.57±19.13 for infertility stress, 4.07±0.65 for social support, 4.07±0.65 for depression, 4.47±2.56 for marital adjustment, 4.84±0.59 for spirituality 110.40±20.69 for quality of life 4.10±0.51, respectively. The skewness for all the factors under analysis was less than ±2 and the kurtosis was less than ± 4, which satisfied the basic criteria for verification of normality of the samples used in the present research (Table 2).
| Variables | Categories | n(%) or Mean±SD |
|---|---|---|
| Age(yr) | <35 | 151(62.4) |
| ≥35 | 91(37.6) | |
| Education | High school | 19(7.90) |
| ≥University | 223(92.1) | |
| Religion | No | 139(57.4) |
| Yes | 103(42.6) | |
| Family type | Nuclear family | 218(90.1) |
| Co-residence family | 12(5.0) | |
| Etc | 12(5.0) | |
| Marital period (year) | <1 | 36(14.9) |
| <1~3 | 114(47.1) | |
| <3~5 | 59(24.4) | |
| ≥5 | 33(13.6) | |
| Family monthly income (unit 10,000 won) | <300 | 36(14.9) |
| <300~500 | 103(42.6) | |
| ≥500 | 103(42.6) | |
| Smoking | No | 118(48.8) |
| Smoking | 78(32.2) | |
| Quit | 46(19.0) | |
| Drinking | No | 46(19.0) |
| 2~3(month) | 73(30.2) | |
| - | 1~2(week) | 100(41.3) |
| - | 3~4(week) | 22(9.1) |
| - | Everyday | 1(0.4) |
| Exercise | No | 149(61.6) |
| Yes | 93(38.4) | |
| Working time(hours/day) | <8 | 33(13.6) |
| - | <9~12 | 194(80.2) |
| - | ≥13 | 15(6.2) |
| Infertility treatment period (year) | <1 | 163(67.4) |
| - | <2~3 | 61(25.2) |
| - | ≥4 | 18(7.4) |
| Variables | Range | Mean±SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Infertility related stress | 58~153 | 99.57±19.13 | .12 | -.54 |
| Social support | 1~5 | 4.07±0.65 | -.68 | 1.34 |
| Depression | 0~30 | 4.47±2.56 | 1.85 | 5.56 |
| Marital adjustment | 3~6 | 4.84±0.59 | -.37 | -.11 |
| Spirituality | 28~165 | 110.40±20.69 | -.14 | .41 |
| Quality of life | 3~5 | 4.10±0.51 | -.37 | .64 |
| Model | χ2 | χ2/ df | SRMR | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| Modified model | 325.314(p<.001) | 2.37 | .054 | 0.934 | 0.917 | 0.075 |
3.1. Verification of The Structural Model
The present research set up a structural model on the basis of a set of previous studies and the theory of quality of life of Boivin et al. [14]. The evaluation of the hypothetical model was conducted to examine whether its overall structure can yield an appropriate explanation. The goodness of fit index was calculated for that purpose. The structural equation model analysis confirmed the chi-square test and fit index for exploring the path through which each latent variable affected the quality of life and identifying the proposed hypothetical model fit to the sample data. The absolute fit indices and the incremental fit indices evaluating the overall goodness of fit of the model were as follows: χ2 /df = 2.37, CFI=.0.93, TLI =0.91, RMSEA=0.07 Thus, the study model reflected well for the model (Table 3).
| Endogenous variables | Exogenous variables | Direct effect ß (p) |
Indirect effect ß (p) |
Total effect ß (p) |
|---|---|---|---|---|
| Quality of life | - | - | - | - |
| - | Infertility related stress | -0.79(p<.001) | -0.09(.183) | -0.88(p<.001) |
| Infertility related stress-> Depression | -0.42(p<.001) | -0.08(.006) | - | |
| Infertility related stress->Marital adjustment |
-0.55(p<.001) | 0.04(.413) | - | |
| Infertility related stress-> Spirituality | 0.20(.021) | -0.04(.243) | - | |
| Quality of life | - | - | - | - |
| - | Social support | -0.12(.142) | 0.13(.005) | 0.01(.142) |
| Social support-> Depression | -0.20(.013) | 0.04(.422) | - | |
| Social support-> Marital adjustment | 0.19(.034) | -0.01(.342) | - | |
| Social support-> Spirituality | 0.50(p<.001) | 0.10(.012) | - | |
3.2. Direct, Indirect, and Total Effects of Variables
The path coefficient of the final model was evaluated by estimates of the magnitude of the parameter and its significance. There were significant direct (γ=-0.79, p<.001) and total effects (γ=-0.88, p<.001) between the quality of life and infertility-related stress. Infertility related stress was directly associated with depression (γ=0.42, p<.001), marital adjustment (γ=-0.55, p<.001) and spirituality (γ=0.20, p=.021). In addition, social support was directly associated with depression (γ=-0.20, p=.013), marital adjustment (γ=0.19, p=.034) and spirituality(γ=0.50, p<.001) (Table 4).
4. DISCUSSION
It was found that the factor of infertility stress marked the score of 3.10, which was lower than 3.24 in Kim and Shin’s [18] similar research on infertile women. Therefore, it might be safe to assume that this research supports the conclusion that infertile women had a greater level of depression and stress than their spouses (infertile men) [27]. The rank of the sub factors in their influence on the quality of life of infertile men was identified in the order of parental needs, social area, relationship area, refusal of children and sex area, which supported the results of Kim and Shin [18]. This perhaps indicates that the culture of patriarchy still remains in current society. It was found that infertility stress on infertile men varied depending on the subjects’ religion, the period of infertility treatment, family relationship, personal health and occupation. This result is consistent with the finding of Min et al. [28], stating that infertility stress varies with the general characteristics of the subjects. In particular, the subjects following a religion were found to be less stressfull than those not following a religion. Thus, religion obviously plays a mediator role in reducing infertility stress. Also, it was found that the subjects staying longer than 13 hours at work showed a greater level of stress than those staying less at work. An average Korean stays at work for 2014 hours per year, which is 294 hours longer than the average 1730 hours of OECD countries [29]. Longer hours at work, which might aggravate infertility stress, would affect the success rate of pregnancy. A variety of efforts to reduce stress at work places, thus, are called for as an effective strategy of solving the serious problem of low birth rate, since infertility stress would lead to a low level of success rate of pregnancy [4.5].
It was also found that the absence of supporters was closely related to a greater level of infertility stress, which is consistent with the result of Mikkelsen et al. [30]. It is clear that infertile men also needed support similar to infertile women. It is necessary that a standardized guideline be developed and promoted to manage infertility stress of infertile men. Also, infertile men usually do not want to let their infertility known to others except their spouses. Moreover, they would try to obtain support from medical personnel. Thus, a support program at the clinic should be operated.
This research found that infertile men living in an extended family would get more social support. An extended family often would not secure the privacy of a married couple. However, the family structure, on the other hand, would provide social support for infertile men [4, 5]. The nuclear family would not play such a role in providing support. Therefore, efforts at the society level are necessary: for example, the establishment of the appropriate social environment and care centers for infertility. To take an example overseas, Japan operates infertility counseling centers and Australia puts comprehensive nursing care into practice for infertility patients [5]. Such efforts would play an important role in solving the national issue of low birthrate. A high level of social support would at least lead to opening up of those patients. A significant difference was also found in social support between those with medical treatments experience in the past and those presently under treatment. This difference might be explained by assuming that the subjects also received support while receiving medical treatments.
Depression also had a significant effect on the quality of life of the subjects, which agreed with the findings of the researches on infertile women and infertile couples [31, 32]. It was reported that the degree of depression of infertile women was similar to that of patients with heart diseases or high blood pressure [2]. However, the depression level of infertile men under analysis was relatively lower compared to that of infertile women, though it still had an influence on their quality of life. This low level of depression is consistent with the finding of the past research on those who had failed to have a baby after IVF (In Vitro Fertilization) treatment. It might be assumed that men would be more likely to better control their emotions and conceal feelings.
It was also found that there was a significant correlation between depression and smoking, which seems consistent with Bae’s report that infertile men would try to get rid of depression by drinking [33]. An intermediation program for infertile men, thus, should design an effective and desirable way to help them control their drinking and smoking habits to manage depression.
The present study found that marital adaptation, though influenced by infertility stress, did not exert a direct effect on the life quality of infertile men. Such a result is similar to the findings of past researches. In contrast to infertile women, infertile men did not show a significant effect of marital adaption on their quality of life [3]. Kim and Shin [18], however, reported that marital adaptation influenced infertile women’s quality of life. Such a difference between men and women might be attributable to their different periods of medical treatments. In Kim and Shin’s [18] research, 11.8% of the subjects had been under medical treatments for less than a year, while 67.4% of the subjects in the current study had been treated for less than a year. It can be assumed that such a short period of treatments would not have affected their marital adaptation. Marital adaptation is a correlational factor [34], and, thus, would not exert a direct impact on the quality of life of infertile men. It was also found that marital adaptation was higher in the subjects aged 35 or older, which is similar to the finding that the younger the subjects, the lesser their marital adaptation [35]. Also, those with the experience of infertility treatments showed a greater level of marital adaptation than those without such an experience. Such a finding is different from the finding of Ragni et al. [36]. It might be assumed that a long period of medical treatments to escape from the difficulty of infertility would strengthen the unity of a married couple. In contrast, some researchers reported that the period of medical treatments would often lead to marital conflicts [3]. Further detailed research works are called for in order to identify the relationship between medical treatments for infertility and marital adaptation.
As mentioned above, marital adaptation was found not to affect the life quality of infertile men, perhaps because their period of medical treatments was mostly less than a year. Such absence of influence might result from the fact that the measurement tool for marital adaptation did not include communication, reciprocal relationship, and/or conflicts between infertile men and women, and hence failing to appropriately reflect their quality of life. Thus, it might be suggested that further research should use a tool containing such factors such as marital communication, conflicts, infinity and relationship. Bae [3] reported that infertile men would feel responsible for infertility, get stressed and depressed of seeing their spouses fail to get pregnant after IVF treatments, conscious of their spouses and lose activeness. It seems essential that structured intermediation programs should get infertile couples involved in order to enhance their marital adaptation and communication.
The current research found that spirituality was an influential factor in the quality of life of infertile men. A higher score was recorded from those who had been married for more than 5 years, who had received medical treatments for infertility, and whose wives were in the process of gathering ova. Such a result seems similar to the finding that middle-aged women possessed a higher level of intrinsic sources of spirituality [37, 38]. Thus, it seems that gender difference would not result in a significant difference in the effect of spirituality, but further research should investigate the relationship between gender, age and period of infertility on one hand and spirituality and quality of life of infertile men on the other. The presence of people who provide support was closely related to a higher score of quality of life, which might mean that a low level of stress would lead to a higher level of life quality. This result is consistent with the finding of past research works that infertility stress would cause conflicts, loss of control, depression and a low level of quality of life [8, 11, 15]. That is, the infertility stress of infertile men should come from getting rid of the pressure of parenthood, which can not be obtained by themselves. Also, treatments should be carefully carried out not to give displeasure or humiliation to infertile men, but to help enhance their self-esteem.
It was found, as expected, that the subjects of infertile men had a high level of financial burden. Each surgical procedure for infertile women cost an average of 4.45 million Won and 60.9% of them had to pay an additional 0.3 to 2 million Won. It was reported that a great portion of the subjects were under financial burden: 71.3% answered ‘very serious’ and 26.5% answered ‘serious’. Thus, in arranging strategies to solve the serious problem of low birthrate, government should take measures to alleviate their financial burden by providing subsidies and providing medical insurance cover the medical and surgical treatments for infertile men. In Korean culture, men are mainly responsible for the household economy, which aggravates the seriousness of the financial burden. Thus, a strategic plan to secure infertile men’s rights in their treatments and surgeries should be developed at a national level. 94.4% of the subjects showed their expectation to be successful in pregnancy after medical treatments. Medical personnel have to treat them with a high level of consideration and affection. Previous research works reported that infertile men wanted to obtain more information about infertility from medical personnel [33]. As lack of sufficient information might lead to infertility stress, which could eventually lower the quality of life, it seems that a standardized guideline should be prepared to provide infertility-related information. Also, experts in infertility should be trained in order to offer appropriate counseling at the clinic. Self-help groups in on- and off-line spaces can also help infertile men overcome infertility stress.
CONCLUSION
The structural model used in the current research on the quality of life of infertile men can be characterized by the following points. First of all, it is an integrative model combining personal, relational and social factors for forecasting the subjects’ quality of life. It was found that infertility stress exerted a greater impact on their quality of life than any other factors, and that depression had an indirect effect. It suggests that infertile men tend to hide their emotions and not to express them out. It might be assumed that they would consider infertility as their own problem instead of complaining about the difficult situation to others. Thus, it seems necessary that self-help groups be used more actively in order to enhance their quality of life by sharing their infertility stress and enabling them to vocalize their depression.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Gangnam CHA hospital, South Korea with approval number GCI-16-02.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This research is funded by the Namseoul university research fund.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
This manuscript is based on a part of the first author's doctoral dissertation and this research is funded by the Namseoul university research fund.


