All published articles of this journal are available on ScienceDirect.
Prescription of Antimicrobials in Primary Health Care: Scoping Review
Abstract
Objective:
To map the available evidence about the prescription of antimicrobials in Primary Health Care.
Methods:
A Scoping Review has been proposed based on the procedures recommended by the Joanna Briggs Institute.
Results:
This review included a total of 16 studies. The articles compiled demonstrated that this theme is the center of discussion, in a linear manner, over the past 12 years. Among the studies, 37.5% occurred in Brazil, and regarding the prescription of antimicrobials analyzed in studies, amoxicillin was the most prescribed, the physician was the prescribing professional in 12 studies, and the prescriptions were mostly intended for the general population (children, adolescents, adults and the elderly).
Conclusion:
This review ratifies the premise of rational use of antimicrobials promoted by the World Health Organization through the goals of sustainable development when understanding that these drugs have been considerably prescribed in the daily routine of Primary Health Care and there is no specific system to control and monitor their rational use.
1. INTRODUCTION
The antimicrobials are drugs used to treat a microbial infection, inhibiting the growth and/or destroying microorganisms, covering medicines that treat infections caused by bacteria and other microbes such as parasites, viruses and fungi. Among the antimicrobial drugs, antibiotics are one of the pillars in the treatment of an infection; however, their unnecessary or inappropriate use contributes substantially to the Antimicrobial Resistance (AMR) [1].
The AMR is a worldwide concern because it is a threat to human health, and, although it is an evolutionary phenomenon, reducing the inappropriate use of antibiotics would broaden their effectiveness and mitigate clinical, human and economic costs of drug-resistant infections. The estimated world’s annual mortality related to drug-resistant infections will be 10 million people by 2052 [2].
Worldwide, there was an increase of 65% in the consumption of antibiotics from 2000 to 2015 and double in low- and middle-income countries [3]. The increased consumption may be related to several factors, including the inadequate practice of antibiotic prescription [4] that directly affects the AMR and reduces the effectiveness of those drugs [5].
The inappropriate prescription of antibiotics is common in all countries, particularly in the centers of Primary Health Care (PHC) [6]. In a hospital environment, there is greater control of these requirements, contrary to what occurs in the PHC, particularly in the middle- and low-income countries [7].
PHC was not always the focus of AMR-fighting strategies, which concentrated on tertiary care institutions. However, currently, the literature indicates the need to evaluate the use of antibiotics at the primary level because some developing countries have health facilities that lack adequate access to the infrastructure of water, sanitation, hygiene and waste management, which cause the spread of antibiotic-resistant infections [8]. In addition, professionals with little or no training regarding the prescription of antibiotics [9,10], late or no diagnosis of infections, affect the prescription for infectious diseases that are not caused by bacteria, leading to the shortage of medicines [11].
Although it is a routine activity, the prescription of antimicrobial agents is a complex process associated with intrinsic (attitude, knowledge, individual characteristics) and external factors (institutions, health systems, patient, environment). The quality of the prescription of medications, along with the pharmaceutical assistance, serve as indicators used for the evaluation of services, because it allows comparing the level of problem-solving ability of actions undertaken and the conditions of services provided [12].
The control of AMR is a challenge for health systems in the world because it threatens the global efforts to reach the Sustainable Development Goals (SDG), in particular, the SDG 3, which aims “to ensure a healthy life and promote the well-being for all, in all ages” and, until 2030, foresees an increase in the pace of progress in the fight against the growth of AMR. Thus, the monitoring of the use of those drugs, the investigation of factors that favor the inappropriate use and the creation of interventions for the control are recognized as indispensable strategies for slowing the progression of this problem. Furthermore, the present study aims to map the available evidence about the prescription of antimicrobials in Primary Health Care.
2. MATERIALS AND METHODS
2.1. Design
This is a scoping review based on the procedures recommended by the Joanna Briggs Institute (JBI) [13]. To formulate the research question, the Population, Concept and Context (PCC) strategy was used, where “P” refers to the population/participants, “C” to the concept one proposes to investigate and “C” to the context. Therefore, this review considered the studies performed with the Population (Health Professionals), Concept (Prescription of antimicrobial agents) and Context (Primary Health Care). Based on these definitions, the following guiding question was established: What is the scientific evidence regarding the prescription of antimicrobials in Primary Health Care?
2.2. Data Collection
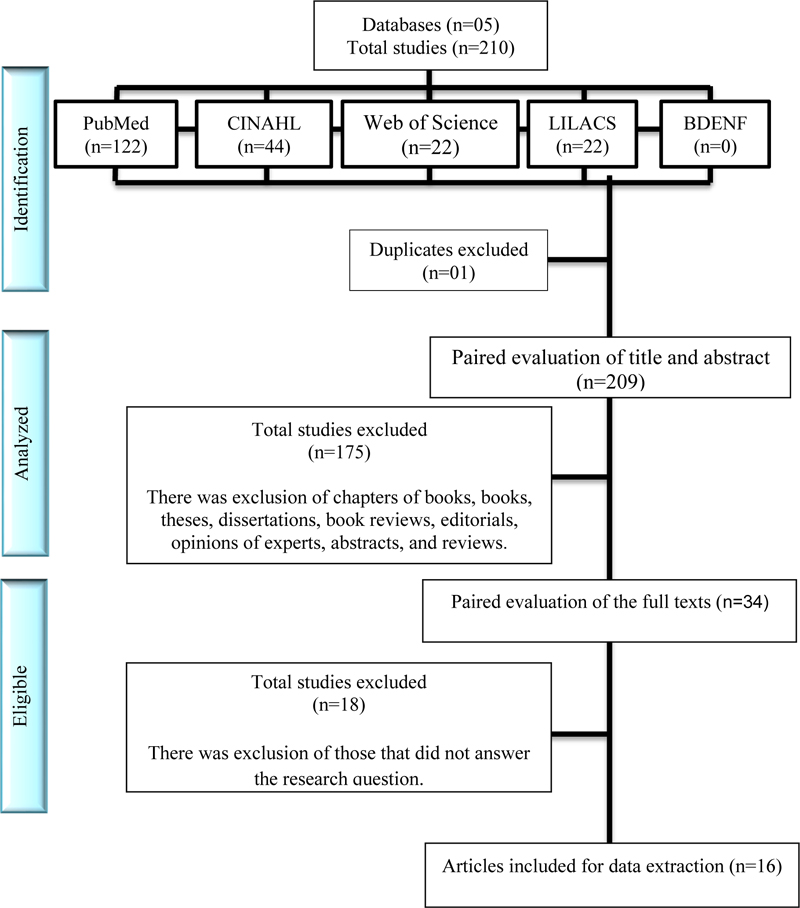
Data collection was carried out systematically on the databases PubMed, CINAHL, Web of Science, BDENF and LILACS. The sample included studies with the specific object regarding the prescription of antimicrobials in the PHC, with empirical results without limits of year or language, in order to research on the ‘Use of Antimicrobials in Primary Health Care’. The exclusion criteria were chapters of books, books, theses, dissertations, book reviews, editorials, opinions of experts, abstracts, reviews and researches that were not related to the primary object of this study.
The search strategy was constructed to meet the requirements of each database, i.e., the Health Sciences Descriptors (DeCS) were used for the database Lilacs and BDENF, and Mesh Descriptors to search on the other databases. The search strategy was constructed and may be reproduced according to the Chart 1 below.
Data collection was carried out on December 29, 2019, being held by two reviewers independently to ensure the rigor in the process of selection of articles, and, in case of doubts, a third party was responsible for the decision to include or not. The first step was the exclusion of texts through the reading of the title. Next, the abstracts of the texts included in the first screening were read. All texts selected after reading the abstracts were fully read and had their data extracted independently by at least two of the authors, and then, organized jointly. The parameters for the acquisition of the data extracted were author, year, country of study, design, most prescribed antimicrobial, prescriber and population.
2.3. Data Analysis
The information compiled from the articles was analyzed descriptively and presented in the form of tables and charts with the characteristics relevant to the main findings in studies related to the theme.
Since this study did not involve humans, it did not require submission to the Research Ethics Committee. Moreover, for a scoping review, there is no need to evaluate the methodological quality of the studies included. The present study followed the Standards for Quality Improvement Reporting Excellence 2.0 (SQUIRE 2.0), and was reviewed according to the checklist of items of systematic review - Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
3. RESULTS
The search performed on different databases returned 210 studies. After excluding duplicate citations, the titles and abstracts of 209 documents were read to verify compliance with the inclusion criteria. Of these, 175 were excluded because they were chapters of books, editorials or reviews. Of the 34 texts fully read, 18 were excluded because they did not respond to the research question, resulting in 16 studies to be included in this review. The process of selection of documents is presented in the PRISMA flowchart, as shown in Fig. (1):
| PubMed | (((((“Anti-Infective Agents”[Mesh] OR Anti-Infective Agents[Text Word]) OR “Anti-Bacterial Agents”[Mesh]) OR Anti-Bacterial Agents[Text Word]) AND (((“Prescription Drugs”[Mesh] OR “Medication Systems”[Mesh]) OR Prescription Drugs[Text Word]) OR Medication Systems[Text Word])) AND (((“Primary health care”[Mesh] OR “Pharmaceutical Services”[Mesh]) OR Primary Health Care[Text Word]) OR Pharmaceutical Services[Text Word])) NOT “hospitals”[MeSH Terms]) |
| CINAHL | (((MH “Antiinfective Agents”) OR “Anti-Infective Agents”) AND ((MH “Drugs, Prescription”) OR (MH “Medication Systems”) OR (MH “Medication Systems”) OR “Medication Systems”) AND ((MH “Drugs, Prescription”) OR “Primary health care” OR “Pharmaceutical Services”)) NOT (MH “Hospitals”) |
| Web of Science | “Anti-Infective Agents” OR “Antimicrobial Action” OR “Anti-Infective Drugs” OR “Antimicrobial Agents” OR Antimicrobials AND “Prescription Drugs” OR “Medication Systems” OR “Prescription medication” OR Prescription OR “Prescription Drugs” AND “Primary Health Care” OR “Pharmaceutical Services” OR “Basic Attention” |
| LILACS | (tw:((tw:((tw:(“Anti-Infective Agents”)) OR (tw:(“Antimicrobial Action”)) OR (tw:(“Anti-Infective Drugs”)) OR (tw:(“Antimicrobial Agents”)) OR (tw:(Antimicrobials)))) AND (tw:((tw:(“Prescription Drugs”)) OR (tw:(“Medication Systems”)) OR (tw:(“Prescription medication”)) OR (tw:(Prescription)))) AND (tw:((tw:(“Primary Health Care”)) OR (tw:(“Pharmaceutical Services”)) OR (tw:(“Basic Attention”)))))) AND NOT (tw:((mh:(Hospitales)) OR (mh:(Hospitais)))) |
| BDENF | (tw:((tw:((tw:(“Anti-Infective Agents”)) OR (tw:(“Antimicrobial Action”)) OR (tw:(“Anti-Infective Drugs”)) OR (tw:(“Antimicrobial Agents”)) OR (tw:(Antimicrobials)))) AND (tw:((tw:(“Prescription Drugs”)) OR (tw:(“Medication Systems”)) OR (tw:(“Prescription medication”)) OR (tw:(Prescription)))) AND (tw:((tw:(“Primary Health Care”)) OR (tw:(“Pharmaceutical Services”)) OR (tw:(“Basic Attention”)))))) AND NOT (tw:((mh:(Hospitales)) OR (mh:(Hospitais)))) |
Source: The authors (2020).
The studies recovered in this review covered the years 2007 to 2019, presenting linearity over this period. Only the year 2013, according to the searches, had no publications recovered on the topic. The cross-sectional studies were the most used, accounting to87.5%, according to Table 1.
In relation to the characterization of the studies according to the location (country) of development of research, the antimicrobials most prescribed, the prescriber and the target population of the prescribed antimicrobials, 37.5% of the studies occurred in Brazil, followed by Africa with 18.75% and the other countries Japan, New Zealand, Poland, Sri Lanka, Palestine, Canada and the Czech Republic, with 6.25% each. The most prescribed antimicrobial was amoxicillin with a rate of 68.75%, and, within the studies analyzed, its prescription ranged from 6.8 to 49.7%. Regarding the prescriber, 13 studies contained this information, and, in eight of them, the doctor was the only prescribing professional. Notably, in only three studies, the nurse was the prescriber. Concerning the use of antimicrobials by the studies, they were mostly intended for the general population (children, adolescents, adults and the elderly), according to Chart 2.
4. DISCUSSION
The scientific evidence regarding the prescription of antimicrobials in PHC demonstrates that this theme has been the center of discussion over the past 12 years in a linear form, which is justified by the problem of AMR that has been discussed since the beginning of the use of antibiotics. The growth of this resistance corroborates the global efforts of SDG because the impact of AMR in the increased hospital admissions, length of hospital stay, in deaths and costs to health systems hinders the promotion of health and well-being for all, at all ages.
| Variables | N | % |
|---|---|---|
| Year of Publication | ||
| 2019 | 1 | 6.25 |
| 2018 | 2 | 12.5 |
| 2017 | 1 | 6.25 |
| 2016 | 1 | 6.25 |
| 2015 | 1 | 6.25 |
| 2014 | 1 | 6.25 |
| 2012 | 2 | 12.5 |
| 2011 | 1 | 6.25 |
| 2010 | 1 | 6.25 |
| 2009 | 1 | 6.25 |
| 2008 | 3 | 18.75 |
| 2007 | 1 | 6.25 |
| Type of study | ||
| Cross-sectional | 14 | 87.5 |
| Cohort | 1 | 6.25 |
| Longitudinal | 1 | 6.25 |
Source: Research on databases.
| Author (year) | Place (country) | Most prescribed antimicrobial | Prescriber | Population |
|---|---|---|---|---|
| Uda, Okubo, Kinoshita, Morisaki, Kasai, Horikoshi and Miyairi (2019) | Japan | 3rd generation cephalosporin (50.1%) | - | Children |
| Tomlin, Woods, Lloyd and Tilyard (2018) | New Zealand | Amoxicillin (42%) | - | Children and adolescents |
| Bilal, Osman and Mulugeta (2018) | East Africa | Amoxicillin (33.3%) | - | General |
| Mitre, Silva, Silva, Rezende and Sousa Jr (2017) | Brazil | Penicillin (52.3%) | Physicians | General |
| Ahiabu, Tersbøl, Biritwum, Bygbjerg and Magnussen (2016) | Amoxicillin (26.7%) | Physicians and medical assistants | General | |
| Adisa, Fakeye and Aindero (2015) | Western Africa | Amoxicillin (25.4%) | Community extension workers, nurses, community health workers, pharmacy technicians and physicians | Adolescents, adults and the elderly |
| Chlabicz, Chlabicz, Marcinowic, Rogowska-Szadkowska, Pytel-Krolczuk and Leszczyńska (2014) | Western Africa | Amoxicillin (28%) | Physicians | Adults |
| Oliveira, Xavier and Araújo (2012) | Poland | Metronidazole (9.5%) | Physicians and Nurses | General |
| Pajarín Fernández, Peacok Aldana, Granados Hormigó and Álvarez González (2012) | Brazil | Quinolones (56.7%) | Physicians | The elderly |
| Obreli Neto, Vieira and Cuman (2011) | Cuba | Amoxicillin (6.8%) | Physicians | General |
| Sawalha, Sweileh, Zyoud, Al-Jabi, Shamseh and Odah (2010) | Brazil | Amoxicillin (39%) | Physician | General |
| Murphy, Martin-Misener, Cooke and Sketris (2009) | Palestine | Amoxicillin (34%) | Nurse | The elderly |
| Jindrak, Marek, Vanis, Urbaskova, Vlcek, Janiga, Maresova (2008) | Canada | Macrolides | Physicians | Children |
| Tavares, Bertoldi and Muccillo-Baisch (2008) | Czech republic | Amoxicillin (48.7%) | Physicians | Adults and the elderly |
| Abrantes, Magalhães, Acúrcio and Sakurai (2008) | Brazil | Amoxicillin (47%) | Physicians | Children and adults |
| Abrantes, Magalhães, Acúrcio and Sakurai (2007) | Brazil | Amoxicillin (49.7%) | Physicians and dental surgeons | General |
Most of the studies have been obtained from the developing countries, which affects the use of antimicrobials, because the patterns of microbial resistance are uneven among countries and within a same country, depending on the most prevalent infectious diseases in each location and the use of antimicrobials for the control of such diseases. Unfortunately, patients who are treated with an antimicrobial drug may acquire resistance not only to a drug, but to several others, depending on various situations that may be linked to the prescriber, the prescription, the patient and the environment.
A greater control of the prescription of those drugs in the hospital environment, regardless of the community context, is a consensus in the literature. Therefore, the PHC constitutes a possibility for monitoring and control of this prescription, promoting the rational use at the primary care level to try to halt the progression of the AMR and prevent the patient from arriving at the tertiary level without chances to fight the infection by multidrug-resistant bacteria.
Analyzing the years of recovery, according to the searches, the first article used an evaluation instrument of the World Health Organization (WHO) [14], which is still mentioned, even with 14 years between its publication and its use in the study (1993-2007) [15]. Even before the promotion of rational use of medicines, WHO, in 1993, developed indicators to assess the use of medications in outpatient health facilities. The indicators are grouped into three categories, namely: prescribing indicators, percentage of drugs found with a prescribed injection, percentage of drugs prescribed by generic name and percentage of drugs prescribed from the essential drugs list.
The reason for the aforementioned period may be the fact that the document published by the WHO was not in the Portuguese language, the first language of the first publication recovered in this review. Nevertheless, the article developed in Southeastern Brazil [15] that evaluated the prescription of antimicrobials in Basic Health Units (BHU) used those indicators, which are still used nowadays [16-19].
In relation to the type of study, the cross-sectional design is more appropriate when the goal is to identify the situation, at any given time, of the prescription of antimicrobials in PHC or perform an audit in order to check the progress of interventions to the problem of AMR in the location studied. Nonetheless, among the limitations pointed out by the authors in relation to this experiment is the difficult monitoring of the whole situation, which involves the prescription (patient, prescriber and environment), since some studies evaluate the prescribing indicators [16-19], others evaluate the prescription characteristics [20] (adequate or inadequate) regarding the items a prescription must contain, and some others verify the adequacy of the antimicrobials prescribed for certain infection [21]; however, the complexity of the prescription for the development of AMR involves all those investigations at the same time and analyses of knowledge of prescribers and patients, analyses of the environment of the health facility (availability of water, sanitation and waste management) and socioeconomic factors.
In relation to the characterization of the studies, the majority occurred in Brazil [15,19,20, 22-24], with prescriptions made by the medical professional for the general population (children, adolescents, adults and the elderly) [15-16, 18-19, 22-23, 25], mostly prescribing Amoxicillin.
The researches carried out in Brazil may be justified by some points, such as being classified by IMS Health (Intercontinental Marketing Services Health) as one of the nations, which, together with the other twenty in the world list, represents two-thirds of global pharmaceutical growth between 2012 and 2017. With that, the antimicrobials fulfill a wide space in this percentage, representing one of the drugs most used in the country [26], with a universal and free coverage from pharmaceutical care at the PHC level, through the Unified Health System [15, 22-23]; and being a developing country.
The physician [15, 17-25, 27-28] is recognized, in all countries, as a skilled professional to prescribe all classes of medications, which justifies the largest contingent of the analyzed prescriptions. Depending on the country, the rules for the prescribing professional change, such as in a study conducted in West Africa [29], where, in addition to physicians, the so-called ‘community health extension workers’ were also authorized to prescribe medications, who are community health agents with practical training for the community based on the health system adopted, which features four care levels and the BHU is the most basic level.
Another example is Brazil [19], where nurses can prescribe medicines according to the public health programs and routines previously approved in public or private health institutions. It should be emphasized that, according to the International Council of Nurses (ICN) [30], nurses can prescribe drugs in four different ways: independent, autonomous or substitute; dependent, collaborator, semi-autonomous, complementary or supplementary; the protocol group and the prescription changing schedule and dosage. The United States, the United Kingdom, Australia and New Zealand are part of the protocol group, which follows a specific written standard for the management of certain drugs in a given clinical situation. In Canada, the nurse’s prescriptive practice is more consolidated [31].
Concerning the antimicrobials prescribed in the PHC, the amoxicillin is a representative of penicillin, betalactam antibiotics, acting as bactericides against gram-positive and gram-negative microorganisms. Due to this, it is indicated for upper respiratory and urinary tract infections, clinical conditions whose symptoms are commonly confused with simple diseases, in addition to the extended spectrum, oral administration and good tolerability of the drug [22].
The antimicrobials are the drugs most often prescribed and used incorrectly, and are considered one of the most notable medications that influence not only the patient under treatment, but the whole ecosystem surrounding him/her; and this explains the fact of great concern regarding the distribution and dispensing of antimicrobials, with massive investment in studies and researches not only at secondary and tertiary level, but also at primary level.
Regarding the patients to whom the prescription is intended, the major concern is the age. In relation to children, the prescription of antimicrobial agents is associated with upper airway infections, representing 43% of the prescriptions; however, there are discussions regarding a specific diagnosis in PHC, since a large part of those infections is viral [20, 28, 32]. As for the elderly [21, 31], the justifications include recurrent infections, typical factors of the age, associated comorbidities and difficulties presented by prescribers in relation to the therapeutic scheme (high doses, irregular frequencies and treatment length).
Concerning the analysis of prescriptions, the studies used audits in their own healthcare establishments [16, 18-19, 22-23, 25, 31], guides of interviews [17, 28], tests of knowledge [21]; and three used data from electronic information system [27, 32-33]. The scientific productions analyzed converge in relation to the growth of antimicrobial prescriptions worldwide and the impact of resistance to such drugs for public health as a waste of resources and risks to health in general. Nonetheless, in a study published in 2011, there has been a small reduction in the prescription of antibiotics, even if incipient, demonstrating that the campaigns of the rational use of antimicrobials are beginning to give signs of improvement.
In relation to the studies that use an electronic database, an automated system of encoded data enables automation and repetition of analyses of prescriptions of antimicrobials in any follow-up time, thus being able to monitor regularly the use of drugs in order to verify the effects of interventionist strategies on the rational use of drugs and identify potential problems.
The importance of this class of drugs in the context is notorious [34-36]. The evidence presented here contributes to the identification of the usage profile of those drugs in the world, per region, and is the beginning to draw appropriate interventions for the health system used in each country.
CONCLUSION
Undoubtedly, the pharmacological treatment for infections is a valuable ally in healing. However, the microbial resistance hinders the therapeutic progression. The results found in the present study corroborate the premise of rational use of antimicrobials fostered by WHO through the SDG, indicating that those drugs are being prescribed in a considerable way in the daily routine of PHC and do not have a specific system to control and monitor their rational use.
The power of resistance to those drugs is growing continuously, while strategies to promote their rational use are lagging behind, because as can be seen, there is no specific control system covering the entire cycle of pharmaceutical care.
Therefore, the studies recommend some interventions, a system designed to assess the quality of the prescription of antimicrobials using prescription data related to the diagnosis; public campaigns in favor of rational use of antimicrobials; Patient-based interventions; Restriction Policies; continuing education of professional prescribers; Multi-faceted interventions; guidelines about the management of the drug for users and commitment of the health system to promote and subsidize those interventions.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Not applicable.


