All published articles of this journal are available on ScienceDirect.
Night-time Noise Levels and Patients’ Sleep Experiences in a Medical Assessment Unit in Northern England
Abstract
Background:
Hospital in-patients need sleep so that restorative process and healing can take place. However, over one third of in-patients experience sleep disturbance, often caused by noise. This can compromise patients’ perceptions of care quality and cause physical and psychological ill health.
Aims:
To assess 1) in-patients sleep quality, quantity, reported sources of sleep disturbance and their suggestions for improvement 2) objectively measure decibel levels recorded at night.
Methods:
This descriptive study conducted in a Medical Assessment Unit used multi-methods; a semi-structured ‘sleep experience’ questionnaire administered to a purposive sample of in-patients; recording of night-time noise levels, on 52 consecutive nights, using two calibrated Casella sound level meters.
Results:
Patient ratings of ‘in-hospital’ sleep quantity (3.25; 2.72 SD) and quality (2.91; 2.56 SD) was poorer compared to ‘home’ sleep quantity (5.07; 2.81 SD) and quality (5.52; 2.79 SD). The difference in sleep quality (p<0.001) and quantity (p<0.001) ratings whilst in hospital, compared to at home, was statistically significant. Care processes, noise from other patients and the built environment were common sources of sleep disturbance. Participants’ suggestions for improvement were similar to interventions identified in current research. The constant noise level ranged from 38-57 decibels (equivalent to an office environment), whilst peak levels reached a maximum of 116 decibels, (equivalent to banging a car door one metre away).
Conclusion:
The self-rated patient sleep experience was significantly poorer in hospital, compared to home. Noise at night contributed to sleep disturbance. Decibel levels were equivalent to those reported in other international studies. Data informed the development of a ‘Sleep Smart’ toolkit designed to improve the in-patient sleep experience.
1. INTRODUCTION
The quality of the physical environment in which care takes place is important because it contributes to patient safety and well-being [1]. Florence Nightingale highlighted the importance of a healing environment for hospital patients in her Environment Theory [2]. She drew attention to several important environmental factors that cause patient distress and delay recovery, including unwanted noise [2]. Positive patient care experience is an important indicator of high-quality health care [3]. However, the physical characteristics and milieu of the hospital setting make it a challenge to create a healing environment that promotes patient comfort and well-being [4].
Hospital in-patients are particularly in need of sleep for its restorative and healing properties, but 30-60% of in-patients experience sleep disturbance [5-8]. Studies show that in-patients experience dynamic changes in their sleeping patterns that can lead to sleep disruption and sleep deprivation [7, 9-11]. Sleep has an important biological function and is essential for good health. However, the prevalence of sleep insufficiency has led to its recognition as a public health epidemic [12]. Poor sleep is known to have a negative effect on all physiological systems; leading to abnormal emotional processing, reduced immune function, delayed wound healing and an increased risk of hypertension, diabetes, obesity, depression, heart attack, and stroke [13-17]. Poor sleep is also associated with delirium [18] and is an independent risk factor for falls [19]. Disruption to sleep patterns following hospitalisation can persist for up to a year after discharge to home [20]. At its most extreme, sleep deprivation is a form of torture [21]. Sleep quality is a rather neglected aspect of patient care and is typically underreported by health professionals, despite being an important factor contributing to optimal health and wellness [18].
Several factors cause sleep disturbances and sleep disruption for hospital in-patients, but noise, defined as ‘unwanted sound’ [22], is one of the most common causes [7, 23, 24]. The problem of unwanted night-time noise in hospitals is both widespread and significant, as over 17 million people are admitted to hospital each year in England alone [25]. Results from a UK patient experience survey, with a sample of over 70,000 respondents, indicate that 39% of patients reported being disturbed by noise from other patients and 20% by noise from the hospital staff [26]. Similar survey data collected from patients across America show that over 40% of the respondents reported noise around their bed space at night [27]. Unwanted noise in the workplace also has a negative impact on staff and can lead to lapses in concentration and at worst, burnout [28].
To understand how we can improve in-patient sleep, it is important to understand the patients’ perspective about their sleep experience, identify sources of disturbance, and accurately measure noise levels in the ward environment. Several studies have measured noise levels in critical care and operating theatre settings, but less is known about the soundscape of general wards [29]. Of the few published studies conducted on wards, common sources of noise at night reported by patients were staff conversations, other patients, alarms and ward equipment [7, 8, 30]. The World Health Organisation (WHO) has published guidelines for acceptable levels of environmental noise in hospital wards; a maximum sound level (LAmax) of 40 A-weighted decibels (dBA) and an equivalent continuous sound level (LAeq) of 30 dBA, overnight [31]. International studies have reported that noise levels in hospitals have increased over the past 50 years and frequently exceed WHO recommendations by approximately 20-40 dBA [32, 33]. It is readily apparent that the problem of unwanted noise at night is not new [34] despite it being a ubiquitous problem that impacts negatively on care quality and patients’ health and well-being. Additional research is required to understand in-patients’ experiences of sleep and the factors that cause sleep disturbance, including environmental noise. Little research has been conducted in ward settings, but existing evidence reports that noise reduction interventions are feasible and have the potential to improve patients’ sleep experiences [35]. Successful interventions may have the potential to mediate improved patient outcomes, shorten hospitalisations and improve the working environment for staff.
The aim of this multi-methods study, conducted on a Medical Assessment Unit, was to evaluate patient self-report questionnaire data (self-reported sleep quality/quantity at home and in-hospital, sources of in-hospital sleep-disturbance) and measure night-time noise levels.
2. MATERIAL AND METHODS
2.1. Study Design
A multi-methods study design was chosen to address the research aims. This was an appropriate design as we aimed to objectively measure noise levels in a Medical Assessment Unit and explore patients’ subjective sleep experiences and ideas for improvement using a brief researcher generated questionnaire.
2.2. Setting and Participants
We recruited a purposive sample of patients consecutively admitted to the Medical Assessment Unit (24 beds) of a district general hospital in Northern England. All eligible adult patients (≥18 years) admitted to the Medical Assessment Unit, for a minimum of one night, were invited to participate providing they were clinically stable, gave consent, and were able to communicate in English. Those participants who were completely deaf, or diagnosed with a sleep disorder were excluded. We aimed to recruit a sample of 150 participants, which is comparable to other similar studies [5, 8, 36].
2.3. Data Collection
The collection of the patient survey data and measurement of environmental noise levels took place in two concurrent phases, between September and November 2016, following ethical approval.
2.3.1. Phase 1. Development and administration of a brief ‘Sleep Experience Questionnaire’ (SEQ)
Several aspects of sleep can be evaluated. International recommendations tend to focus upon sleep quantity and recommend that adults aim for 7-8 hours of sleep to support healthy ageing [37]. For the purpose of this study, we chose to ask in-patients about sleep quantity and quality as both are important. We defined ‘sleep quantity’ as the total sleep time in hours, and ‘sleep quality’ as the subjective assessment of how refreshed and rested an individual felt after sleep [38]. A scoping review of available measures to assess patient sleep patterns identified the Richards-Campbell Sleep Questionnaire (RCSQ) as a potential measure [39]. However, the RCSQ had some limitations as it was validated for use in critical care settings [38]. Also, it does not fully assess the quality and quantity of sleep in the hospital, compared to that at home, from the patients’ perspective. We wanted to evaluate the considerable variation in individuals’ sleep-wake cycles [40] and began to understand how sleep quality, and quantity, altered at home compared to that in thehospital. As there were no suitable measures, we designed the brief ‘Sleep Experience Questionnaire’ (SEQ) in consultation with service users and a sleep scientist (available from authors on request). The measure included clinical and demographic items (e.g. age, gender, use of medication to promote sleep, use of a hearing aid, Modified Early Warning Score and self-reported pain rating) and questions designed to assess sleep quality and quantity, both at home, and in-hospital, self-rated by participants using 10 cm Visual Analogue Scales (VAS). Open-ended questions were also included to determine the aetiology of sleep disturbances in the Medical Assessment Unit and suggestions for ways to promote sleep for hospital in-patients from their own unique perspective. The questionnaire was circulated to a working group (2 service users, 4 health professionals, 5 academics including a sleep scientist) to support the face and content validity of the measure. In response to user feedback, the wordings used in question 5 and 6 was modified and a lay explanation of sleep quality and sleep quantity added.
During the data collection period, a senior nurse identified potential participants admitted before 22.00 hrs, on the previous night, who were clinically stable. A research nurse then screened participants against set exclusion criteria (inability to communicate in English, diagnosis with a sleep disorder, complete deafness). Study information was given to eligible participants and the opportunity to ask questions. Following informed consent, willing participants completed the paper-based SEQ.
2.3.2. Phase 2. Objective measurement of environmental night-time noise levels
Most studies recording environmental noise levels in hospitals have done so for a period of days, rather than months, and predominantly in critical care settings. We recorded night-time noise levels for a sustained period for three reasons; first, so that we could add a new perspective to what is known on this topic. Second, we could minimise the observer effect, which potentially undermines the integrity of research findings. Third, data from participant’s subjective assessment of sleep quality and quantity in the Medical Assessment Unit, and night-time noise level could be collected simultaneously. Data triangulation is a useful approach to validate research findings [41] and results using both data collection methods contributed to a comprehensive explanation of this phenomenon.
Noise levels were continuously recorded in one-minute intervals over each 24-hour period, using two sound level meters (Casella, model CEL-632C, Class 1) calibrated, as per manufacturer’s recommendations. The meter settings (fast i.e. a time constant of integration of 125ms and A-weighted) were chosen as recommended in the WHO guidelines [31].
The sound meters were located in two 4-bedded patient bays; one located at the end of the corridor, and the other room situated close to the nurses’ station in the centre of the unit. These bays represented a typically quieter (End Room) and a busier (Middle Room) clinical environment according to feedback from clinical staff. The microphone (Casella, CEL-251) for each sound level meter was secured to the ceiling in each bay. Sound level meters were calibrated regularly using an acoustic calibrator (Casella, CEL-120).
2.4. Data Analysis
2.4.1. Patient Questionnaire Data
Quantitative data were extracted from the questionnaires and data entered into SPSS (version 24). Data were analysed using descriptive and inferential statistics. VAS data for ‘sleep quality’ and ‘sleep quantity’ in hospital, and at home, were compared using paired samples t-tests with significance level set to 0.05.
Qualitative data from open-ended questions were analysed using thematic analysis to identify patterns or themes in the data [42]. This method matched the multi-method study design because it is not aligned with a specific epistemological perspective or qualitative methodology. Data were read, and re-read, as part of a familiarisation process. We coded the data using a theoretical approach as we had a specific research question. The aim was to explore patient-reported sources of sleep-disturbance to develop an aetiology specific to the Medical Assessment Unit setting using an inductive approach. We also wanted to understand participants’ views about suggestions for sleep-promoting strategies. To support the management and retrieval of qualitative data, we used Microsoft Excel, an approach used by others to provide an audit trail [43]. Using an open coding approach, one researcher developed a preliminary coding frame. A second researcher repeated the process independently to support the trustworthiness of the analytical process. Preliminary codes were compared, refined and grouped together to form themes, which were reviewed against the data set. There are two levels of themes in the thematic analysis [42]; in this analysis, we focused on each participant resulting in semantic themes that stayed close to the explicit meaning of the data set. The final stage of the six-stage analysis [42] was the refinement of the themes.
2.4.2. Environmental Night-time Noise Level Data
Environmental night-time noise levels were recorded for 52 consecutive days. Three parameters were studied; 1) maximum sound pressure level (LAmax dBA), 2) mean sound pressure level (LAeq dBA), 3) the number of night-time 15-minute intervals in which maximum sound pressure levels ≥ 80dBA. A technician downloaded sound level meter data daily using Casella Insight software. For completeness, details of the analytical approaches that were used are available on request from the authors.
3. RESULTS
3.1. Participant Characteristics
Two hundred and four patients were screened and eligible to participate. Of these, 147 (72%) agreed to participate. Two participants consented but did not complete items on self-reported sleep quality and quantity. The final sample comprised 145 participants. Participant characteristics and self-reported outcomes are summarised in Table 1.
| Participants (n=147) | Frequency (%) or Mean (SD) |
|---|---|
| Gender Male Female |
87 (59.2%) 60 (40.8%) |
| Age (years) | 67.0 (17.7) |
| Prescribed medication to induce sleep (n=145) Yes No |
21 (14.5%) 124 (85.5%) |
| Hearing impairment Yes No |
39 (26.5%) 108 (73.5%) |
| Modified Early Warning Score | 1.48 (1.94) (range 0-9) |
| Self-reported pain level (10-point Visual Analogue Scale) | 2.00 (2.56) (range 0-9) |
3.2. Self-Reported Sleep Quality and Quantity
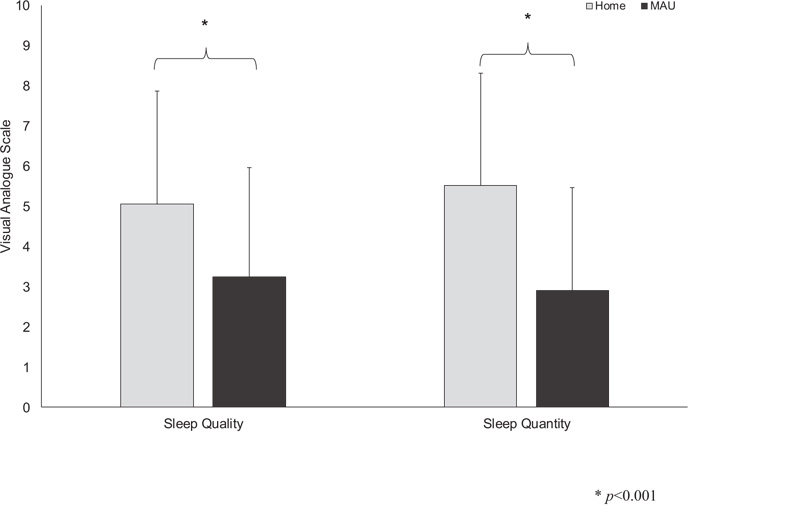
Fig. (1) shows data from a 10-point VAS of (n=145) participants’ self-reported sleep quality, and quantity.
Participants’ average home sleep quality was rated by participants as 5.07 (SD 2.81 points) and sleep quantity as 5.52 (SD 2.79 points). The average sleep quality and quantity on the Medical Assessment Unit was 3.25 points (SD 2.72 points) and 2.91 points (SD 2.56 points), respectively. Paired samples t-tests showed a statistically significant difference between self-reported sleep quality, and sleep quantity at home compared to that in the hospital. Participants reported poorer sleep quality and quantity whilst in hospital compared to that at home; a statistically significant decrease was evident in both parameters (t146=6.01, p<0.001) sleep quality; (t146=10.3, p<0.001) sleep quantity).
3.3. Qualitative Data
3.3.1. Aetiology of Sleep Disturbance in a Medical Assessment Unit
Five themes characterised the qualitative data from open-ended questions about sources of sleep disturbance shown in Fig. (2). Table 2 provides supporting details, including participants’ quotes and suggestions for improving in-patient sleep. Many participants did not think it was possible to reduce the level of noise in the ward.

| Theme | Frequency of Response to ‘What Caused Sleep Disturbance?’ | Participant Quotes on Causes of Sleep Disturbance | Participants’ Sleep-promoting Suggestions |
|---|---|---|---|
| 1. Care Processes | 62 |
“1am blood test. 2am X-ray. Woken up to do OBS”. “Doctor’s visit, Nurses taking swabs ƒ?" all roughly at 1- hour intervals rather than progressive and co-ordinated”. |
“Once patients are settled- try to leave them all together. Perhaps try to admit all new patients to the same area”. “Once stable patient could be moved to a quiet area and limit admissions to nearer the ward entrance”. |
| 2. Other Patients | 63 |
“The patient in the next bed was coughing and groaning”. “Worst factor in disturbing sleep was other patients snoring, vomiting and one patient very disruptive”. |
“Move noisy patients out of 4 bedded bay”. “Offer ear plugs”. “Headphones for the TV”. “The staff are doing the best they can. If there were more staff to attend to patients when they were anxious or distressed, it would be better”. |
| 3. Built Environment | 41 |
“A lot of beeping- especially from BP machine”. “Alarm from IVAC on another patient frequently during the night”. “Noise-doors banging”. “General ward noise-trolleys moving up and down the corridor outside the bay”. “Lots of noise from squeaky bed wheels and people moving around”. “I was very cold. I couldn’t settle”. “Staff had to use main room light because lamps were not working on either bed”. |
“Single rooms for all patients”. “Perhaps soundproofing the doors”. “Quieter equipment e.g. foot pedal on bin and bin lid”. “Possibly adjust the noise of the buzzers at night time. Have vibrating phones with light-up display for the Nurses- to reduce noise. (phones to be in nurses’ pocket) this would reduce delays in answering phones too”. “Use machines with a lower beeping noise or use machines which vibrate instead”. “Dampen noise on wheels of trolleys etc.” |
| 4. Physical and Emotional Factors | 38 |
“Pain and coughing (myself)”. “Pain in back. And bed uncomfortable”. “Kept getting up to the toilet”. “Change of environment-sleeping with strangers”. “Missed my own bed and bedding”. “Strange bed. Strange room. Anxious about my health. Anxious about my business.” |
“Asked for a sleeping tablet when admitted to the Medical Assessment Unit because of previous experience of sleepless nights here due to noise”. “Give medication on time- then not waiting around. Also, when you get the medication, it helps you get to sleep”. |
| 5. Staff Noise | 19 |
“Other things like nurses and patients coming and going, no-one lowered their voices”. “At 5.30am I was woken by noise in the corridor”. |
“Keep voices down a bit”. “If nurses can be as quiet as possible”. “Staff just being more aware that patients are in a bedroom trying to sleep”. |
3.3.1.1. Care Processes
In this theme, participants described a range of care processes that led to frequent night-time sleep disturbances. The broader health and social care team provided the care, which included nurses, health care assistants, doctors and allied health professionals. Participants were disturbed by a variety of care processes received by themselves or patients nearby, such as the monitoring of vital signs, the implementation of various diagnostic tests such as chest X-ray and blood tests, and the delivery of medication through nebulisers. Participants recognised that many of these clinical procedures were a necessary part of their health care, but commented on the lack of care co-ordination. Sleep promoting suggestions related to reducing or changing the organisation of patient admissions at night.
3.3.1.2. Other Patients
In this theme, participants described factors that caused sleep disturbance caused by other patients in the clinical area. The noise generated by patients was either ‘general’ or ‘specific’. Participants described ‘general noise’ from patients that did not have a single identifiable cause. Specific noises that caused their sleep disturbance reported by participants were often linked to physical noises such as patient snoring, coughing or audible breathing. Participants also mentioned the noise caused by patients needing to get up in the night to use the toilet or commode. However, the most commonly reported source of sleep disturbance was the noise from patients described as being distressed or disruptive who were talking, or shouting out. Participants suggested offering earplugs or headphones to in-patients to muffle environmental noise. An increase in staff numbers was suggested to provide additional care for distressed patients.
3.3.1.3. Built Environment
In this theme, participants described non-human factors in their environment that caused sleep disturbance. Most factors caused sleep disturbance by generating unwanted environmental noise. For example, participants identified a wide range of noise-generating fixtures and fittings. Participants reported sleep disturbance being caused by noise from doors and cupboards banging, trolleys, squeaky wheels on beds, televisions and a printer. Participants also described noise from medical devices and equipment used in the ward setting as sources of disturbance during the night. They described ‘beeping’, ‘bleeping’, and the noise from alarms, buzzers, call bells and intravenous fluid delivery pumps as sources of sleep disturbance. Ambient temperature and light were also identified by participants as sources of sleep disturbance; being either too hot or too cold and lights being switched on, or on and off. Providing individual patient rooms was the most common sleep-promoting suggestion offered by participants across all themes. Other suggestions included reducing the volume on alarms and buzzers and repairing or replacing noisy equipment such as bins and trolley wheels.
3.3.1.4. Physical and Emotional Factors
In this theme, participants described intrinsic physical symptoms or sensations that disturbed their sleep. Some participants complained of being in pain, coughing or feeling generally unwell, which made it difficult for them to sleep. Others mentioned that they needed to get up to go to the toilet frequently because of the effects of the medication they had been given. A few participants mentioned that they were feeling physically uncomfortable due to the mattress or pillow. Others mentioned that their sleep was disturbed because they were feeling tired, were unable to sleep or felt anxious.
3.3.1.5. Staff Noise
A small proportion of participants mentioned noise from staff as a source of sleep disturbance. This could be general noise from staff moving about the ward, or from staff talking to one another. Participants mentioned hearing singing, shouting, loud conversations and music that caused their sleep disturbance. One participant mentioned that the noise caused by staff opening and closing plastic folders had caused sleep disturbance. Participants suggested that staff talking could be reduced and staff awareness about the volume of noise caused by talking should be increased.
3.4. Night-time Noise Levels
Table 3 shows the data on noise levels recorded for 52 nights in total. During the entire data collection period, in both the ‘Middle Room’ and ‘End Room’, there were no 15-minute periods where sound pressure levels were within the WHO guidelines (i.e. LAmax ≤40 dBA and LAeq ≤30 dBA). No significant differences were observed between maximum or equivalent continuous noise levels at weekdays or weekends.
| Logarithmic Mean of Nightly Maximum Sound Pressure Level (LAmax dBA) | Logarithmic Mean of Nightly Equivalent Continuous Sound Pressure level (LAeq dBA) | Number of 15-minute Periods Where Maximum Sound Pressure Levels ≥ 80 dBA (mean (SD)) | |
|---|---|---|---|
| End Room | 102.60 | 49.20 | 23.94 (SD 5.83) |
| Middle Room | 106.43 | 51.59 | 26.42 (SD 4.67) |
4. DISCUSSION
This multi-methods study addressed two interrelated study objectives with findings that add new insights concerning patients’ sleep experiences and levels of night-time noise in a Medical Admissions Unit.
First, we evaluated participants’ reports of their sleep quantity and quality at home, and in a hospital. Second, we asked them about the causes of sleep disturbances during their hospital stay so we could develop an aetiology of sleep disturbances in the Medical Assessment Unit. We also asked participants to offer suggestions for ways to promote sleep for hospital in-patients at night.
Participants’ self-reported sleep quality and quantity were significantly poorer in the hospital compared to at home. This finding was not unexpected as several international studies have reported that between 40-60% of patients in hospitals report poor sleep quality [7, 44, 45]; with an average decrease in night-time sleep duration of 1.8 hours between home and in a hospital [7]. Our findings show a self-reported decrease in sleep of over 2 hours in a hospital compared to home. This suggests that patients in the Medical Assessment Unit are likely to experience fragmented sleep, which if sustained, could lead to sleep deprivation. In the short-term, sleep deprivation can have an immediate effect on the neuroendocrine and hormone systems (e.g. increased cortisol secretion), cardiovascular system (increased heart rate and blood pressure) and on behaviour and cognition (daytime sleepiness, reduced alertness, negative emotions) [46]. Sleep disturbance also has a long-term effect; studies have reported that in-patients’ sleep patterns are often disrupted for up to a year following a period of hospitalisation which has a negative impact on health and well-being [20]. International recommendations state that adults should aim for 7-8 hours of sleep to support healthy ageing [37]. Participants in this study reported an average sleep duration at home of 6 hours per night, which was unexpectedly low. Poor health and associated symptoms ahead of hospital admission may explain this finding. Alternatively, the older age of participants (mean age 67 years) may be a contributory factor as the ability to maintain sleep tends to decrease with age. A recent study from Australia provides some useful comparative data. The authors published data on the self-reported sleep duration, at home, of a sample of 144 participants with a mean age of 64.2 years as 7.1 hours [7]. The minimum (1 hour) and maximum (15 hours) sleep duration was surprisingly diverse [7]. From these data, we can assume that many in-patients may have accumulated a sleep deficit prior to hospital admission that could negatively influence their health and response to treatment. These data highlight the importance of a holistic patient assessment. Sleep and rest patterns are important aspects of biological function that should be assessed as part of person-centred care. Self-report data on sleep quality and quantity has some limitations and may be subject to recall bias. That said, studies comparing self-report data and polysomnography data have reported that the former tends to overestimate sleep quantity compared to the latter [47]. So the ‘at home’ sleep quality and quantity reported by our study participants may be potentially better than data recorded using objective techniques.
Findings from the qualitative data enabled us to develop a novel aetiology of sleep disturbance in a Medical Assessment Unit. The most frequently reported causes of sleep disturbance were care processes, noise from other patients, built environment and physical and emotional factors. There are surprisingly few recent studies available for comparison. A literature review on noise at night in general wards, published five years ago, reported that staff, other patients and visitors were the most common causes of environmental noise [48]. A more recent Australian study reported that clinical care provision, and noise from staff, as the most common causes of in-patient sleep disturbance [7]. A UK study that focused upon the acoustic environment of wards, rather than sources of sleep disturbance, reported ward equipment as the most common source of noise [30]. Medical Admissions Unit in-patients reported similar sources of noise.
Noise from other patients, rather than staff, was the second most frequently reported cause of sleep disturbance in this study, which contrasts with findings from other studies [7, 30, 48]. Our study participants described different types of noise generated by other patients. They identified physical factors, such as snoring and coughing, as causing sleep disturbance. Study participants also referred to ‘distressed’ or ‘disruptive’ patients as disturbing the sleep of other in-patients. Similar patient-related noise sources have been reported in other studies [36, 49, 50]. Noise from distressed or disruptive patients is stressful for both staff, patients and those close to them. As the average age of patients in general hospitals is 70 years of age, many in-patients are likely to have dementia and/or delirium. Furthermore, staff often lack specialist training to enable them to assess patients with dementia and develop appropriate interventions [51]. A new 24-hour service staffed by specialist support workers, trained to provide one-to-one care for distressed patients, was piloted at the participating organisation following this research. The use of single-patient rooms may offer an additional solution, but this approach may not always be practicable or desirable. A recent review identified both positive and negative aspects of caring for patients in single rooms [52]. The use of earplugs is a feasible alternative to reduce general background noise to reduce sleep disturbance, but is a less effective approach for masking peak noise levels [35].
Noise from the Built Environment, which we conceptualised as the building, medical equipment, fixtures and fittings, was the third most frequently reported cause of sleep disturbance by our study participants. Other studies have reported noise from alarms, doors, trolleys and cupboards as a common source of sleep disturbance [7, 48]. Findings from our study add to research on this important topic by confirming that whilst there are likely to be similarities in specific ‘noise generators’ across clinical settings, each has its own specific soundscape.
Participants’ physical and emotional status was reported as a potential source of sleep disturbances. For example, physical sensations such as pain and discomfort were reported as factors that caused sleep disturbances. Other studies have reported similar findings [6,7,10,53]. A closer look at the implementation of pain assessment protocols at night may address sleep disturbance caused by pain. It is accepted that interventions designed to educate nurses about acute pain management often lack theoretical foundation [54] and current practice could be improved [55]. Emotions and feelings linked to being in a strange environment with other people also caused sleep disturbances. Studies conducted in China and Iran have reported worries and concerns about health and illness as emotions that contributed to poor sleep quality for patients; this was also evident in our findings [44, 45].
In the final part of the qualitative study, we asked participants to make suggestions for improvements that could promote sleep and reduce sleep disturbance for in-patients. This is a unique and innovative aspect of this study as all too often, patients are not included in quality improvement initiatives. Interestingly participants’ suggestions broadly reflect several of the noise reduction interventions reported in a systematic review [35]. This demonstrates the value of seeking patients’ feedback in the development of health services.
In the second part of this study, we objectively measured night-time environmental noise levels over a 52-day period in a Medical Assessment Unit. The prolonged recording period of night-time noise levels in this study is a particular strength. Few studies have objectively and accurately recorded night-time noise levels in a ward setting for such a prolonged period. For this reason, our study makes an important and significant contribution to the current literature on this topic. The average night-time equivalent continuous sound pressure levels were between 38-57 dBA. This is categorised as a ‘soft’ to ‘moderate’ noise level, that at the higher level, is equivalent to office conversation. The decibel levels in this study were similar to those reported in an overview of studies published between 1964 and 2005; equivalent sound pressure levels were reported as between 35-82 dBA [33]. More recent studies conducted in medical, general surgical and orthopaedic wards report average equivalent sound levels of between 42-64.6 dBA [7, 8, 36, 56-59], whilst in critical care settings, levels can be 80dBA [8]. The highest and lowest maximum sound pressure across all nights, across both rooms, on the Medical Assessment Unit was between 94-116 dBA. This instantaneous noise level is very loud and equivalent to hearing a banging car door at one metre distance. A peak noise level of this magnitude is common in hospital settings; others have reported similar maximum sound level pressures of 100 dBA [7, 60].
There was no significant difference between average night-time equivalent continuous sound pressure levels and maximum sound pressure levels recorded on weekdays, compared to weekends. This was surprising, but the consistent patient flow rate through the Medical Assessment Unit provides a logical explanation for this finding. Over the last forty years, the (logarithmic) average night-time noise levels in a hospital setting have steadily increased [33]. It is clear from our study, and others, that hospitals are noisy places and are becoming increasingly so, largely due to the technological innovations that are now part of daily clinical practice. The level of noise required to cause sleep disturbance leading to poor health consequences is ≥ 55 dBA [61, 62]. Maximum sound pressure levels in the Medical Assessment Unit were consistently above this level.
Noise levels in the Medical Assessment Unit, and those reported in most international studies, exceed current WHO recommendations [31]. Unfortunately, WHO recommendations appear to be meaningless in today’s hospital environments as they set an unachievable target. In one study, noise levels recorded in an unoccupied room, set up with the equipment required for respiratory support alone, exceeded WHO recommendations [60].
Environmental noise levels recorded across different clinical settings vary considerably and multiple factors contribute to noise production and propagation. These include the architecture of the clinical setting, fixtures, fittings, equipment, the acuity of patients and the number of staff, to name a few [63]. A welcome addition to the WHO guidance would be directives on effective approaches to reduce noise to reduce sleep disturbance. Suggestions for interventions that can either eliminate noise at source, or reduce the propagation of noise, could be a valuable first step in supporting health and social care professionals to promote sleep for hospital in-patients.
Another important consideration is the quality and familiarity of specific sounds and their impact on patients. Sounds from alarms are more likely to cause disturbance than other sounds such as human voices [64]. It may be worth considering whether interventions should target a reduction in maximum/peak noise levels in clinical settings rather than average noise levels. For example, the cabin of a commercial flight has an average equivalent sound pressure in the region of 80-85 dBA [65], yet many people are able to sleep in this environment. Further research could establish whether sudden loud noises in a clinical environment are more likely to cause sleep disturbance than continuous background noise.
This study has some limitations. The setting was a single ward in one hospital, which may reduce the generalisability of the results to other settings. Conversely, the focus upon a single clinical setting enabled us to develop a very comprehensive understanding of the soundscape in the Medical Assessment Unit. It is widely accepted that patient self-report data may be prone to recall bias. However, the use of polysomnography, the gold standard to assess sleep, was not feasible due to the invasive nature of the data collection process and expense of the equipment. The prolonged recording period of night-time noise levels is a strength of this study because it is longer than that reported in the majority of comparable studies.
This study shows that the self-rated patient sleep experience was significantly poorer in the hospital, compared to home. Noise at night was a contributor to sleep disturbances in this study, with similar noise levels reported in other international studies. Future research should identify effective interventions to improve the quality and quantity of sleep for hospital in-patients. This is an important aspect of care because it influences the patient experience and health outcomes. Sleep deprivation is associated with poor physical and mental health. Moreover, sleep disturbance is associated with adverse events such as falls that lead to avoidable patient harm and prolonged hospital stay. This study provides a new aetiology of sleep disturbance, which shows that five key factors influence the patient sleep experience; additional research is needed to understand how such factors vary across different clinical settings. Several countries distribute patient experience surveys, but questionnaire items about the in-patient sleep experience are not consistently included and the specific sources of sleep disturbance poorly understood. Future research about sources of sleep disturbance caused by the ‘Built Environment’ are needed as this aspect of noise generation is often overlooked. Health architects play an important role in ‘designing out noise’ to create a healing environment in new hospital builds.
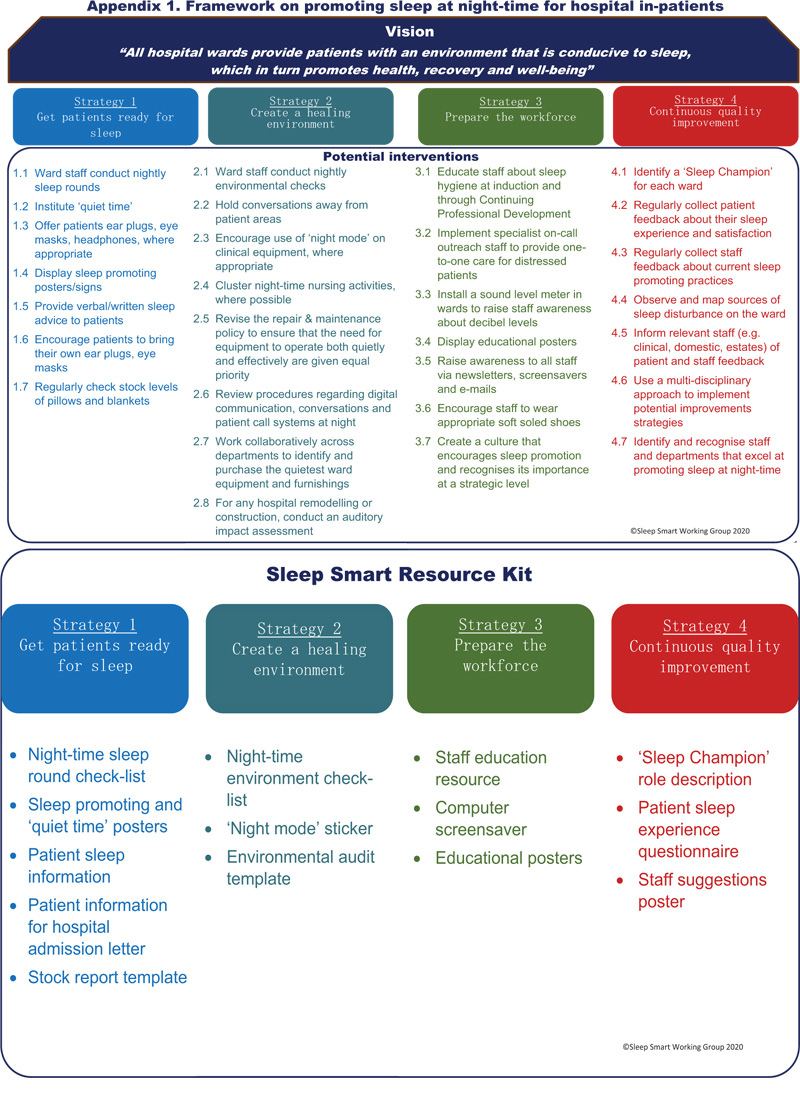
Research data informed the development of a research derived actionable ‘Sleep Smart’ toolkit designed for use by health professionals to guide the improvement of the in-patient sleep experience. Appendix 1 shows the sleep promotion framework and an overview of the ‘Sleep Smart’ toolkit (copyright © 2019 Sleep Smart Working Group) with additional resources available from the corresponding author.
CONCLUSION
This study confirms that sleep quality and quantity in a Medical Assessment Unit is significantly worse than at home. Most importantly, many patients admitted to the hospital due to ill health may already have a sleep deficit. The first aetiology of noise in the Medical Assessment Unit, from a patient perspective, shows that care processes, other patients and the built environment are key sources of sleep disturbance. Most importantly, our study shows that although sources of sleep disturbance may be broadly similar across clinical settings, each clinical setting is different. Noise levels at night in a Medical Assessment Unit, studied over a 52-day period, are above those recommended by the WHO [31], but similar to those reported in multiple international studies. The problem of noise at night in hospitals is not new, but does not seem to be a priority amongst those with the most significant influence. Several simple strategies can reduce noise at night and promote sleep. Unfortunately, no one factor can be singled out against another as having a greater or lesser impact on noise reduction or sleep promotion [35]. Noise from other patients may be reduced by considering ward layout and using noise ‘blocking’ interventions, such as ear plugs. Other approaches include reminders for staff to ensure that they close doors, avoid conversations in hallways or next to the bedside, turn televisions off or provide headphones for patients wanting the television on, provide earplugs, have pagers/phones on vibrate and implement ‘quiet hours’ [59, 66-70].
At a policy level, the current WHO guidance [31] requires urgent updates and the addition of an action plan for change. The most recent version of the guidance avoided making recommendations for acceptable noise levels in hospital settings, which is unfortunate [61]. An important first step should be to raise awareness at a governmental level to ensure that this important aspect of patient care is on the agenda for change. At a national level, hospital staff, patients, and those close to them, need to be at the forefront of ‘designing out noise’ in new hospitals. Specific attention to the redesign of patient flow between Accident and Emergency/Emergency Departments and other clinical areas is warranted to minimise night-time disturbance. National patient experience surveys could revise items to reflect the key themes in our aetiology when asking participants about what caused noise at night. Care processes and built environment are two important factors that are not currently included. Patient feedback is a powerful driver of improvement, but only if it is meaningful to health and social care staff. We recommend that hospitals develop and implement methods of providing patient feedback to staff on sources of sleep disturbance. The first step in cultural change is to raise awareness about the need for change. The impact of poor sleep on physiological and mental health requires more emphasis in health professional education. Using a “patient story” is a useful way to raise awareness at a local level particularly as feedback is more likely to be actionable if it is locally applicable and context-specific. At a local level, health and social care teams can evaluate the frequency of clinical observations and patterns of care provision at night to identify opportunities to reduce disturbances where possible. To achieve sustainable cultural change, the approach needs to be participatory, and the teams need to include all hospital staff, including those working in estates, portering and domestic services. Workforce managers could also consider implementing a night-time response outreach team of staff trained to sensitively, and safely, support distressed patients to reduce night-time disturbance. Change needs to occur at several levels if we are to address this challenge effectively.
AUTHORS' CONTRIBUTION
FA, JS, JW, BE, JG contributed to the successful funding application for the research. FA, JS, JW, BE, EH, PR contributed to data collection and/or data analysis. All authors contributed to drafting the manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Health Research Authority (16/NE/0269) and the Research Ethics Committee of the School of Human and Health Sciences at the University of Huddersfield, UK gave ethical approval for the research to be conducted.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All study participants gave informed consent to participate in the research which included the agreement that results would be published.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article.
FUNDING
This research was funded by a grant from the General Nursing Council of England and Wales.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest in this research and article writing.
ACKNOWLEDGEMENTS
We would like to thank all patient participants for their contribution. We would like to acknowledge Ms Beverley Holliday and Ms Kathryn Hanson (research nurses) for collecting the patient questionnaire data and the Working and Steering groups for their helpful input.
APPENDIX