All published articles of this journal are available on ScienceDirect.
Description and Validation of Nursing Diagnosis Using Electronic Documentation: Study Cases in Mother and Child Hospital Indonesia
Abstract
Background:
A nursing diagnosis is a clinical judgment concerning a human response to a health condition, vulnerability for that response, by an individual, family, group, or community. For the determination of the right nursing diagnosis, a system that guides nurses in implementing care professionally is needed.
Objective:
To describe the nursing diagnosis in mother and child cases validated by using a management nursing information system.
Methods:
This case study used secondary data from 5.294 medical records. Medical records were retrieved from the server, analyzed, and validated by using the mapping model in accordance with the most frequent cases in mothers and children in the hospital. Approximately ten million (10.021) nursing diagnoses were performed by nurses and validated by using a mapping model of medical cases and nursing assessment. The selected medical cases were the five most frequent cases, namely normal delivery, cesarean delivery, healthy newborn, fever, and dengue in children.
Results:
This study yielded the five most frequent nursing diagnoses, namely risk for infection (20.1%), pain (13.37%), anxiety (9.37%), the risk for imbalanced fluid volume (9.36%), and risk for bleeding (9.27%).
Conclusion:
The electronic nursing documentation could help to determine a nursing diagnosis and had been validated for its appropriateness with assessment and the most common cases in mothers and children. Information and system training development are required to carry out the nursing process comprehensively.
1. INTRODUCTION
Nursing care is a cycle of activity comprising assessment, nursing diagnosis, intervention, implementation, and evaluation. Excellent nursing care will guarantee the continuity of care and improve patient safety, inter-professional collaboration, and also patient continuity. Patient safety becomes the purpose of nursing care, and formulating accurate nursing diag-noses will lead to appropriate nursing interventions and guarantee patient safety.
The nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or vulnerability for that response, by an individual, family, group, or community. It is the process of determining a patient's problem preceded by a comprehensive assessment comprising biological, psychological, social, spiritual, and cultural. As a result of the critical thinking process, determining nursing diagnosis should be based on a correct and accurate assessment [1]. Formulating diagnosis refers to a problem and appropriate etiology to perform safe interventions for the patient. A nursing care plan is crucial to guide nursing care and patient care continuity. The nursing care plan should be documented and becomes a communication means among the healthcare team [2].
Implementation of nursing care is the translation of knowledge into practice. Translating diagnosis theory into practice still becomes a problem for nurses in Indonesia, considering diverse education in Indonesia. The previous study revealed that most nursing education has a vocational education background [3], it caused a lack of critical thinking in the continuity of care. Most of the vocational education in Indonesia also inhibited the process of determining accurate diagnosis and providing quality care [4]. Such a condition is similar to previous research explaining that the knowledge factor in 10 hospitals in Ethiopia influenced nursing care implementation and documentation [5].
Indonesia has established a national standard for formulating a nursing diagnosis, outcome, and intervention in 2018, but the implementation still required some improvement and evaluation. The previous research stated that the establishment of standard in nursing language could help and facilitate the nurses in performing nursing care [6, 7]. The use of language terminologies like The North America Nursing Diagnosis Association (NANDA), Nursing Intervention Classification (NIC), and Nursing outcome (NOC) helped nurses to think critically and improve their continuity [8].
Several studies found some discontinuity between assessment and nursing diagnosis, and also patient progress notes [9]. A similar condition also happened in Indonesia that the quality and the continuity of nursing care were still not optimal [10]. Being trapped in a routine and performing collaboration work also became a problem in implementing nursing care in Indonesia. The unavailability of an integrated clinical pathway guidebook in a hospital also contributed to the poor implementation of nursing care in Indonesia. Unstandardized diagnosis would contribute to errors in determining the nursing diagnosis [11].
Integrated Clinical Pathway (ICP) is a guidebook developed by the hospital to provide direction for multidiscipline healthcare providers. ICP also assists the nursing care following the patient's progress, which consists of daily target and nursing target to achieve. The implementation of ICP in Indonesia still requires more improvement. A study conducted in a hospital in Indonesia stated that the development of ICP modules, staff training, and developing an electronic system for nursing documentation could improve the implementation of nursing care and the completeness of nursing care documentation. Technology is capable of facilitating the implementation of nursing care [12].
Translation of nursing care theory into practice has also developed along with the advancement of science and technology. The use of electronic nursing documentation enabled nurses to perform more effective and efficient nursing care [13, 14]. The implementation of computer-based care also improved nurses' continuity, and the use of standardized nursing language also increased critical thinking and facilitated the continuity among items in the nursing process [15, 16].
2. METHODS
This study is a case study that described nursing diagnosis formulation and its validity using the electronic nursing documentation system. This study also described the use of nursing language standards in facilitating the nurse to determine nursing diagnosis and intervention. This case study used secondary data from the electronic nursing documentation in a mother and child hospital.
The samples selected from medical diagnosis were the five most frequent cases, namely normal labor, cesarean delivery, healthy newborn, fever, and dengue in children. Five million two hundred ninety-four (5.294) patient medical records were chosen by the computer. Medical records (MR) were retrieved from the server, analyzed, and described by using the mapping model following the most frequent cases in mothers and children in the hospital. Approximately ten million (10,021) nursing diagnoses were performed by nurses, with each patient having an average of two nursing diagnoses. The nursing diagnosis was determined and validated by using a mapping model of medical cases and assessments.
Ethical clearance got approval from The Faculty of Nursing, Universitas Indonesia. Researchers ensure the confidentiality of the patient's medical records anonymously, and all data is coded and stored using a password and username. Researchers also guarantee data only used for research and scientific purposes. The patients' data were kept in strict confidence and only used for research and learning purposes.
3. RESULTS
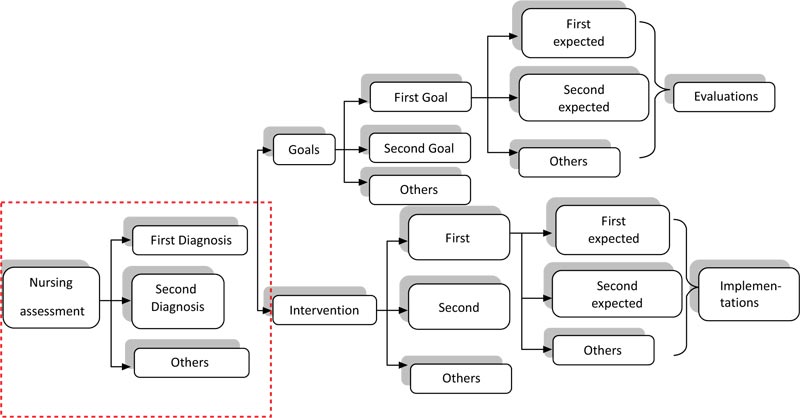
Nursing Management Information system provides a number of nursing diagnosis options and the nurses are required to use their clinical judgement to determine the nursing diagnosis. The following chart explains the process of nursing care plans in the nursing management information system (Fig. 1). Nursing care plan flowchart in nursing management information system.
Fig. (1) shows the flowchart of the nursing management information system. Nurses would have to complete the nursing assessment at first. The compound results of the assessment would suggest the recommended nursing diagnosis. This system uses the North American Nursing Diagnosis Association (NANDA), Nursing Intervention Classification (NIC), and Nursing Out Come (NOC) language [14]. Once the nursing diagnosis is confirmed by the nurse, a set of nursing outcomes referring to the nursing diagnosis would appear. Nurses need to decide suitable outcomes based on the patient’s condition. This process would be applied to nursing interventions. A number of interventions pertinent to diagnosis and outcomes would appear to guide the nurses in selecting the appropriate intervention. Nursing notes would be made in accordance with the complete electronic-based nursing documentation.
| No. | Diagnosis | Domain | Frequency | Percentage |
|---|---|---|---|---|
|
1 2 3 4 5 6 7 8 9 10 11 12 13 |
Risk for infection Acute pain/Postpartum pain Anxiety Risk for imbalanced fluid volume Risk for bleeding Self-care deficit Hypothermia Insufficient breast milk Hyperthermia Risk for imbalanced body temperature Ineffective infant feeding pattern Impaired physical mobility Other |
Safety/protection Comfort Coping/stress tolerance Nutrition Safety/protection Activity/rest Safety/protection Nutrition Safety/protection Safety/protection Nutrition Activity/rest Other |
1,709 1,137 797 796 788 734 433 352 259 211 203 138 2,464 |
20.1 13.37 9.37 9.36 9.27 8.63 5.09 4.14 3.05 2.48 2.39 1.62 11.13 |
| 10.021 | 100 |
Table 1 shows the thirteen-most frequent nursing diagnoses. Nutrition and safety/protection are the most common domains that have been set by the nurse, followed by domain activity and rest, comfort, and stress tolerance. This study also validated the nursing diagnosis from 5.294 medical records under five most frequent cases, namely normal parturition, section cesarean labor, healthy newborn, fever, and dengue in children. Meanwhile, the order of five most frequent nursing diagnosis in mother and child was a risk for infection (20.1%), postpartum pain (13.37%), anxiety (9.37%), the risk for imbalanced fluid volume (9.36%), and risk for bleeding (9.27%).
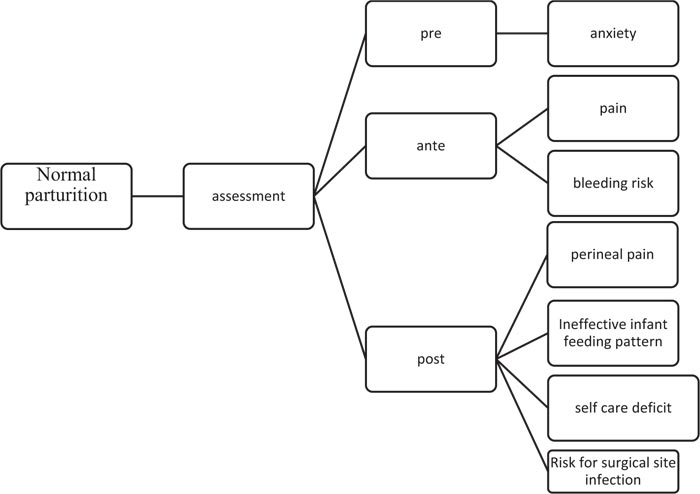
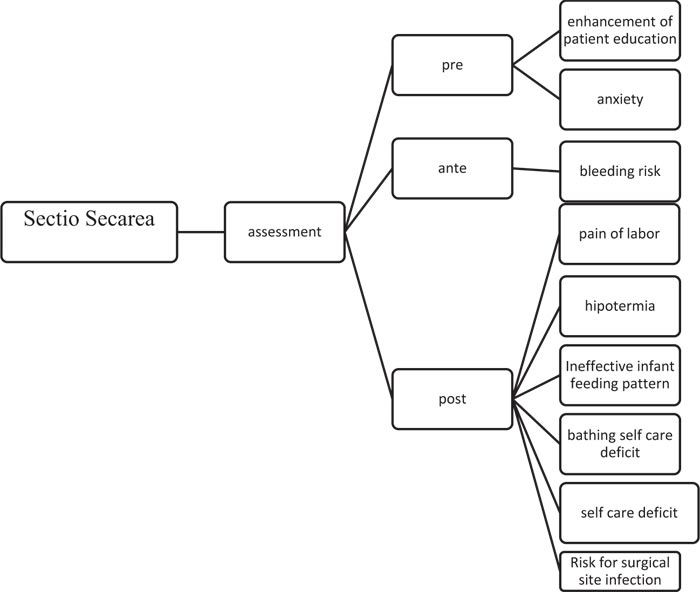
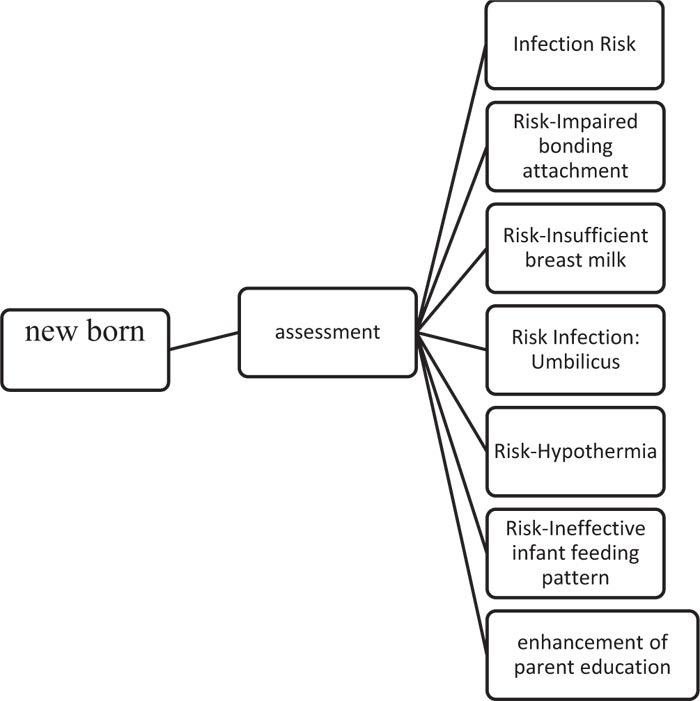
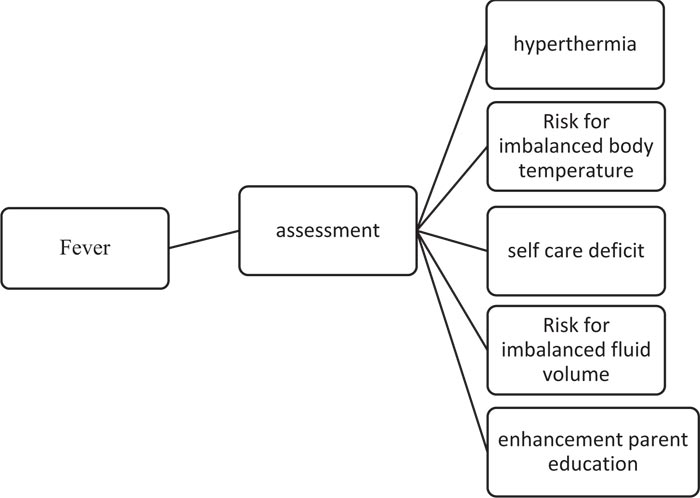
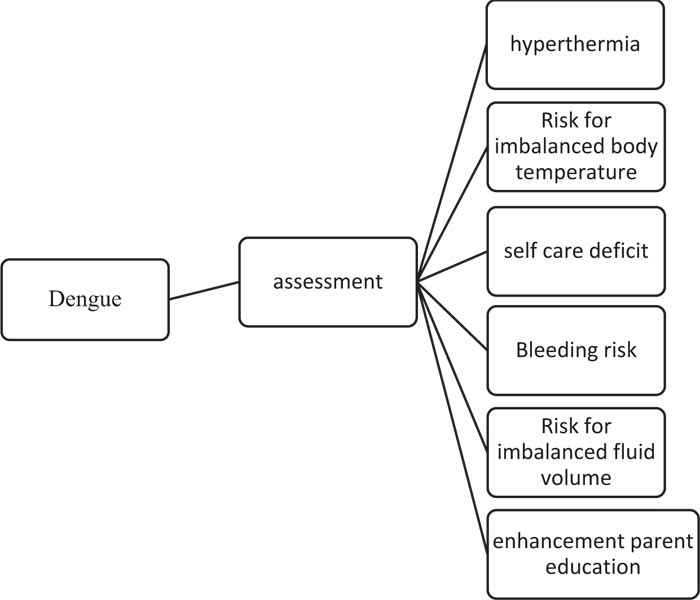
Fig. (2a-e) shows the mapping of five nursing diagnoses most stated in this study. The result of the nursing diagnosis develops from some symptoms. After the assessment, the nurse documented in the system, after that, the system will recommend choosing a nursing diagnosis. The statement of diagnosis described was relevant to previous research.
4. DISCUSSION
A nursing diagnosis is a judgement based on a comprehensive nursing assessment. The medical diagnosis provides an essential set of data, but it did not automatically require to make an accurate nursing diagnosis. Therefore, before the nurses state the problem, they have to conduct a patient assessment. The patient assessed first to determine the nursing diagnosis, which then followed by the outcome criteria and interventions.
Data of initial assessment in the system, reassessment, nursing care plan, and its implementation documented medical records. In the era of 4.0 technology, hospitals need a management information system. Information is required to give, coordinate, and also integrate the hospital service. Hospital plans and designs the management information process to meet the internal and external information needs (Standard Information and Medical Record Management /MIRM). The hospital management information system prepared the collection, provided data and information regularly, collected based on the needs of the professional caregiver, head of a division, head of a service unit, and other parties outside the hospital (SNARS; MIRM Standard.4). The use of an information system will help to present the data fast and accurately.
A nurse competence stated nurse diagnosis based on comprehensive assessment comprising physical, health history, allergy history, nutrition screening, pain, functional status, psychological, social, economic, spiritual, cultural, and discharge planning assessment [17].
The five most frequent cases in this study were normal parturition, section cesarean, healthy newborn, fever, and dengue in children, and the most frequent nursing diagnosis was a risk for infection (20.1%). Risk diagnosis referred to clinical judgment concerning the susceptibility of an individual, family, group, or community for developing an undesirable human response to health condition/life processes. The risk for infection might refer to the neonates who need special treatment for their umbilicus and also for normal and cesarean parturition. This result relevant to the previous studies that presented the final set of validated nursing diagnoses in ICU was a risk for infection [18, 19].
The second most frequent nursing diagnosis retrieved from the electronic system was pain (13.37%). The mother felt perineal pain after normal or cesarean parturition. This condition followed the previous research that explained postpartum commonly felt in the injury perineal area and might last for three (3) months, six (6) months, up to a year. Such pain might affect daily life, emotion, and also well-being. Pain assessment could be conducted using a visual analogic scale/VAS [20], or numerical scale, and completed with provocation, quality, radius, severity, and time of pain. The correct pain assessment would determine pain interventions, education of pain-relieving through recommended “kegel” and pelvic exercise (week, 2019). Another study found individual approaches could reduce pain pre-, ante- and post-natal [21].
Anxiety is the third most frequent nursing diagnosis in mother and child hospital. Previous research examined the correlation between anxiety and pain experiences [22]. In this study, anxiety could happen before Caesarea surgery, during neonate treatment and interaction, or when treating a child who suffered from fever or dengue. Nurses play an essential role in relapse anxiety because anxiety could inhibit recovery. Nurses could give information related to the care plan, what to do, treatment steps, and prepare the family to be able to take care of the patient after discharge. This statement is relevant to the Communication and Education Management Standard in SNARS, and nurses should play their roles based on this standard [17].
The risks for imbalanced fluid volume and bleeding are the fourth and fifth most frequent nursing diagnoses in mother and child hospital. Many children hospitalise because of fever conditions. This research is similar to previous research that validated 131 patients, and the risk for imbalanced fluid volume and bleeding becomes the final set of 32 most frequent nursing diagnoses [18]. Determining risk for imbalanced fluid volume and the bleeding had implications for a nurse to observe a balance of intake output, vital signs, and also early warning system. Standard of Patient Care and Services in SNARS emphasized to do monitoring and conduct protocol of early warning system [17].
From the Third-teen most frequent and validated nursing diagnoses, the weakness found is that determining diagnosis related to culture, spirituality, and the need for education is not identified yet. Educating patients and family is essential, concerning that structured education and discharge planning could reduce anxiety, shorten the length of stay, and reduce readmission rates [23].
A comprehensive assessment will lead to correct diagnosis and interventions [9]. In Patient Assessment Standard, it was stated that the person in charge to conduct an initial examination, determine a diagnosis, and intervention should be a professional nurse [17]. However, in Hospital “X”, most of the nurse's educational background is vocational, so this condition made a gap in determining the nursing diagnosis. The previous research stated that education and nursing knowledge is related to the quality of nursing care [3, 10, 11, 23, 24].
The nursing information system facilitated the nurses to formulate the nursing diagnosis because it links the suggested assessment to diagnosis. The nursing management information system is a combination of computer science, informatics science, and nursing science to facilitate management and the process of information and knowledge retrieval used to support the implementation of nursing care. The nursing management information system in the hospital is required to improve the effectiveness and efficiency of nursing services [14]. Such standardization can help to present the clinical data standards easily and fast. Moreover, it can improve the quality of clinical information and simultaneously increase a nurse's time to focus on core services. Besides, the nursing management information system has the accessibility and legality to help nurses obtain the information of the patient [16, 25].
Nursing management information systems can reduce human error, improve human behavior, and enhance the role of the nurse to improve the quality of care with higher capability supported by advanced technology [25, 26]. The SIM program linked with nursing diagnosis, intervention, and outcomes might assist the nurses to organize the nursing care plan [16]. From the assessment data resulted, the program will be linked to Nursing Diagnosis Association by the filled assessment. Therefore, the nursing care plan in the nursing management information system allows the nurses to provide continuous nursing care (continuity of nursing care) to address the holistic patient response. Continuity of nursing care is the integration of concepts and realities of the clinic, involved a variety of interdisciplinary sciences and organizations. Continuity of care helps nurses to improve nursing care [27] and effective communication to be able to evaluate the effectiveness of nursing actions performed in a responsible manner [28, 29].
CONCLUSION AND RECOMMENDATION
A case study described that the nursing system helps a nurse to state diagnosis. There were five most frequent nursing diagnoses in Mother and Child Hospital, namely risk for infection, pain, anxiety, the risk for imbalanced fluid volume, and risk for bleeding. This system helped the nurses to formulate nursing diagnoses that the result of the nursing diagnosis develops from some symptoms assessment. The statement of diagnosis described was validated by the system and relevant to previous research. Improvement in education and skills is required to conduct an assessment, determine diagnosis, and interventions. The research recommended that a management information system is used in the hospital to facilitate the nurses in determining diagnosis and making the decision for the nursing care plan.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the The Faculty of Nursing, Universitas Indonesia, Indonesia with approval number 169/H2.F12.D/HKp.02.04/2013.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study is funded by Grant International Collaboration from UI DRPM, Indonesia (Number NKB 1913/2019).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Thanks to FoN UI, UI DRPM, and team member: Ariesta, Yusnita, Shanty, Dhika, Iin, Difa, Tika, Dita, Usi, Widi, Windi, Fizo, Furqan, Ridwan, Marjuqi, Kinta.


