All published articles of this journal are available on ScienceDirect.
Nursing-Based Guidelines for Caregivers regarding Adult Patients with Percutaneous Endoscopic Gastrostomy
Abstract
Background:
Percutaneous Endoscopic Gastrostomy (PEG) may cause complications when the management is inadequate and inappropriate. To avoid these complications, caregivers’ experiences and practices must be considered.
Study Aim:
This study aimed to evaluate the effect of nursing- based guidelines on caregivers’ knowledge and practices regarding adult patients with percutaneous endoscopic gastrostomy.
Methods:
A quasi-experimental design was used. The study was conducted in the medical and surgical departments in the National Cancer Institute, Cairo University, Egypt. Sample: The sample consisted of 30 patients with PEG and their caregivers. A Structured interviewing questionnaire, Self-Administered Structured Questionnaire for caregiver, Caregiver Performance observation checklist, and PEG-specific questionnaire were obtained for data collection
Results:
The majority of studied patients (86.7%) were suffering from oncologic problems, in post-test and following up, the majority (83.3%) of caregivers had satisfactory level (76.7) (90%) (70%) in knowledge, complication and management of PEG, respectively. During follow up, the majority (73.3%) (90%) of caregivers were well level as regarding nutritional management and care of PEG. There were statistically significant differences between pre/post and follow-up nursing-based guidelines for caregivers’ knowledge and practice regarding patients with percutaneous endoscopic gastrostomy. The results show an improvement in the patients outcomes and the level of caregiver coping with the care of PEG and overall Patient satisfaction at (χ2 = 3.844, 4.097) p<0.001
Conclusion:
Nursing-based guidelines were helpful in the improvement of the caregiver's knowledge and practice regarding percutaneous endoscopic gastrostomy.
Recommendations
Periodic educational training programs regarding PEG were based on the best practice guidelines for caregivers of those patients.
1. INTRODUCTION
Percutaneous Endoscopic Gastrostomy (PEG) tube feeding is characterized by a successful and safe procedure for feeding patients with impaired swallowing [1]. The PEG is used for deteriorating neuromuscular disorders, and the advantages of PEG tubes are improving the body’s status by nutritional support in oncologic and pediatric patients [2, 3].
PEG provides support for patients with long-term enteral feeding, and advantages over parenteral nutrition [4]. With the advancement in the field, PEG tube placement is performed by endoscopic procedures worldwide and estimated 100000-125000 procedures are performed annually in the United States [5].
The most important function (PEG) is to provide a route for enteral feeding and hydration and drug administration for patients. A gastrostomy tube placed endoscopically is usually a better choice than surgical placement [6].
From minor complications such as peristomal wound infection and tube leakage into the abdominal cavity causing peritonitis, stoma leakage, inadvertent PEG removal, tube blockage, pneumoperitoneum, and gastric outlet obstruction, other complications, such as hemorrhage, necrotizing fasciitis, bumper syndrome, aspiration pneumonia, perforated viscus, colonic fistula, and metastatic seeding may occur which are considered major problems [7].
Pre-insertion, the nurse discussed the goals and diagnosis to obtain informed consent from the patient and family. In some conditions, through PEG, patient's survival and nutritional conditions improved along with their quality of life [4].
Awareness of these complications and the use of preventive strategies can allow the endoscopist to maximize outcomes and to identify complications at an earlier stage. As with any invasive technique, a thorough knowledge of purpose, indications, and fundamental procedural steps constitutes the most important safety factor [8, 9].
The patient and caregiver should be aware of and meet with all members of the Health Professional team involved in the process of gastrostomy insertion as the ongoing care is an important part of the management of many patients and caregivers [10]. Quality of PEG tubes care begins at pre-insertion assessment and during post-insertion aftercare. The prevention of complications and proper management is critical to ensure a successful outcome [4].
Nurses are mainly providing care to patients with PEG tubes. It is important that health professionals’ team have the knowledge and skills to provide information to the patients and their families to provide the best possible care for patients with a PEG [11]. Also, the patient/ caregivers should be instructed and provided with written information on safe and effective gastrostomy tube care and feeding. The risk predictors for increased adverse events are related to PEG feeding, as well as a consequently extended hospital stay due to the patient’s physical and nutritional status [12].
1.1. Significance & Justification
PEG insertion for adults will result in an improvement in the quality of life of patients and their families rather than just maintaining the patients’ life, and saving time for the caregivers. The responsibilities of the nurses are to support and educate the caretakers and patients for home enteral feeding to meet their requirements to reduce problems and complications, since the lack of standardized nursing-based guidelines for monitoring patients receiving PEG and for educating patients/ caregivers about management and practices may result in complications.
1.2. Aim of the Study
This study aimed to evaluate the effect of nursing-based guidelines on the caregivers’ knowledge and practices regarding adult patients with percutaneous endoscopic gastrostomy.
1.3. Research Question
1.3.1 What is the effect of nursing-based guidelines on the caregivers’ knowledge and practices regarding their adult patients with percutaneous endoscopic gastrostomy?
1.3.2 What is the effect of caregivers’ knowledge and practices on their adult patient’s progress with percutaneous endoscopic gastrostomy?
2. MATERIALS AND METHODS
2.1. Research Design
The quasi-experimental design was utilized to achieve the aim of the current study. The pre-test (control group) – post-test (study group) designs are the preferred methods to compare participant patients and their caregivers to measure change occurring after the nursing-guidelines intervention.
2.2. Setting
The study was conducted at the medical and surgical departments in the National Cancer Institute, Cairo University, Egypt.
2.3. Sample
A purposive sample of adult patients with new insertion for PEG within three months was obtained from the previously mentioned settings. The total number was 30 patients from both genders and their caregivers, above 18 years, with different educational levels, willing to participate in the study.
2.4. Tools for Data Collection
Four different tools were used to collect data pertinent to this study. They included the following:
2.4.1. Structured Interviewing Questionnaire
It was developed by the researcher in a simple Arabic language; it contained two parts; the 1st part was concerned with socio-demographic characteristics of studied patients, such as “age, gender, level of education, financial status, marital status” and the 2nd part was used to assess physical health and nutritional condition of patients [10].
2.4.2. A Self-Administered Structured Questionnaire for the Caregiver
It was developed by the researcher in a simple Arabic language and comprised of two parts. The 1st part was concerned with the characteristics of studied caregivers, such as “age, gender, level of education, marital status, and types of caregiver relationship. The 2nd part assessed caregivers’ level of knowledge pre/post and follow-up nursing-based guidelines regarding PEG based on the related literature [6, 13, 14]. It included knowledge regarding definition, indications, contraindications, benefits, complications, drugs’ administration, and nutritional care for the patient with PEG after discharge.
The total score of the questionnaire was 60 degrees, which represents 100%, total scoring for general knowledge about PEG was 32 degrees and knowledge of management and complication of PEG was equal to 28 degrees. The scores were distributed according to the importance of the items. Below 50% was graded as unsatisfactory and 50% and above were graded as satisfactory.
2.4.3. Caregiver Practice Observational Checklist
The observational checklist was developed and constructed by the researchers based on the related literature [15, 16]. An observational checklist was designed to assess caregivers’ practice regarding Percutaneous Endoscopic Gastrostomy. It includes three parts used to assess caregivers’ practice regarding drug administration, nutritional management, and gastrostomy site care.
The total score of the questionnaire was 100 degrees, which represents 100%. Total score for drugs administration was 20 degrees, for nutritional management, 48 degrees and for gastrostomy site care, 32 degrees. The scores were distributed according to the importance of the items. Below 50% was graded as poor level and 50% to 75% was graded as average level, and more than75% was graded as good (with satisfaction).
2.4.4. PEG-specific Questionnaire
It was written in a simple Arabic language, developed by the researchers based on the related literature [16] to measure patient’ progressive/outcome, including physical condition, nutritional state, and caregiver experience. It comprised of three parts. The first part was concerned with the physical condition (patient's health status includes gastrointestinal symptoms, gastrostomy site, and tube troubleshooting). The second part was concerned with the nutritional state to include current body weight and measure the Mini Nutritional Assessment [17], which included screening score max. 14points; The score of 12-14 points was designated as normal nutritional status, 8-11 points score indicated risk of malnutrition and 0-7 points score indicated malnourishment. The third part was used to assess patient’s/caregiver’s experience, including the level of coping for the caregiver and overall patient satisfaction. It was applied in the post follow-up based on the nursing-based guideline.
2.5. Educational Guidelines
Educational guidelines were designed by the researchers based on the needs of the studied caregivers to improve their knowledge and practice and evaluate the effect of nursing-based guidelines on caregivers’ knowledge and practices regarding adult patients with PEG-based on the related literature [15, 18]. These were written in the Arabic language based on four parts. The first part consists of knowledge related to PEG (as definition, types, indications, Contraindications, benefits, complications). The second part included knowledge regarding care for patients with PEG (as preoperative, immediate postoperative, general care after discharge). The third part included knowledge regarding care at home (as daily skincare, tube care, feeding through a tube, drug administration through the tube, nutritional support and emergency events that require informing the physician). The fourth part included knowledge regarding common problems from PEG (problem, causes, and management to problem).
2.6. Operational Definition
The guideline is a statement to establish the control of action, which aims to simplify particular processes according to the normal routine or practice evidence-based health care.
2.7. Validity and Reliability
Testing validity includes face validity aimed at inspecting the tools for clarity, relevance, comprehensiveness, simplicity, and applicability. Minor modifications were done such as content validity for all tools and educational guidelines were revised by 5 nursing specialists in the Medical-Surgical Nursing Department at the Faculty of Nursing, Ain Shams University for the content validity to ensure that the assessment tool produces stable and consistent results over time. Tools’ reliability: Cronbach's Alpha test was used to measure the internal consistency of tools. It showed good reliability scores for the following tools: (second part from Self-Administered Structured Questionnaire for caregiver = 0.708 and Caregiver Performance observation checklist = 0.79).
2.8. Pilot Study
It was conducted on 5 caregivers to test the tools regarding clarity, applicability, and feasibility. Based on the result of the pilot study, alterations and deletion of some details were performed and then the final formats were developed. The caregivers who were shared in the pilot study were removed from the sample of the current study.
2.9. Procedures of the Study
This study was conducted through four consecutive phases: assessment, planning, implementation, and evaluation. Data collection was done pre/post- guidelines implementation from May till August 2019.
- Assessment phase: This phase aimed at assessing the studied patients' and caregivers' demographic characteristics and assessing knowledge and practice of caregivers with regard to adult patients with PEG pre-guidelines implementation.
- Planning and preparatory phase: Based on the assessment phase, the content and media of the guidelines (in the form of visual materials) were prepared by the researchers, and the tools were tested by the pilot study.
- Implementation phase: The observation checklist was applied by the researchers who were available 6 days per week alternatively in the study settings in the morning shift. The questionnaire was administered in the clinical area to the studied patients and caregivers in the presence of the researchers. The assessment was done in the first four weeks for the total study sample. The total numbers of caregivers were 30, divided into five main groups according to the study settings, and then implementation of the guidelines was carried out at the previously mentioned study settings for each group separately based on their needs. The duration of each interview took approximately 1 to 1.5 hours; the interview started according to caregivers' available time. The Arabic language was used to facilitate the caregivers' level of understanding. Methods of teaching used were real situations, modified lectures, group discussions and demonstrations. An instructional media was used; it included the guidelines handout and audiovisual materials.
- Evaluation phase: It evaluated the effect of the nursing-based guidelines on caregivers’ knowledge and practice to compare between the results pre/post-intervention and after three months follow-up, measuring the patients’ progress in the follow-up to compare with post-intervention of nursing-guideline only (in pre-intervention progress of the patients, there was a new case of PEG, so no comparison was made with post or follow-up).
2.10. Data Analysis
The data were analyzed using descriptive analysis in the form of min/max, mean, and Standard Deviation (SD). The paired sample t-test was employed to determine the difference between subjects before/after program using Statistical Package for Social Sciences (SPSS) v.16 for Windows.
3. RESULTS
3.1 . Structured Interviewing Questionnaire
The current study showed the distribution of socio-demographic characteristics of the studied patients; the mean age was 55 ±10.3 years ranging from 33 - 75 years, and more than two-thirds (70%) were male with 76.7% of them having a low financial status. Less than half (46.7%) of them were illiterate, and one-fifths (20%) had a primary level of education. Regarding the marital status, more than half of the studied patients (63.3%) were married, while less than one-quarter of them (23.3%) were widow as shown in Table (1).
Regarding the physical health and nutritional assessment of studied patients with PEG, the result showed that the majority of them (86.7% & 80%) were suffering from the oncologic disorder and used to perform oral hygiene. While less than two-thirds of them (60%) were found taking prescribed chemotherapy treatment and half of the studied patients (50%) were inserted PEG recently. More than two-thirds of the patients (63.3% and 66.7%) had no problems in the pre-gastrostomy insertion site with a clean surgical wound site and more than half of them (56.7%) were under feeding plan as shown in Table (2).
| Items | No. = 30 | % | ||
| Age | - | Mean ±SD 55 ±10.3 Min -Max 33 -75 |
||
| Gender |
• Male • Female |
21 9 |
70.0 30.0 |
|
| Level of education • Illiterate • Primary • Secondary • Higher school • University |
14 6 4 3 3 |
46.7 20.0 13.3 10 10 |
||
| Financial status • Enough • Not enough |
7 23 |
23.3 76.7 |
||
| Marital status • Single • Married • Divorced • Widowed |
1 19 3 7 |
3.3 63.3 10 23.3 |
||
| Items | No = 30 | % |
|---|---|---|
| Present medical diagnosis • Neurologic disorder • Oncologic disorder |
4 26 |
13.3 86.7 |
| Duration of PEG insertion • Month • 2 month • 3 months |
15 13 2 |
50.0 45.3 6.7 |
| Current taking prescribed treatment for a physical illness? • Chemotherapy • Radiotherapy • Maintain medication |
18 2 10 |
60.0 6.7 33.3 |
| Pre gastrostomy insertion site • No-problem • Bleeding • Redness • Increasing pain |
19 1 6 4 |
63.3 3.3 20 13.3 |
| Surgical wound site • Clean site • Redness |
20 10 |
66.7 33.3 |
| Oral hygiene • Perform • Not perform |
24 6 |
80 20 |
| Patient underfeeding plan • Yes • No |
17 13 |
56.7 43.3 |
3.2. A Self-Administered Structured Questionnaire for the Caregiver
The present study according to the first part was concerned with the characteristics of the studied caregivers showing their age and sex distribution, more than half of them (60%) were male and two-fifths of them (40%) were between 20 to 29 years old as shown in Fig. (1).
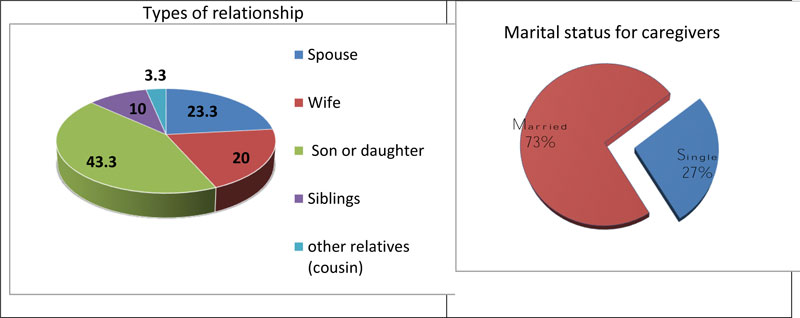
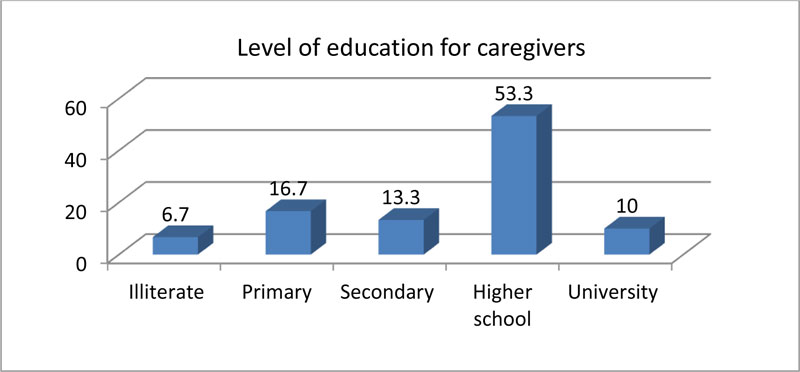
Regarding the types of relationship, less than half studied caregivers (43.3%) were sons or daughters, while less than one-quarter of them (23.3%) were spouses while nearly three-quarter (73.3%) of them were married as shown in Fig. (2). Also, as far as education is concerned, more than half of them (53.3%) were from high school (Fig. 3).
The second part of assessing caregivers’ level of knowledge pre/post and follow-up nursing-based guidelines regarding PEG showed that the majority (86.7%) (96.7%) of caregiver had an unsatisfactory level of knowledge of the complication and management of PEG in pre-test, while post-test and at follow up, the majority (83.3%) (76.7%) (90%) (70%) of them had satisfactory level of knowledge about the complication and management of PEG. So, there were highly statistically significant differences in the findings pre/post test and at follow up (P value is significant (f = 50.8, f =78.2 at p < 0.001) as shown in Table (3).

| Items | Pre-test | Post-test | Follow-up after 3 Months |
F | p-value | |||
| No. | % | No. | % | No. | % | |||
|
Knowledge about PEG. ▪ Satisfactory ▪ Unsatisfactory |
4 26 |
13.3 86.7 |
25 5 |
83.3 16.7 |
23 7 |
76.7 23.3 |
50.8 | HS 0.000 |
|
Knowledge about Complication and management of PEG. ▪ Satisfactory ▪ Unsatisfactory |
1 29 |
3.3 96.7 |
27 3 |
90.0 10.0 |
21 9 |
70.0 30.0 |
78.2 | HS 0.000 |
3.3. Caregiver Practice Observational Checklist
In pre-intervention, the majority of caregivers 86.7%, 90% and 93.3% had a poor level of drug administration, nutritional management, and care for PEG, respectively. While in the post follow up intervention, one-third (33%) of caregivers had average level related to drugs administration, and two-fifths (40%) had a good level, whereas in the follow-up, the majority (73.3%) (90%) had maintained a good level regarding nutritional management and care of PEG.
The results showed highly statistically significant differences between pre/post-test and at follow-up intervention nursing-based guidelines for caregiver's practices regarding drug administration, nutritional management, and care of PEG (f = 34.7, f =76.07, f =100.6 at p < 0.001) in Table (4).
3.4. PEG-specific Questionnaire
The current study shows that progressive patient outcome concerning physical and nutritional included post and follow-up intervention related to gastrointestinal symptoms and less than one-third (30%) had no problem while an equal percentage (26.6%) was suffering from nausea and anorexia at follow up, and post-intervention, while 16.7%, 36.6% and 23.3% had no problem, nausea, and anorexia, respectively. Regarding the gastrostomy site, more than one-third of patients (36.7%) were characterized by soft and dry site and 46.7% of them had no problems with tube troubleshooting in the follow up, at p < 0.05 as shown in Table (5).
| Items | Pre-test | Post-test | Follow-up after 3 months |
F | p-value | |||
| No. | % | No. | % | No. | % | |||
|
Drugs administration by PEG. ▪ Well level ▪ Average level ▪ Poor level |
1 3 26 |
3.3 10.0 86.7 |
8 9 13 |
26.7 30.0 43.3 |
16 11 3 |
53.3 36.7 10.0 |
34.7 |
HS 0.000 |
|
Nutritional management. ▪ Well level ▪ Average level ▪ Poor level |
0 3 27 |
0.0 10.0 90.0 |
12 11 7 |
40.0 36.7 23.3 |
22 8 0 |
73.3 26.7 0.0 |
76.07 |
HS 0.000 |
|
Care for PEG. ▪ Well level ▪ Average level ▪ Poor level |
0 2 28 |
0.0 6.7 93.3 |
12 11 7 |
40.0 36.7 23.3 |
27 2 1 |
90.0 6.7 3.3 |
100.6 |
HS 0.000 |
| Items | Post-intervention | Follow-up after 3 months |
χ2 | p-value | ||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| I. I. Patient’ health status: *Gastrointestinal symptoms ▪ Nausea ▪ Anorexia ▪ Vomiting ▪ Diarrhea ▪ Constipation ▪ Abdominal distension ▪ No problems |
11 7 1 6 4 3 5 |
36.6 23.3 3.3 20 13.3 10.0 16.7 |
8 8 0 2 4 1 9 |
26.6 26.6 0 6.6 13.3 3.3 30.0 |
2.636 | S 0.015 |
| Gastrostomy site….. ▪ Skin Infection ▪ Hypergraunlation ▪ Tenderness ▪ Soft and dry |
13 0 13 4 |
43.3 0.0 43.3 13.3 |
7 3 9 11 |
23.3 10 30 36.7 |
-2.237 | S 0.033 |
| Tube troubleshooting ▪ No problems ▪ Blockage ▪ Displacement ▪ Leakage ▪ Dislodgement ▪ Deterioration |
10 1 4 9 0 6 |
33.3 3.3 13.3 30.0 0.0 20.0 |
14 2 4 6 0 4 |
46.7 6.7 13.3 20.0 0.0 13.3 |
1.546 | NS 0.133 |
| II. Patient nutritional status | ||||||
| According to mini nutrition assessment are ▪ Normal nutritional status ▪ Risk of malnutrition ▪ Malnourished |
9 15 6 |
30.0 50.0 20.0 |
18 10 2 |
60.0 33.3 6.7 |
3.261 |
S 0.003 |
| Current bodyweight ▪ Underweight ▪ Average weight ▪ Overweight |
15 9 6 |
50.0 30.0 20.0 |
12 15 3 |
40.0 50.0 10.0 |
0.000 |
NS 1.000 |
| Items | Post-intervention | Follow-up After 3 Months |
χ2 | p-value | ||
| No. | % | No. | % | |||
| Patient/Caregiver experience: | - | - | - | - | - | - |
| Level of caregiver coping with the care of PEG ▪ Sever coping ▪ Moderate ▪ Mild coping |
7 9 14 |
23.3 30.0 46.7 |
16 9 5 |
53.3 30.0 16.7 |
3.844 |
HS 0.001 |
| Overall Patient satisfaction ▪ Satisfactory ▪ Unsatisfactory |
13 17 |
43.3 56.7 |
24 6 |
80.0 20.0 |
4.097 |
HS 0.000 |
According to a mini nutrition assessment, the two-thirds of studied patients 60% had normal nutritional status and half of them (50%) had average weight in the follow up and less than one-third (30%) of them had normal nutritional status while 50% were underweight in post-intervention period as shown in Table (5).
The results show that there was a highly statistically significant difference between post test and follow-up after 3 months regarding patients’/caregivers’ experience. The majority of the patients (80%) were overall satisfied. More than half (53.3%) of the caregivers were coping with the care of PEG at the followi up while56.7% of them were not satisfied with post-intervention and 23.3% of the caregivers were having a tough time coping with patients. In relation to the level of caregivers coping with the care of PEG, the overall patient satisfaction was observed to be (χ2 = 3.844, 4.097) p<0.001 as shown in Table (6).
4. DISCUSSION
The purpose of this study was to evaluate the effect of nursing-based guidelines on the caregivers’ knowledge and practices regarding adult patients with PEG.
The present study shows that more than two-thirds of studied patients were male with a lower financial status. This result was in accordance with the studies [19] [20], which reported that more than half of the studied group were male.
The finding of the study reported that less than half of the studied patients were illiterate and one-fifth of them obtained a primary level of education and their age was from 33-75 years. This result agrees with the reported study, which claimed that the highest number of patients who required a feeding tube placement belonged to the age group of 51-60 years [21]. Also, it is reported that the median age was 68 years [20].
Regarding the socio-demographic characteristics of the studied caregivers, the present study results showed that two-fifths of the studied caregivers were female and their age was from 20 to 29 years, while more than half of them were in high school. Also, less than half of the caregivers were sons or daughters, and less than one-quarter of them were spouses, which agreed with another study [21] that reported that 80% of caregivers were 31–64 years of age. Also, it was reported [22] that nutrition by PEG was dependant on the activity of patients and their careers. So the patients' experiences and satisfaction of living with a PEG are dependent on the educational state, age, gender, and medical diagnosis. The main caregivers for PEG patients at home were spouses.
The current study reflects the physical health and nutritional assessment of the studied patients with PEG, the majority of them were suffering from oncologic disorder. This result was not in agreement with another report [23] which claimed that the most studied patients were inserted with PEG, from the neurologic group, followed by the oncologic disorder, another diagnosis and trauma.
The present study shows that the majority of studied patients performed oral hygiene and less than two-thirds of them were taking prescribed chemotherapy treatment. This result corresponded with another study [24], which reported that tube feeding by percutaneous routes appeared to be comparably effective during chemo/radiotherapy. Also, it was reported that prophylactic PEG not only decreases adverse effects but also may potentially improve oncological outcome of the patients with oropharyngeal cancer [26].However, a report showed that patients who had chemotherapy or radiotherapy before PEG placement had a higher incidence of peristomal infections [27].
The present study shows that half of the studied patients were inserted PEG recently; this correlated with another study [25], which claimed that there is a progressive increase in the use of PEG with the meantime of treatment longer than one year.
The current study results revealed that more than two-thirds of studied patients had no problems in the pre-gastrostomy insertion site and had a clean surgical wound site and more than half of studied patients were under feeding plan. This result disagrees with another reported study [26], which claims that peristomal infection remains the most common complication following PEG tube placement, but another study states that the quality of life improves after PEG in both patients and caregivers in this series [28].
The findings of the present study showed highly statistically significant differences between pre/post and follow-up intervention regarding the caregiver’s knowledge about PEG; this finding disagrees with another study [27], which reported a barrier to gastrostomy feeding existing among Asian clinicians and their caregivers due to negative perceptions about complications and no differences in nutrition outcomes were observed between NG and gastrostomy feeding at 4 months. While agreeing with the result of another study [28], which reported that PEG is a simply invasive PEG procedure with low morbidity and mortality rates, and is easy to follow-up and replace when a blockage occurs; another study [29] reported improved understanding of the caregivers' perspectives and concerns in adults who already had or will have PEG in the future. Also, updated knowledge relating to PEG tube indications, placement, management, and care, reinforces PEG feeding as the most valuable access for patients [1].
Regarding caregivers’ practice related to nutritional management and care of PEG in follow-up, the present study showed that the majority of them had better levels. This finding disagrees with the fact that the number of patients undergoing PEG has increased, so the guidelines may help in the improvement of PEG-related care, nutritional management, and relocation of medical resources [32].
The findings of the present study showed that there were highly statistically significant differences between caregivers’ practice about PEG care pre/post- and follow up guidelines’ intervention. These results are in conformity with the reported study [22], which showed that comprehensive and practical discharge training, and home care and counseling services should be provided to effectively address the challenges faced by caregivers of patients with PEG. So, to avoid complications of PEG, the caregivers must be careful with their experiences and practices.
The present study showed that the general patient outcome concerning physical, nutritional and patient/caregiver experience in post and follow-up guidelines improved. This finding agrees with another study [1], which reported that health education provides safety of PEG feeding after placement, thus resulting in lower costs and appropriate nursing care by healthcare professionals, and patients/caregivers to prevent complications. Another study [30] claimed that according to the patients/caregivers who reflected their experiences of PEG tube feeding, including constructive cognitive appraisal, they focused on positive adaptation and acceptance of PEG feeding.
The present study shows patients’ progressive outcomes concerning physical and nutritional state post and follow-up intervention about gastrointestinal symptoms. The result shows that less than one-third of the patients had no problem while one quarter of patients were suffering from nausea and anorexia at follow up. These results are in agreement with another study [31], which confirms that long-term enteral feeding via PEG is a safe, functional, easy-to-apply, and highly suitable method with excellent long-term outcomes and minimal troubles.
The current study shows that there were no statistically significant differences between post and follow-up intervention of nursing-based guidelines regarding tube troubleshooting for patients with a PEG; these results are in agreement with another study [32], which reported the development of many complications such as dislodgement, outflow, and infection. An infected stoma is an important complication and PEG stoma infection can compromise patients’ quality of life and impact morbidity. It is important that the patient is monitored adequately to assess for early signs of potential complications to ensure timely medical attention and good clinical outcomes.
The findings of the present study highlight the importance of regular nutrition by mini nutrition assessment. The two-thirds of the studied patients had normal nutritional status and half of them had average weight at follow-up. This result agrees with the reported study that the patients’ nutritional status and conditions should be screened to minimize malnutrition in hospitalized patients to decrease complications after PEG tube placement, including undernourishment and many organic disorders [1].
The finding of this study shows that there is a highly statistically significant difference between post and follow-up intervention regarding patients’ outcomes concerning the physical and nutritional state. Another study [33] reported that the complications of PEG are few but produce side effects in these elderly patients with multiple co-morbidities, as such, patients considered for PEG feeding should have reasonable prognosis and the procedure is inappropriate for patients with worst health condition.
The current study results revealed that the majority of the studied patients were overall satisfactory and more than half of the caregivers were had difficulty coping with the care of PEG and during follow-up, there was a statistically significant number of caregivers coping with the care of PEG with overall patient satisfaction between post and follow-up intervention. This finding agrees with the study [13], where the majority of caregivers and patients felt that PEG-tube helped in feeding and prolonging survival. Also, it was reported that the primary outcome is based on the caregiver’s self-efficacy for improving the patient management.
It is the opinion of the researcher that one of the responsibilities of nurses toward patient/ family care is to educate them through program, guidelines, purchases, or patient/family classes to increase the quality of patient care especially oncology patients [34]. Additional research is needed to safely guide PEG monitoring, management, and patient/family education. Nurses administering PEG play a critical role in the early identification and management reactions; and the management programs are important to ensure consistent delivery of best-practice education and care [35]. The nurses play an essential role in providing patient-focused health information to the family. Also, according to a study [36], the reason behind inappropriate care towards PEG feeding is explained by the lack of education, knowledge, teamwork, communication, and financial support.
CONCLUSION
The general patient outcomes concerning physical, nutritional state and patient/caregiver experience of post and follow-up guidelines intervention improved. The findings of the present study showed that there were highly statistically significant differences between the caregiver’s knowledge and practice about PEG care pre/post and follow up guidelines intervention,
RECOMMENDATION
Health care professionals should be aware that caregiver education is an integral part of patient care with PEG. Continuous training and educational programs must be designed for caregivers to get updated knowledge about practices regarding the care of patients with PEG. Using research findings, the policies, procedures, and practical guidelines for the patients’ caregivers should be developed.
ADMINISTRATIVE AND ETHICAL CONSIDERATION OF THE STUDY
Official permission was obtained from the Director of the intended hospital in which the study was conducted and the heads of the departments. Meeting and discussions were held between the researchers and nursing administrative personnel to make them aware of the aims of the study. The aim of the research was also clarified to the participants. Verbal consent was obtained from each patient and caregivers to participate in the study, after clarifying the procedures of the study. Participants were informed about their right to refuse participation and withdraw at any time without any significance. The privacy of data was ensured.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has approved from Ethical Committee of Scientific Research, Ain Shams University Faculty of Medicine, Egypt.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
AVAILABILITY OF DATA AND MATERIALS
The data sets analyzed during the current study are available from the corresponding author [E.S] upon request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to acknowledge all nurses, nursing managers and management groups and organizations for giving the research team support, which helped the researchers in data collection but were not involved in the study design, analysis, and interpretation of data and writing of the manuscript.


